Digital Full-mouth Rehabilitation for Complex Cases Involving Severe Deep Overbite and Worn Dentition: A Case Report
Abstract
Introduction:
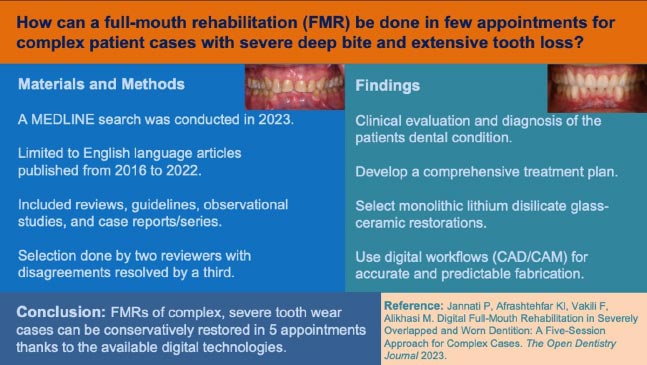
The demand for aesthetic restorations in dentistry has led to full-mouth reconstructions or rehabilitations (FMRs) as a viable solution for treating patients with worn and altered teeth. This study presents a clinical case report of a middle-aged patient with severe tooth wear and deep overbite with digital workflows.
Case Presentation:
The case report highlighted the successful application of digital technology in the comprehensive rehabilitation of a patient with worn dentition, showcasing improved esthetics, function, and patient comfort. The case report demonstrated the potential benefits of this rapid approach in achieving successful outcomes. Digital CAD/CAM technology is a solution for optimizing the prosthetic workflow, achieving time and cost efficiency, and delivering high-quality dental restorations.
Conclusion:
Future primary studies with larger sample sizes and longer follow-ups can further validate the FMR digital approaches.
1. INTRODUCTION
Tooth wear is a phenomenon characterized by tooth surface loss (TSL) without bacterial infection and can have either physiological or pathological origins [1]. While physiological tooth wear occurs gradually with age, pathological wear, such as attrition, abrasion, abfraction, and erosion, is often multi-factorial in nature and can be challenging to isolate a single etiological factor in clinical presentations of worn dentition [2-4]. The term 'tooth surface loss' was proposed by Eccles in 1982 to encompass all causes of wear regardless of their identification [2-4]. Severe tooth wear can result in both esthetic and functional problems, including decreased vertical dimension of occlusion (VDO) [5]. The management of worn dentition can range from preventive and localized treatments to full-mouth rehabilitation (FMR) based on the severity of the condition [6]. FMR presents a significant challenge for dental practitioners, requiring a reliable and predictable workflow. Integrating computer-aided design/computer-assisted manufacture (CAD/ CAM) technology, advanced ceramic materials, and adhesive cementation offers a reliable approach to FMR [7, 8]. Conventional FMR techniques are often time-consuming, requiring numerous clinical appointments and laboratory procedures, with the risk of errors in each step potentially necessitating repeat treatment. Digital advances in intraoral scanners (IoS) and laboratory scanning, as well as intuitive software design, have greatly improved the speed and accuracy of CAD/CAM fabrication processes.
The use of virtual on-screen designing and CAM with rapid prototyping options such as milling (s-CAM) or printing (a-CAM) allows for the efficient production of various restorations without physical models. The utilization of CAD/CAM technology enhances the predictability and reliability of FMR while reducing treatment duration and appointments/steps [9]. This clinical report outlines the application of a digital approach in a full-mouth rehabilitation procedure for a patient with severe deep bite occlusion and extensive tooth surface loss.
2. CLINICAL CASE REPORT
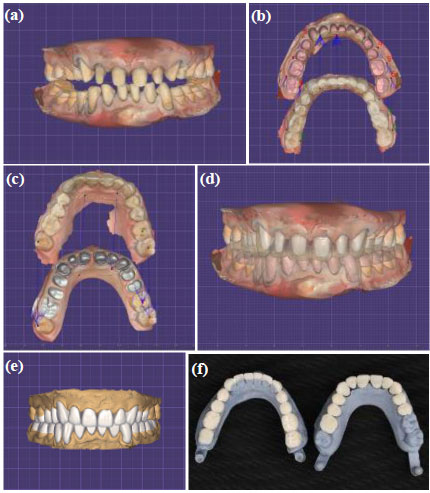
A 45-year-old male patient was referred to the Prosthodontics Department at the Dental College to treat his worn dentition. The patient presented with chief complaints of tooth surface loss (TSL), reduced chewing ability, and mild esthetic concerns, particularly regarding shade. The medical history was unremarkable, with no indications of temporomandibular joint disorder (TMD), except for excessive consumption of lemon and vinegar related to a pre-diabetes condition. Intraoral examination revealed a two-surface amalgam filling on the left second molar and composite resin fillings on the right first premolar, right second premolar, and right first molar. Abfraction was observed in several teeth of varying severity, with mild abfraction in all posterior teeth except for the right first and second molars, which showed moderate abfraction. The patient's occlusion was classified as Class II division 2 with a deep bite. All teeth displayed worn incisal/occlusal surfaces, exposing dentin in the maxillary central incisors, and limited to enamel in the maxillary premolars and most areas of the mandibular premolars (Fig. 1). The extraoral examination showed a square, symmetrical face, a slightly shorter lower third, and competent lips. The pattern of worn dentition did not match the opposing teeth, indicating that the cause of TSL was not solely due to parafunctional habits but may also have been a result of a chronic erosion progression exacerbated by job-related stress.

