A Preventive Strategy against Root Caries for the General Dentist: A Cross-sectional Clinical Study
Abstract
Objective:
The purpose of this study was to look into the prevalence of root caries and gingival problems among patients attending a teaching dental hospital in the Sultanate of Oman, as well as to assess patients' knowledge and attitudes toward oral health and to develop a “prototype” preventive plan against root caries for general practice.
Methods:
A cross-sectional clinical study of patients attending patient clinics for routine procedures was conducted. For each patient examined, the participating clinical faculty members were to complete a two-part survey: a root surface chart and a periodontal chart. A questionnaire that sought to assess patients’ knowledge and attitudes was also conducted.
Results:
There was a high prevalence of gingival recession and root caries in the study population, which indicates that root caries are already a dental management issue. Patients who reported a family history of diabetes had significantly more root surface active lesions and were three times more likely to have a lesion compared to patients who did not. Despite their lack of knowledge about dental diseases and what would happen to their oral tissues as they aged, the majority of patients in this study are concerned about future carious attacks and would prefer to receive direct advice from their dentist.
Conclusion:
There is a need for a program to educate dentists about the shortcomings of the current approach to patient education and motivation and provide them with the necessary training to implement a successful root caries prevention strategy in their practises.
1. INTRODUCTION
The main disease processes which affect the structure of the oral cavity, dental caries, and periodontal disease can all be present throughout adult life and are all preventable. In the case of dental caries, the peak incidence usually occurs during the childhood or teen years. Adults are still susceptible to caries, but the carious process may occur in different sites due to theeffects of periodontal disease and gingival recession.
As the population ages and the dentate proportion of this ageing population increases, general dental practitioners will treat increasing numbers of older adults. The expectations of these older adults will be high; they will have lived through a period of improved healthcare provision and rising standards of both medical and dental treatment [1]. One changing aspiration of this group is to retain most of their natural teeth throughout their lifetime. Given the high prevalence of root caries in older adults, there is a high demand for effective root caries preventive strategies [2].
Several factors also contribute to an increase in the number of exposed root surfaces due to early gingival recession in the younger age groups, resulting in a higher risk of root caries [3]. Gingival recession exposes the root surface and may be associated with dentine hypersensitivity, root caries, and non-carious tooth surface loss. Furthermore, the gingival recession that is left untreated tends to worsen over time as a result of apical displacement [4]. Root caries incidence and prevalence are therefore expected to be high and increasing [5], in combination with periodontal disease and gingival recession, where exposed root dentin is at risk for root caries propagation, particularly in certain individuals with suboptimal oral hygiene, impaired dexterity, and reduced salivary flow [6].
For many years, dental caries, and periodontal disease prevention's primary focus has been improving patient oral hygiene. The dentist's responsibility was to motivate the patient to use the right plaque removal technique. Today, prevention takes a broader and more holistic approach [7], with preventive interventions that target widespread contributing factors, increase community protection, and develop action plans for implementing these interventions.
While working in specialty clinics and general practising clinics, the investigators of this work became aware of a high level of gingival recession among attending patients. A surprising number of root caries lesions were also observed in regularly attending patients who were predominantly caries-free and maintained a high level of oral health. Little is known about patients’ knowledge and attitudes toward root caries and gingival recession. Whether patients are aware of the changes which occur in their oral cavities and what perceptions these patients have towards these changes and their oral health. As we work to assist dentists, patients, and the general public in improving their oral and overall health, there is also a need to evaluate how important it is for the dental public health sector to provide supplementary information, raise awareness of, and support the implementation of a preventive approach to dental care. The first successful initiative for the adoption of a more preventive approach to dental care based on the best available evidence was the 'Delivering Better Oral Health (DBOH)' document, published in 2007 by Public Health England at the request of the Department of Health to the British Association of Community Dentistry (BASCD) [8]. DBOH was intended to provide dentists with a simple guide to the evidence explaining what the research meant in practice for the adoption of the preventive strategy and treatment of their patients. The approach focuses on preventive advice for all patients while providing additional support for those at the greatest risk of poor oral health.
