Management of Trauma-induced External Root Cervical Resorption and Discolouration of the Maxillary Central Incisors: A Case Report with a Four-year Follow-up
Abstract
Background:
Clinicians often face a dilemma when determining the cause of a patient's tooth discolouration and how to treat it concurrently in the presence of trauma-induced external root cervical resorption.
Objective:
This case report describes the management of trauma-induced cervical resorption and discolouration of the maxillary central incisors with a four-year follow-up.
Case Report:
A 38-year-old gentleman requested that the shape and colour of his anterior teeth be restored. The patient had a history of a motorcycle accident 15 years ago, in 2003, that resulted in fractures in both maxillary central incisors. Clinical examination showed the presence of discoloured broken teeth 11 and 21, as well as a cervical defect in tooth 11 palatally. Upon radiographic examination, 11 and 21 were root canal treated, and there was cervical resorption related to 11. Treatment consisted of cervical resorption management, internal and external bleaching, and composite restoration of the maxillary central incisors.
After a four-year follow-up, this report demonstrated the successful management of a complicated case involving trauma induced resorption and discolouration. The patient expressed satisfaction with the conservative strategy that was taken to treat his discoloured teeth.
Conclusion:
This clinical report, with a long follow-up record, helps to provide dental practitioners with a conservative, minimally invasive, patient-centred treatment alternative for a complicated tooth discoloration case.
1. INTRODUCTION
The appearance of our teeth plays a crucial role in our overall aesthetic appeal. It's common to think that discoloured anterior teeth are unattractive. This can lead to self-consciousness and affect an individual's confidence and social interactions. It is important to consider the patient's overall dental health, the extent of the discolouration, the presence of dental complicating factors, and the aesthetic goals when determining the most appropriate treatment option [1]. The bleaching of nonvital teeth has grown in significance in recent years due to the increased demand for beautiful and whiter teeth. The whitening of nonvital teeth is a minimally invasive procedure that, if performed properly, carries only minimal risks [2]. There are several treatment options available to restore the colour of the anterior teeth, each with its own advantages and limitations.
The presence of external root cervical resorption (ERCR) together with tooth discolouration presents a clinical dilemma. ERCR refers to the loss of tooth structure due to the activity of cells that break down and resorb the root surface of a tooth from the outside [3]. In the research that has been done on ERCR, numerous techniques, both surgical and non-invasive have been recommended. Despite the surgical method of lesion exposure and management being the conventional and successful management pathway, several intraoral non-surgical non-pharmacological adjunctive treatments such as low-intensity pulsed ultrasound (LIPUS), low-level laser therapy (LLLT), and photobiomodulation (PBM) [light-emitting devices (LED)] were recently explored in preventing or reducing root resorption lesions [4, 5].
ERCR is a pathological process and may be induced by internal bleaching [3], according to clinical reports [6-8] and histological studies [9, 10]. The ERCR mechanism is not completely understood. However, this is thought to be the consequence of bleaching material passing through the dentinal tubules and cemental defects, leading to the death of the cementum and an inflammatory reaction in the periodontal ligament, ultimately leading to ERCR [11]. Nevertheless, no cases of ERCR have been documented with lower concentrations of carbamide peroxide [2]. This clinical report describes the surgical management of trauma-induced ERCR and the management of discolouration by using internal and external bleaching using a low concentration of carbamide peroxide with a four-year follow-up.
2. CASE REPORT
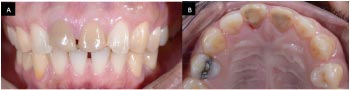
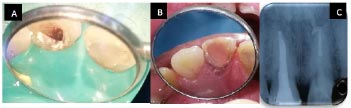
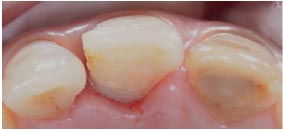
A 38-year-old gentleman came with a request to restore the shape and colour of his maxillary central incisors. The patient had a history of a motorcycle accident 15 years ago, in 2003, that resulted in fractures in both maxillary central incisors. After 15 years and 4 months, there has been a discolouration of his anterior teeth, and the teeth have become darker over time. Root canal treatment (RCT) was done for teeth 11 and 21 six years ago in 2012. Medically, no other systemic complications were declared or detected. The patient was healthy with no history of smoking. Clinical examination revealed the presence of discoloured broken 11 and 21 (Fig. 1). The patient has a high lip line showing fully maxillary central incisors (Fig. 2). No active pain or infection was reported at the time of the examination. A rough cervical margin was detected near the gingiva at 11 palatally (Fig. 3). This aspect was clinically visible and confirmed with an intraoral periapical radiograph (IOPA) and cone-beam computed tomography (CBCT).