The incisal level of the mandibular anterior teeth was adjusted using a flowable composite (G-aenial, GC, Tokyo, Japan), where the reference was the lip level (Fig. 2A). To analyze vertical dimension, phonetics, facial profile, and interocclusal space were evaluated. The vertical dimension of rest (VDR) was approximately 5 mm from the VDO. Lucia jig was made (GC Resin Pattern, GC, Japan). After several minutes and deprogramming of the muscles, the centric relation (CR) was recorded by injecting posterior bite registration (Granit, Mueller Omicron Dental, Lindlar, Germany) in the newly defined vertical dimension (VDR – VDO = 2). The first impressions were made using one-step putty/light-body silicon impression material (Speedex, Coltene, Altstätten, Switzerland), which served as a diagnostic cast. The ear-bow (Spring-bow Hanau earpiece facebow, WhipMixCorp, Kentucky, United States) record was determined for mounting on the Hanau semi-adjustable arcon articulator (Hanau Wide-Vue Arcon 183-2, WhipMixCorp, Kentucky).
Based on the earbow record, the maxillary cast was mounted on the articulator (Hanau Wide-Vue Arcon 183-2, WhipMix Corp, Kentucky, United States). Then, the mandibular cast was mounted against the maxillary cast using the jig and the CR record (Fig. 2B). The Broadrick flag was used to estimate the posterior plane on each side. The wax-up procedure was done based on the defined occlusal plane, and the putty index (Speedex, Coltene, Switzerland) was prepared intraorally for the mockup process.

The mockup was made with a bis-acrylic composite-based temporary material (Teco, Tecodental, New York). Face profile, smile, phonetics, and freeway space were examined after occlusal equilibration and adjustments, and minor esthetic modifications were made. Based on the mockup, the treatment planning was designed (full-coverage crowns: teeth #6, 7, 8, 9, 10, 11, and 28; laminate veneers: teeth #22, 23, 24, 25, 26, and 27; vonlay: teeth #4, 5, 12, and 13; overlay: teeth #3, 18, 19, 20, 21, 28, 29, and 30). Teeth #2, 14, and 15 were excluded from the treatment planning and were left intact since they provided stable holding contacts after a slight enameloplasty. Due to the presence of generalized TSL and the need to restore most posterior teeth to cover exposed dentin areas, establish stable occlusal contacts, create appropriate buffer space, and correct the deep curve of Spee, we were advised against utilizing the Dahl appliance. Despite being recognized as one of the most conservative approaches in full-mouth rehabilitation (FMR), its application was cautioned against in this particular case [10]. The mockup was removed from the patient’s mouth after he approved it, followed by finishing and polishing with discs (3M Sof-Lex, 3M, Minnesota, US). A flowable composite (G-aenial, GC, Tokyo, Japan) was used for cementing them as a temporary restoration for follow-up newly established VDO. Then, the patient's condition was assessed regarding the temporomandibular joint (TMJ) and muscle comfort, phonetics, chewing ability, and esthetics for four weeks.
The mockup of each jaw and the occlusion were scanned. The putty index was determined for tooth preparation. The anterior temporary restorations were removed. The maxillary and mandibular anterior tooth preparations were performed using a round-end cylindrical bur (Jota, Rüthi, Switzerland) based on the putty index. The occlusal clearance was assessed considering the posterior temporary restorations. After completing the anterior preparation, a new anterior jig was made as the anterior stop, maintaining the VDO. Retraction cords #00 (EasyCord, Mueller Omicron Dental, Lindlar, Germany) were used for gingival retraction for the crowns’ and at the gingival vonlays’ finish-line preparations. Both prepared arches and occlusion with the anterior jig were scanned with IoS (Medit i500, MEDIT Corp., Seoul, South Korea) (Fig. 3A).
The STL (Standard Tessellation Language) and PLY format (Polygon File Format) files were extracted and sent to the laboratory. The finish lines were determined. Then, the mockup, occlusion, and preparation STL files were superimposed on the corresponding prepared arch (Figs. 3B, 3C and 3D). These data were used to assess the final smile line using digital smile design (DSD) software (Digital smile design, Madrid, Spain). The restorations’ shape and occlusal/incisal level were estimated and used for designing resin patterns (Detax, Ettlingen, Germany). Finally, resin patterns and Geller casts (Longer blue modeling resin, Longer3d, China) were printed (a-CAM) (Asiga, Sydney, Australia) (Figs. 3E and 3F).