The purpose of this work is to first explore the prevalence of root caries and gingival problems in patients attending a teaching dental hospital in the Sultanate of Oman, then in the second part, investigate patients’ knowledge and attitudes towards root caries and gingival problems, and finally develop a “prototype” preventive strategy against root caries for the use in general practice. Data of this kind would be of great use to general dental practitioners and could be used to develop a meaningful strategy to aid in root caries prevention. This work will also illustrate several recommendations for implementation for the development of a program that is hoped to increase the awareness of dentists towards the shortcomings of the current approaches to patient education and motivation and to equip them with the necessary skills to implement a successful preventive strategy against root caries.
2. METHODS
This is a cross-sectional clinical study also collecting retrospective information by means of a survey. Ethical approval for this study was obtained from the Institutional Review Board of the dental school, adhering to the guidelines for clinical research, prior to initiating the data collection process. All adult patients attending faculty clinics and seen by the clinical research team members for routine dental appointments over the period of the data collection process (3 months) were included. To be eligible for inclusion, patients had to be over the age of 16 and under the age of 65, and they had to have not received any treatment for an acute dental condition on the day of the examination. Exclusion criteria for the study were patients who were below the age of 16 or above the age of 65 and patients who had received treatment for an acute dental condition on the day of the examination.
2.1. Part I – Cross-sectional Patient Examination
A cross-sectional study of patients attending patient clinics at Oman Dental College was conducted. Clinical faculty members (n = 12) were asked to recruit all adult patients attending their practise for routine dental appointments over a period of 3 months. Informed consent was taken from each patient. The study instrument was comprised of a survey sheet that included two dental charts and a brief checklist. A two-part survey was to be filled in by the participating clinical faculty members for each patient they examined. The survey was divided into two parts: a root surface chart and a periodontal chart. The remainder of the survey requested descriptive information about the patient: date of birth, sex, occupation, smoker or non-smoker, state of oral cleanliness, gingival condition, number of cavities, number of restored teeth, medical family history, and the name of any medication the patient was taking. The survey also contained instructions on conducting each portion of the examination.
Root surface chart - Participating clinical faculty members were instructed to examine clean, gently dried teeth with special emphasis on root surfaces. They were asked not to probe unless root caries were present and then to probe gently only to determine the texture of the lesion. Four root surfaces per tooth were examined and the condition of each surface was recorded in the chart. On examination, the teeth were given scores using an in-house coding system as the input (SCARF); (S)ound tooth surface and no recession root (C)aries present (active or arrested), (A)braded root surface (non-bacterial tooth loss), gingival (R)ecession (present/absent), and (F)illed root surfaces.
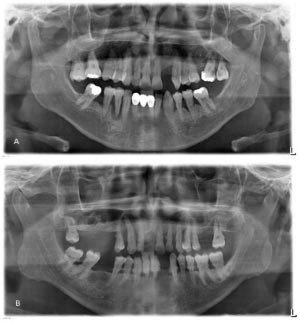
Periodontal chart - On examination, the following values were recorded in all teeth (6 locations/tooth): plaque (absent/present), bleeding on probing (absent/present), probing depth (mm), and recession (mm). A panoramic X-ray was taken in order to determine bone levels and to help determine the final periodontal diagnosis of the included patients.
The clinical charts were piloted by the authors in their own faculty practise in order to determine whether the design was usable and reasonable. The participating clinical faculty members were asked to complete the survey within a given two-month period. Considerable examiner training was given to the participating clinical faculty members on the day release day during which the study was introduced.
2.2. Part II – Cross-sectional Patient Survey
The study instrument was an online questionnaire through Google, distributed among all adult patients attending our practise for routine dental appointments using a QR code that patients scanned on their devices. The questionnaire was designed according to the principles of Lumsden [9], which sought to assess patients’ knowledge and attitudes toward root caries and gingival problems. The questionnaire pack comprised a covering letter introducing the study and a combined consent form and information sheet. The patient questionnaire was comprised of 20 questions, 16 of which were closed questions; three open questions; and 1 combined. Further comments from patients were encouraged, and an open textbox was outlined for this purpose at the end of the questionnaire (appendix).