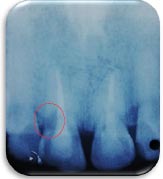
An IOPA radiograph was taken in 2018, and it was found that the periapical area of 11 and 21 was considered healthy with no signs of a lesion. The cervical resorption site of 11 was extended vertically from the cementoenamel junction (CEJ), reaching the middle third of the root (Fig. 4). This finding gave us the justification to take CBCT to study the area of defect further and evaluate the extension and size of the defect.
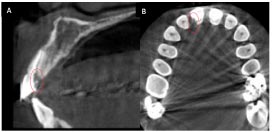
In the CBCT, communication between the root canal space and the periodontal ligament (PDL) space occurs through the defect from the CEJ to about 5 mm down to the root’s middle third. The cervical defect was on the disto-palatal root surface of the tooth and measured approximately 2.5 mm by 5 mm (Fig. 5). The diagnosis was confirmed, which is trauma-induced external root cervical resorption (TIERCR) of Class 3 [12]. The cause of discolouration can be due to trauma, improper endodontic treatment, endodontic material used in the treatment, etc.
After presenting the problem list and the possible treatment options to the patient, there was a discussion about the advantages and disadvantages of every option, especially the risk of root resorption, and he accepted and consented to the proposed treatment plan. Patient management was conducted in compliance with CARE case report guidelines and the Declaration of Helsinki.
For the TIERCR of 11, different treatment options were discussed with the patient, such as monitor only, orthodontic extrusion and restoration of the defect; surgical exposure of the site and defect restoration; or extraction and replacement with either a fixed bridge or implant. The patient agreed to both surgical management and defect restoration. For the discolouration of 11 and 21, different treatment options were discussed with the patient, such as internal bleaching only; external (in office or at home) bleaching only; inside-outside bleaching or external/internal bleaching; direct composite restoration; veneers; or an indirect restoration. The patient requested and consented to the non-invasive treatment, which is internal and external bleaching, and emphasised his desire to preserve the teeth and avoid tooth structure removal.
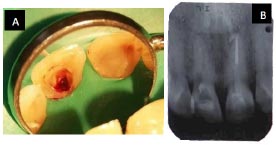
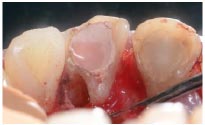
The management of TIERCR started with endodontic retreatment under the microscope to achieve a 3D hermetic seal before the surgical management. After removal of the old gutta-percha (GP) (Fig. 6), 11 was obturated with GP by using the lateral condensation technique and AH26 resin-based root canal sealer (Dentsply, Germany) (Fig. 7).
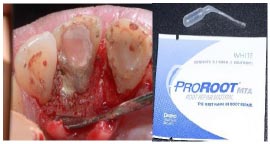
One day after the obturation, the surgical management began. The surgical site was anaesthetised by giving a labial infiltration injection using 2 percent Scandonest (Septodont, USA) with adrenaline (1:80,000). A sulcular incision was made from the palatal mesial aspect of 22 to the distal aspect of 12. A full-thickness mucoperiosteal flap was raised to expose the root surface of 11 (Fig. 8). A defect was discovered on the disto-palatal root surface of 11 that extended 5 mm apical to the CEJ (Fig. 9). Electrocautery and hand instruments were used to clean the defect site of invading tissue. The defect site was shaped by a round bur fitted into a Satelec ultrasonic device (P5 Newtron® XS-Acteon) (Fig. 10). The defect site was cleaned by rinsing with normal saline and then filled with ProRoot MTA (Dentsply, USA) (Fig. 11).


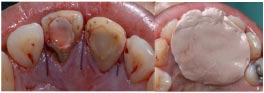
The flap was repositioned and sutured with Dafilon 4-0 non-absorbable suture (Aesculap, USA), and a periodontal pack (COE-PAK, GC) was placed over the surgical site (Fig. 12). The patient was given post-surgical instructions. After seven days and one month following surgery, the patient was recalled and reviewed, and sutures were removed (Fig. 13). An IOPA radiograph was taken to ensure the defect was adequately restored (Fig. 14). The MTA was capped with glass ionomer cement (Fuji IX GC, Japan) first and then composite on later visits (Filtek Z350, 3M ESPE, USA) (Fig. 15).


Three months following the surgical root restoration, the internal and external bleaching processes were started. Prior to starting the whitening procedure, the shade of 11 was C4, while 21’s shade was A4 (Fig. 16). Firstly, the non-vital bleaching (walking or internal bleaching) of 11 was started. The access opening restoration was removed, and the gutta-percha was reduced up to 2–3 mm below the CEJ. This created space was restored with glass ionomer cement (Fuji IX, GC, Japan) to seal the canal orifice. The pulp chamber was filled with 15% carbamide peroxide (Opalescence PF 15%, Ultradent Inc., USA) (Fig. 17). The cavity was sealed provisionally with glass ionomer cement (Fuji VII, GC, Japan). The patient was recalled after 10 days, and the bleaching process was repeated. The results and shade change of each visit were evaluated with the Vita-pan classical shade guide, spectrophotometer (Vita Easyshade®, Vita-Zhanfabrik, Bad Säckingen, Germany) and photography to determine the effectiveness of the treatment and whether additional bleaching applications were needed. After one month and three visits, the shade of 11 was lighter than C4 and became A3.