Resin patterns were assessed intraorally. After verifying the adaptation and proximal contacts, occlusion adjustment was made in eccentric and centric movements. Face profile, smile line, phonetics, and freeway space were examined, and minor esthetic modifications were made with the patient’s approval. Resins were sent to the laboratory to fabricate injectable resin patterns (Resione c01 transparent castable dental resin, Resione, Guangdong, China) and accomplish the heat-press process (Programate p3010, Ivoclar, Vaduz, Lichtenstein). The contouring process and staining (Ivoclar, Lichtenstein) on the Geller cast were done.

Pressed monolithic lithium disilicate glass-ceramic (Ivoclar, Lichtenstein) with a staining technique was chosen for all restorations. The A1 shade (VITA) was selected after consulting with the patient in standard light conditions and considering patient’s skin color and age. Based on the patient's history and considering the comparative durability of dental ceramics, we decided against using direct composite resin, despite some studies advocating it as a conservative technique [11, 12].

After assessing the restorations' adaptation, adjusting the proximal and occlusal contacts, and confirming the form and shade with the patient, the adjusted areas for restorations were finished and polished, and the cementation process started. The ceramics surface treatment was done with 20s hydrofluoric acid 5% (Porcelain Etchant, Bisco Schaumburg, IL, USA), 30s phosphoric acid 37%, (Etch-37, Bisco Schaumburg, IL, USA), and silane (Bis-Silane, Bisco Schaumburg, IL, USA), respectively. Under isolation with a rubber dam (Nic Ton, Bucharest, Hungary), surface treatment of the prepared tooth was done with pumice powder (Kemdent, Swidon, United Kingdom), Al2O3 air-abrasion (Parkell, New York) (5s, 10mm, on exposed dentin), 20s phosphoric acid 37% (on enamel), 5th generation bonding (All-Bond3, Bisco Schaumburg, IL, USA), and 6th generation dentine bonding agent (Clearfil SE BOND, Kuraray, Tokyo, Japan), respectively, for teeth with dominant enamel and dominant dentin. Considering the restoration thickness, the light-cure cement (Choise2 Trans, Bisco Schaumburg, IL, USA) was selected in the esthetic areas. A dual-cure cement (Duo-Link Universal, Bisco Schaumburg, IL, USA) was selected where the restorations were thicker (Figs. 4 and 5). The STL file of final restorations was used for stabilization appliance fabrication with clear resin (Detax, Ettlingen, Germany) and 3D printer (Asiga, Sydney, Australia) since there was no need to adjust the maxillary restoration during the occlusal equilibration.
3. DISCUSSION
This case report focused on the treatment procedure of a patient who suffered from pathologic deep overbite (i.e., vertical overlap) and TSL in 5 appointments. Due to the presence of CAD/CAM technology for the clinician and technician, these cases can be treated in fewer sessions with more precise and predictive occlusion and esthetics [2, 13]. Patient’s comfort, ease of making and restoring working casts, even Geller casts, superimposing details of confirmed mockup on prepared teeth, transferring the new determined VDO from mockup to final restorations precisely with minimum occlusal adjustments, facilities the treatment procedure and results in fewer clinical and laboratory steps.
Obtaining esthetics in a monolithic restoration requires an experienced technician for detailed staining. The final shade and translucency of ceramic restorations can be significantly influenced by the type of material, cement, and substrate. In the present case, there was no discoloration in patient’s teeth and a satisfying and vital final shade was obtained using translucent cement under monolithic restoration. From the perspective of color stability, lithium disilicate is less susceptible [14-17]. By this pathway, omitting porcelain layering steps and multiple and miscellaneous clinical try-in appointments, besides the optimal performance of monolithic restorations in an oral cavity environment, make way for quick treatment procedure (Fig. 6). Digital technology can reduce treatment errors by increasing the accuracy and predictability of treatment steps which lead to saving time [18-21]. Overall, digital CAD/CAM technology presents a promising solution for optimizing the prosthetic workflow, achieving time and cost efficiency, and delivering high-quality dental restorations.
CONCLUSION
The implementation of digital technology enables fast, conservative, and accurate restoration fabrication, yielding promising results. The present work demonstrates that utilizing a full arch digital workflow for designing and fabricating monolithic lithium disilicate glass-ceramic restorations is an effective treatment option for resolving severe deep overbite and tooth surface loss (Fig. 6).
LIST OF ABBREVIATIONS
| FMRs | = Full-Mouth Reconstructions or Rehabilitations |
| TSL | = Tooth Surface Loss |
| VDO | = Vertical Dimension of Occlusion |
| CAD/CAM | = Computer-aided Design / Computer-assisted Manufacture |
| IoS | = Intraoral Scanner |
| TMD | = Temporomandibular Joint Disorder |
| CR | = Centric Relation |
AVAILABILITY OF DATA AND MATERIALS
The data that support the discussion of this work are available from the corresponding authors, [M.A. and K.I.A.], upon reasonable request.
ACKNOWLEDGEMENTS
Declared none.