2.3. Statistical Analysis
To present the results, we used mean values, standard deviation, frequency, and percentage data. To analyse the cross-sectional data collected and to evaluate the association of different factors with root caries, the study used logistic regression analysis and odds ratio estimates. All statistical analyses were carried out using GraphPad Prism 9 (GraphPad Software Inc.; San Diego, CA).
3. RESULTS
3.1. Part I: Cross-sectional Patient Examination
All 12 clinical faculty members completed the clinical charts, and a total of three hundred and two patients were surveyed. A demographic description of the patients was followed by data relating to the patients’ oral condition, their knowledge of dental disease, and attitudes towards their dental care.
Three hundred and two patients were clinically examined. 198 of these were male and 104 were female. The age of the patients involved in this study ranged between 16 and 64 years. Five study age groups were comprised as follows: the 16–20 years comprised 28 patients, the 21–30 years comprised 108 patients, the 31–40 years comprised 76 patients, the 41–50 years comprised 66 patients, and the 51+ group was comprised of 24 patients.
One-fifth of the examined patients were university students; another one-fifth were unemployed or retirees. Twenty-two patients (7.4%) reported that they were smokers. Two hundred fifty (82.8%) patients reported no health issues. Diabetes was reported by twenty patients (6.6%) and hypertension by eighteen (6%), among which the most common combination of conditions was hypertension and diabetes (19%). Eight (2.6%) patients reported using medications that may cause xerostomia, namely, Amlodipine, Fenofibrate, Micardis, Rocaltrol, and Valsartan.
Overall, thirty-six (12%) patients were categorized as having good oral gingival condition, one hundred ten (36.7%) as mediocre, and one hundred fifty-four (51.3%) as poor. The younger group (16-30 -year-old) had more patients categorized with good gingival condition (77.8%).
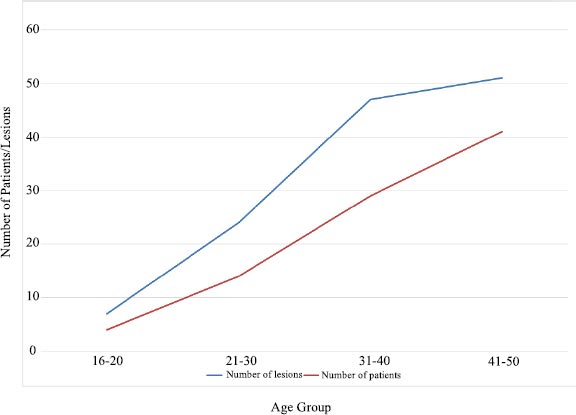
Root caries prevalence increases with age. This increase was noted in both female and male patients (Fig. 1). Almost one-third (29.8%) of all patients examined had root caries, among which 79.5% were active lesions. The most affected teeth with root caries were the maxillary second molars, followed by the maxillary premolars and the lower incisors, and the most affected surface was the buccal, followed by the lingual.
Interestingly, of the eighty-six patients with a family history of diabetes, 32 (37.2%) had active root caries. On the other hand, the percentage of patients with active root caries was 19.4% (42 out of 216) among those who had no history of diabetes in their families. Among those with 5 or more active root caries, 70% (14 out of 20) reported a family history of diabetes. To add to the confusion, among those with active root caries, only 6 patients had diabetes themselves. Those patients who reported a family history of diabetes had significantly more active lesions (p<0.0013). From the analysis by logistic regression, patients with a family history of diabetes were also 3 times more likely to have active root caries lesions (Table 1).
Few patients had restored root surface (10.6%). The prevalence increased among those who were unemployed. Three-quarters of the patients with 3 or more restored root surfaces were unemployed. Root surface restorations were 49.1% composite resin, 35.1% amalgam, and 15.8% glass ionomer.
42.4% of patients had at least one non-carious tooth surface loss lesion. The most affected teeth with non-carious tooth surface loss were the mandibular premolars, maxillary central incisors, maxillary canines, and maxillary first premolars, respectively. The most affected surface was predominantly buccal.