After the internal bleaching, the external (at home) bleaching of 11 and 21 was initiated. A maxillary impression was made with alginate (Kromopan®, Lascod, Italy). The impression was sent to the laboratory to construct a thermoplastic bleaching tray of 1 mm thickness, scalloped for only two teeth. In contrast, the other anterior teeth have no labial coverage by the tray (Fig. 18).

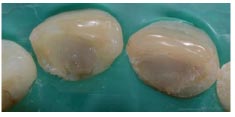
One tube of Opalescence PF 10% (Ultradent, USA) (carbamide peroxide) was given to the patient. The tray was fitted over the maxillary arch and checked for fit and for any possible trauma to the gingiva. The patient accepted the tray, and instructions were given to him on how to use the tray and the material. The original shade of 11 was C4, while the 21’s shade was A4 (Fig. 16). After one month’s review, 21’s shade became B4, and 11’s shade became A2 (Fig. 19). The bleaching was continued for only 21 as the patient was instructed not to put a bleaching agent over 11. After another month, 21 was bleached and became an A3 shade. The shade of the old composite stayed the same, and it was planned to change to a new one after two weeks. After two weeks, shades 11 and 21 were evaluated again, and the teeth were restored with composites of shades A3, A2, and AE (G-aenial Anterior, GC, Australia). The patient was satisfied with the results and was thankful for conserving the teeth (Fig. 20).



After a series of follow-up appointments, The last one was after 4 years, the status of 11 was stable, and there were no signs of resorption, disease, or washout of the MTA. The teeth were stable in colour, with no discolouration noted. An IOPA radiograph was taken, and simple polishing of the composite restoration and full mouth prophylaxis were done (Fig. 21).
3. DISCUSSION
The patient's main concern was the unsightly colour of his upper anterior tooth. Following history taking and examination, the patient's past dental records were reviewed. The patient had a history of a motorcycle accident 15 years ago in 2003 that resulted in fractures and discolouration in both maxillary central incisors. According to [13], ERCR seems to be caused by multiple causes in the majority of cases, with at least two and often as many as three factors being found in each case. The predisposing factors for the resorption process include trauma, periodontal therapy, internal bleaching agents, etc [3, 13]. Trauma was the second-most prevalent factor that was found to induce ERCR, accounting for 28.5% of cases when combined with other factors and roughly 12% of cases when trauma was the only factor [13]. The presence of a defect on the root surface in the labio-lingual direction cannot be detected using conventional radiography due to its two-dimensional nature; hence, cone-beam computed tomography (CBCT) was done, and the presence of cervical root resorption on the disto-palatal root surface of tooth 11 was confirmed. CBCT is a three-dimensional imaging technique that has various applications in endodontics, including the detection of external resorption that may not be visible on conventional radiographs [14, 15].
In the research that has been done on ERCR, numerous techniques, both surgical and non-invasive have been recommended. Several intraoral, non-surgical, non-pharmacological adjunctive treatments such as LIPUS, LLLT, and PBM (LED) have recently been investigated for their ability to prevent or reduce root resorption lesions [4, 5]. The majority of research on these therapies focused on orthodontics and root resorption. These therapies may act via a single or several complicated mechanisms. It may have a preventative benefit by protecting the outer cementum layer through accelerated bone remodelling, or it may encourage the remodelling of root dentin and the cementum in order to treat root injury. However, the effects of the above-mentioned interventions on orthodontic root resorption are still controversial [4, 5] and require more research and trials on traumatised teeth in order to expand their clinical application.
Surgical procedures can involve an open flap surgery that allows access to the defect so that the resorbing tissue can be removed, followed by the application of MTA and/or glass ionomer cement. The removal of the resorptive tissue is performed by using nonsurgical methods, often either mechanical (ultrasonic) or chemical (tetraacetic acid) means [12]. A new technique was proposed using antimicrobial photodynamic therapy as an adjunctive therapy during root canal retreatment [16]. This case was managed by surgical exposure of the lesion, resorptive lesion removal through electrocautery, cavity preparation by ultrasonic means, and restoration by using MTA.