The prevalence of gingival recession was 57.0%, and the most affected teeth were the lower premolars, followed by the upper first molars. Pockets were mostly identified in maxillary molars, second premolars, and maxillary first premolars, respectively.
Bleeding on probing was mostly noticed in the maxillary second molars, maxillary first molars, mandibular second molars, and mandibular first molars, respectively. The surfaces that showed the tendency to bleed the most upon probing were the mesial and distal surfaces of the posterior teeth. While in anterior teeth, the lingual surface showed the most tendency to bleed upon probing.
| Variable | Coefficient | Standard Error | p-value | Odds Ratio | 95% Confidence Interval |
|---|---|---|---|---|---|
| Family History - Diabetes | 1.1166 | 0.3839 | 0.0023 | 3.0545 | (1.4394, 6.4819) |
| Constant | -1.2119 | 0.2278 | <0.0001 | - | - |
| Chi-Square = 10.2995 df = 1 p-value – 0.0013 | |||||
| Tooth Surface Loss | 1.3020 | 0.3737 | 0.0005 | 3.6768 | (1.7676, 7.6480) |
| Constant | -1.4901 | 0.2767 | <0.0001 | - | - |
| Chi-Square = 12.7657 df = 1 p-value – 0.0004 | |||||
| Age | 1.2597 | 0.3729 | 0.0007 | 3.5243 | (1.6970, 7.3194) |
| Constant | -1.4759 | 0.2771 | <0.0001 | - | - |
| Chi-Square = 11.9804 df = 1 p-value – 0.0005 | |||||
| Variable | Coefficient | Standard Error | p-value | Odds Ratio | 95% Confidence Interval |
|---|---|---|---|---|---|
| Root caries | 1.0210 | 0.3657 | 0.0052 | 2.7759 | (1.3555, 5.6847) |
| Constant | -0.7073 | 0.2065 | 0.0006 | - | - |
| Chi-Square = 7.9621 df = 1 p-value – 0.0048 | |||||
| Recession | 1.0772 | 0.3468 | 0.0019 | 2.9365 | (1.4880, 5.7949) |
| Constant | -0.9746 | 0.2624 | 0.0002 | - | - |
| Chi-Square = 10.0736 df = 1 p-value – 0.0015 | |||||
| Age | 1..3494 | 0.3503 | 0.0001 | 3.8551 | (1.9403, 7.6595) |
| Constant | -1.0076 | 0.2436 | <0.0001 | - | - |
| Chi-Square = 15.6075 df = 1 p-value – 0.0001 | |||||
| Oral Hygiene | 0.9949 | 0.2868 | 0.0005 | 2.7044 | (1.5416, 4.7444) |
| Constant | -2.6657 | 0.6907 | 0.0001 | - | - |
| Chi-Square = 13.4268 df = 1 p-value – 0.0002 | |||||
Plaque presence followed the same pattern of distribution as bleeding on probing. The prevalence of dental plaque was 96.0%, with all patients on average having over two-thirds of tooth surfaces covered with plaque, and only eight patients had no signs of plaque nor the tendency to bleed upon probing.
The patients’ age, oral hygiene status, gingival recession, and active root caries were found to be strongly associated with the presence of pockets. Logistic regression analysis further confirmed the multiplicative interactions between the two variables, age and root caries and the interactions between the three variables, age, root caries, and recession. The multiplicative odds ratios were 6.803 and 19.83, respectively (Table 2).
Regarding oral hygiene habits, 23.2% of patients reported brushing once a day, 68.9%, twice a day, 7.3% thrice a day, and only one patient reported brushing four times a day, and another reported not brushing at all. Interestingly, among those patients who brush their teeth thrice a day, 40% had poor oral hygiene.
3.2. Part II: Cross-sectional Patient Survey
Two hundred fifty patients out of 302 returned the questionnaire (82.8% response rate). 168 of these were male, and 82 were female. 8.9% were regular attendees, 16.3% were occasional attendees, and 74.8% attended only when in pain. 15.4% of patients, when asked about their attendance pattern during the COVID-19 pandemic, reported being unable to visit their dentists despite their need to do so. Interestingly, 48% (120) of patients reported that the last time they visited a dentist was more than two years ago, and only 30% (74) of patients reported their last visit to be less than 6 months ago. The median period of time elapsed since patients last visited their dentist was 9 months, ranging from 2 days to 20 years. Generally, there was a similar attendance pattern between the male and female patients.
Five study age groups were comprised as follows: the 16–20 years comprised 20 patients, the 21–30 years comprised 88 patients, the 31–40 years comprised 54 patients, the 41–50 years comprised 52 patients, and the 51+ group comprised 22 patients.
When asked whether they thought they might have decay, 55.6% of patients thought they might have, 23.4% thought they did not, and 21% did not know whether they had decay at that time. It was found that of the patients who thought they had decay, 28.6% had active root caries. Of those who thought they did not have decay, 16.2% had active root caries, and of those who did not know, 54.8% had active root caries (Fig. 2). About half the patients think they may get caries in the future.
Among those who thought they may get caries in the future, 41.1% acknowledged that their dietary habits and consumption of cariogenic foods would contribute heavily to this outcome. Approximately one-quarter of patients believe that their previous experience with caries indicates that they will be prone to further lesions as time progresses. Other factors included age, lack of oral hygiene care, orthodontic appliances, and bleeding gums.
Regarding patients’ knowledge, the causes and prevention of dental caries were unknown to 13.6% of patients, as were the causes and treatments of gum recession, gingivitis, non-carious tooth surface loss, and gingival pockets to 52.0%, 55.2%, 56.8%, and 63.2% of patients, respectively.
Surprisingly, only 38.7% of patients thought they had gingival problems, 40.3% thought they did not, and 21% did not know whether they had gingival problems at that time (Fig. 2). One-quarter of patients feel they may get gingival problems as they get older. When the patients were asked if they were worried or concerned about the prospect of getting caries or developing gum problems, 42.7% said they were worried or concerned. The level of concern was highest in the two younger age ranges, at 60% and 53%, respectively.
Among those who thought they may get gingival problems in the future, more than a quarter believed that their bleeding gums would indicate a developing gingival problem. The same number of patients acknowledged that their oral hygiene routine would contribute heavily to this outcome. Other factors included age, orthodontic appliances, crowded teeth, restorations, depression, smoking, and medications.
Table 3 contrasts the average number of teeth with gingival recession, filled (restored) root surface, decayed root surface (active root caries), and pocketed teeth according to age and against the vulnerability to caries among surveyed patients.
When asked to write down what they thought caused decay, 54.4% of patients said sugar, 46.4% said inadequate brushing, and 16.0% felt sugar and inadequate brushing were contributing factors. When asked what they felt would make teeth stronger, 61.6% of patients said a healthy diet (including fruit and vegetables, good quality food, fresh food, and fresh farm food) would have this effect.
| Age group | 16-20 | 21-30 | 31-40 | 41-50 | 51+ | Overall |
|---|---|---|---|---|---|---|
| Average Number of Teeth | ||||||
| Exposed | 0.21 | 1.31 | 2.97 | 5.15 | 10.58 | 3.21 |
| Restored | 0.29 | 0.22 | 0.32 | 0.18 | 1.92 | 0.38 |
| Decayed | 0.50 | 0.48 | 0.66 | 1.58 | 2.25 | 0.91 |
| Pocketed | 0.43 | 1.00 | 2.13 | 3.94 | 5.08 | 2.20 |
| Percentage | ||||||
| Vulnerability | 60% | 53% | 45% | 33% | 25% | 46% |
| Condition | - | ||
|---|---|---|---|
| a. Causes as reported by patients/ Percentage | |||
| Recession | Improper brushing 37.6% | Plaque accumulation 9.6% | |
| Gingival pockets | Inadequate brushing 20.8% | Plaque 8.0% | Caries 5.6% |
| Gum inflammation | Inadequate brushing 33.6% | Plaque 7.2% | |
| Non-carious tooth surface loss | Sugar intake 18.4% | Improper brushing 11.2% | Erosive foods and drinks 10.4% |
| Gingival bleeding | Improper brushing 38.4% | Gingivitis 13.6% | |
| b. How to prevent the condition as reported by patients/ Percentage | |||
| Caries | Brushing 56.8% | Reduce sugar intake by 10.4% | Regular check-ups 10.4% |
| Gum disease | Brushing and flossing 51.2% | Chairside cleaning 7.2% | |
| Non-carious tooth surface loss | Toothbrush usage and type 18.4% | Avoid erosive foods and drinks 9.6% | |
Regular brushing was seen by 42.6% and regular visits to the dentist by 10.1% as methods to strengthen the teeth. 8.2% felt cutting down on sugar intake would be effective. Interestingly, 20.2% thought milk and 18.1% calcium would strengthen teeth, yet only 16.4% mentioned fluoride (in various forms, such as toothpaste, mouth rinses, and simply as “fluoride”). 0.4% of patients mentioned chewing gum as an adjunct to tooth strengthening.