Surgical repair of root resorption is indicated when the perforation is inaccessible non-surgically; there has been a failure of healing after non-surgical repair; a post and crown are cemented in place; or an extensive coronal restoration is present [17]. Following endodontic retreatment and one day after the obturation of tooth 11, surgical repair was initiated with periodontal flap reflection, curettage of the resorptive tissue by excavation, and electrocautery. No tetraacetic acid was applied as this material was not available. The cavity was prepared with ultrasonic to create a smooth margin. The defect cavity was restored with MTA (mineral trioxide aggregate) material, and the flap was closed and sutured [12, 18]. MTA was chosen to seal the defect in this case because of its excellent biocompatibility and good sealing ability. There are several shortcomings of MTA, including its relatively long setting time and difficult handling properties [19, 20]. Biodentine is another material that can be considered to avoid the difficult handling of MTA. However, evidence of a long-term positive outcome supports the application of MTA for the treatment of root perforation originating from internal or external resorption [21].
After the perforation had been repaired by an open flap surgery and complete healing of the soft tissues had been observed, internal bleaching of tooth 11 was done in order to lighten the colour of the tooth, combined with external bleaching of teeth 11 and 21. Gutta-percha was removed up to 2 mm below the CEJ, and glass ionomer cement was placed to seal the canal orifice and serve as an effective barrier to prevent the leaching of the bleaching agent into the periapical and cervical areas and thus prevent root resorption. The bleaching tray was adjusted to cover only teeth 11 and 21 labially, and the patient was instructed on how and when he should apply the bleaching agent [1, 22]. For the colour change assessment, the Vita-pan classical shade guide, spectrophotometer (Vita Easyshade®, Vita-Zhanfabrik, Bad Säckingen, Germany) and photography were used to assess the teeth shades [22-24]. After the desired tooth colour was achieved, direct composite restorations were deferred for two weeks. This was necessary as it has been shown that the bond strength of composite to bleached enamel and dentine is temporarily reduced; hence, it is recommended to wait at least two to three weeks post-bleaching and prior to bonding composite [1]. Findings of a systematic review generally indicate the good clinical performance of composites in the long-term (follow-up 3+ years) for anterior composite resin restorations, with annual failure rates varying from 0 to 4.1% [25].
There is no contraindication to doing internal and/or external bleaching in teeth; however, there is a risk of ERCR if several risk factors are present, such as the use of hydrogen peroxide concentrations greater than 30%; the application of heat; a history of trauma; orthodontic treatment; the presence of bacteria; and the lack of a barrier over the gutta-percha to protect the odontoblasts and dentinal tubules close to the cervical dentine [2]. The same authors suggested delayed bleaching after trauma to avoid ERCR [2]. The ERCR mechanism is not completely understood. However, this is thought to be the consequence of bleaching material passing through the dentinal tubules and cemental defects, leading to the death of the cementum and an inflammatory reaction in the PDL, ultimately leading to ERCR [11]. No cases of ERCR have been documented with lower concentrations of carbamide peroxide or hydrogen peroxide [2]. In another recent study, there was very little evidence relating to the risks of external cervical resorption with modern internal bleaching protocols [26].
Furthermore, according to the authors' knowledge, no clinical reports were found to show the results of bleaching a tooth associated with TIERCR with long follow-up. After 4 years and at the follow-up visit, the outcomes were satisfactory with no signs of failure, and the patient was grateful for the result.
CONCLUSION
The discolouration of the anterior teeth is an aesthetic dilemma. Management can be complicated and require further follow-up if the discolouration is associated with ERCR and a previous history of trauma, but with an accurate diagnosis, thorough treatment planning, and suitable treatment practices, a predictable outcome is possible. For individuals presenting with tooth discolouration, the ability to provide treatment with minimal adverse consequences continues to be the preferred treatment option.
AUTHORS’ CONTRIBUTION
MA contributed to the conceptualization of the study and collection of the material, did the treatment procedures, designed the graphical part of the manuscript, and wrote the manuscript; AIA and WAFWJ wrote the manuscript. AN did the treatment procedures and TYN took part in the conceptualization of the study. HAG took part in the conceptualization of the study and provided her final approval for the version of the manuscript to be published.
LIST OF ABBREVIATIONS
| ERCR | = External Root Cervical Resorptio |
| LIPUS | = Low-intensity Pulsed Ultrasound |
| LLLT | = Low-level Laser Therapy |
| PBM | = Photobiomodulation |
| LED | = Light-emitting Devices |
| RCT | = Root Canal Treatment |
| CBCT | = Cone-beam Computed Tomography |
| CEJ | = Cementoenamel Junction |
| PDL | = Periodontal Ligament |
| TIERCR | = Trauma Induced External Root Cervical Resorption |
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
The participant involved in this study provided his written informed consent.
AVAILABILITY OF DATA AND MATERIAL
All the data and supporting information are provided within the article.
FUNDING
Special thanks to Universiti Sains Malaysia for the financial assistance through the Short Term Grant (304/PPSG/6315680).
ACKNOWLEDGEMENTS
The authors are thankful for all the efforts made by the dental assistants and laboratory technicians.