Table 4 shows patients’ responses when asked (a) about the causes of recession, gingival pockets, gum inflammation, non-carious tooth surface loss, and gingival bleeding and (b) how to prevent caries, gum disease, and non-carious tooth surface loss. Only 7.2% said that cleaning their teeth in the chair was a way to prevent gum disease, and 9.6% said that avoiding erosive foods and drinks was a way to prevent non-caries tooth surface loss.
When asked what they felt they could do to stop their teeth from decaying, 56.8% of the patients felt that regular brushing would be of benefit. 10.4% said reducing sugar intake, and 10.4% said brushing, reducing sugar intake, and regular check-ups would collectively positively impact. 2.3% felt that they could not do anything to prevent their teeth from decaying.
Interestingly, 28.8% of patients do not brush their teeth after the last meal or before bed. While one-fifth of patients (20.8%) maintained an adequate brushing and flossing routine, three-fifths (60.8%) had no routine whatsoever. Less than one-tenth of patients used mouthwash as an adjunct to brushing.
One hundred ninety-two patients (78.7%) had received some form of oral health advice from a dentist, whereas forty (16.4%) had received advice from an allied dental professional. Fewer patients had received oral health advice from other sources. Ninety patients (36.9%) looked up their oral health advice using Google, fifty-eight (23.8%) found some advice on social media platforms, forty-six (18.9%) asked their friends or relatives, and thirty (12.3%) referred to online forums. According to the patients’ perspective, the best dental advice patients got that had a positive impact on their daily routine, regardless of where they got it was to brush more often (50%), use floss (13.4%), have regular professional dental cleaning (9.8%), use the appropriate toothbrush hardness (7.3%), and use highly fluoridated toothpaste (6.1%). Other dental advice included using mouthwash, ceasing smoking, switching to a healthier diet, and reducing the consumption of fizzy drinks.
Regarding social media, most patients had learned new ideas about oral health care from YouTube (65.8%). The next most common source of information was Instagram (53.8%), followed by Twitter (35%), Facebook (21.4%), Snapchat (12.8%), TikTok (6%), Reddit (2.6%), and LinkedIn (0.9%). One patient remarked that they had not learned anything new on social media.
Table 5.
| Dental Problem | Action | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Call the Dentist | More Brushing | Take Medication | Change Diet | Apply Clove Oil | Saline Mouthwash | Avoid Affected Side | Pull Tooth Out | Apply Cold Packs | Google It | |
| Decay | 20.8% (52) | 22.4% (56) | 10.4% (26) | 6.4% (16) | 6.4% (16) | 4.0% (10) | 0.08% (2) | 0.08% (2) | - | 0.04% (1) |
| Exposed roots | 23.2% (58) | 12.0% (30) | 8.0% (20) | 2.4% (6) | 4.8% (12) | 4.0% (10) | - | 0.08% (2) | 0.08% (2) | 0.04% (1) |
| Hypersensitivity | 6.4% (16) | 12.8% (32) | 3.2% (8) | 24.8% (62) | 7.2% (18) | 2.4% (6) | 24.8% (62) | - | - | 0.08% (2) |
| Bleeding gums | 12.8% (32) | 15.2% (38) | 1.6% (4) | 2.4% (6) | 4.0% (10) | 8.0% (20) | - | - | 3.2% (8) | 0.08% (2) |
| Gingival pockets | 12.8% (32) | 24.8% (62) | 3.2% (8) | 1.6% (4) | 3.2% (8) | 6.4% (16) | 1.6% (4) | - | - | - |
| Swollen gingiva | 14.4% (36) | 8.0% (20) | 11.2% (28) | 1.6% (4) | 4.8% (12) | 4.0% (10) | 2.4% (6) | - | - | 0.04% (1) |
Few patients reported receiving their best advice from a source other than their dentist (23.8%). This included friends and relatives (9.7%), school (4.8%), and the web (2.4%). A high proportion of patients in this survey felt the advice they had received had helped enable them to keep their teeth cleaner 260 (86.1%), and prevent decay 238 (78.8%). However, it appears the patients were unable to assess whether the advice received had helped them stop gingival recession. One hundred and twelve (37.1%) thought the advice had helped them stop their gum shrinking, 52 (17.2%) thought it had not, and 106 (35.1%) did not know.
There appeared to be a high level of satisfaction amongst these patients as to the suitability of the advice they had been given. 83.9% of the patients thought the advice had been easy to understand; 84.8% felt it had been easy to remember, and 80.5% felt the advice had been simple and easy to follow.
When learning about new oral health ideas, the patients preferred to be taught by the dentist (55%), followed by experts on social media (20%), with the dental nurse, dental student, and receptionist not being popular (12.5%, 8.3%, and 4.2% respectively).
This sample of patients was not unanimous in their view of how often they felt they wished to be reminded about their oral care. 37.6% felt they would like to be reminded at every visit. 34.6% felt once a year would be preferable, and 24.3% felt they would like to be told once and never again. These views did not differ greatly across the different age groups studied. However, more 40-plus-year-olds felt they would like to be reminded at every visit compared to the younger groups. Indeed, when asked whether they would be interested in learning about the most recent advances in dentistry, about two-thirds of patients expressed their interest in learning at every visit.
Seventy-seven percent of the patients felt a take-home leaflet would be helpful to remind them of new ideas which had been introduced to them by the dentist. 8.5% thought a leaflet would not be helpful, and 14.5% did not know. The most popular method (47.1% of all patients) of assimilating the contents of a new information leaflet was by reading the leaflet privately at home. The next popular method was having the dentist go through the leaflet point by point with the patient (35.3%). And the least popular was by reading it alone and then having a brief explanation by the dentist (17.6%).
When asked if they would see a dentist right away if they had cavities, exposed roots, hypersensitivity, gingival pockets, bleeding gums, or swollen gums, 72% of patients said that having exposed roots was the only problem that required immediate action (Table 5).
4. DISCUSSION
The results demonstrate consistency in data recording. The high correlation of gingival pockets with oral hygiene and age, and root caries with age, suggests that a high degree of measurement bias did not occur.
Although most patients were aware of “shrinking gums” or gingival recession, and there was some confusion about condition's progression. The prevalence of 51.6% for gingival recession and 29.8% for root surface caries within the study population suggests that root caries is already a dental management problem.
There was a marked feeling of vulnerability to decay within this study population, which was echoed in a recent systematic review on caries and periodontal disease in socio-economically disadvantaged individuals [10]; the two younger age groups felt more vulnerability than the older groups (60% and 53%, respectively), and it would have been helpful to have explored this feeling in more depth.
The difference in root caries prevalence among different age groups was statistically significant (p = 0.0005). A very strong association was found between non-carious tooth surface loss and age with active root caries. Patients with non-carious tooth surface loss were 3.67 times more likely to have active root caries, and older patients were 3.52 times more likely. This is consistent with the notion that non-carious tooth loss may be complicated by superimposed root caries and that advancing age may be an aggravating factor in root caries susceptibility [11, 12].
A link was also established between a family history of diabetes and root caries. Patients with a family history of diabetes had significantly more active root caries lesions (p = 0.0013). Those patients were three times more likely to have active root caries. Having prediabetes and diabetes increases the likelihood of developing periodontal disease in the oral cavity at an increased rate. This association has been established at both a pathophysiological and an epidemiological level [13-15].
The findings of the present study suggest that screening patients with root caries at the dental office for prediabetes or diabetes is strongly justified based on the strong association between root caries and a family history of diabetes [16]. Therefore, it is suggested that a chairside test would have important value in assisting both oral and medical healthcare professionals in identifying patients that are not only at risk of diabetes-related periodontal disease but also at risk of remaining undiagnosed and untreated.
The difference in gingival pocket prevalence among different age groups was statistically significant (p = 0.0001). A strong association was found between oral hygiene, gingival recession, root caries, and age with the presence of gingival pockets. Patients with poor oral hygiene were 2.70 times more likely to have gingival pockets, those with recession 2.94 times more likely, those with root caries 2.78 times more likely, and older patients 3.86 times more likely. A substantial number of studies on the link between aging and gingival problems have reported an increased prevalence and severity of the condition with advancing age [17-19].
Most of the patients reported brushing their teeth twice a day and using only toothpaste. Floss was the most popular of the oral hygiene aids used. The reported cleaning habits of the UK are fairly similar, with Oman having a slightly lower uptake of oral hygiene aids. Despite the lack of evidence about oral hygiene aids’ differences in the impact on patients [20, 21], the limited adoption of a preventive strategy in dealing with dental problems, as is found in the present study, seems to account for the lack of motivation in patients to use oral hygiene aids.
4.1. Preventive Strategy
Information inaccessibility among patients can have adverse effects on effective dentist-patient communication and on the quality of patient care [22]. The majority of patients involved in this study view further carious attacks as inevitable and with concern. However, patients in all areas of the study had little idea of what would happen to dental tissues as they aged. A very high percentage of patients felt vulnerable to tooth loss and caries. At the same time, the patients’ awareness of the disease was not high; among those patients who did not know whether they had root caries or thought they did not have active root caries, 71% had active lesions.
Patients’ understanding of gingival and periodontal disease was similarly confused. Although high proportions of patients had heard of the term, less than half the patients examined thought they had gingival or periodontal disease. A small proportion of patients thought they might get gingival or periodontal disease in the future, and a high proportion of patients felt these conditions might lead to further problems. The literature has noted that a lack of patient education about the seriousness of periodontal problems contributes to misconceptions, which pose a long-term risk to oral health [7].
Approximately one in three Omanis do not have the knowledge or access to the resources required to make appropriate decisions about their dental health. This lack of dental health knowledge impedes the patient’s dental care plan since effective dentist-patient communication has been shown to improve adherence to oral health and preventive recommendations [23, 24].
Patients in this study rarely attended dental check-ups. However, they prefer to be given new information and oral health advice by their dentist. Less than one-fifth of the patients preferred to be given new information from other sources. Interestingly and recently, the central thrust of most postgraduate initiatives, aimed at increasing the quantity and effectiveness of preventive advice that is given in general practice, has been the increased use of ancillary staff in the delivery of the advice [25]. This approach is at odds with the preferences of the patients in this study.
The patients express a high level of satisfaction with the dental advice they have received and believe this advice has helped reduce recession and caries and helped keep their teeth cleaner, even though the clinical data do not support this view. It is also interesting to note the small impact the various social media platforms had on patients in comparison to the impact made by their dentists. This result is comforting, considering the risks social media poses in its ability to influence our interpretation of healthcare topics [26]. Unvetted Social media platforms can easily impede the plans of the dental health mission.
The authors of the present study believe that the preventive approach, although not fully adopted, had an impact on the perception of the wide range of dental advice offered to patients. The finding that patients are divided in their preferences for the regularity of reinforcement of preventive messages will undoubtfully make it very difficult for dentists to judge which approach to adopt to each different patient. This might be attributed to the unique psychological makeup of each patient [27]. Interventions intended to change patients’ oral health behaviours are often based on theoretical behavioural models. In such models, individuals are encouraged to be responsible for their health, which is inadequate and may contribute to social disparities in oral health [28, 29].
Patients do appear to be confused about relatively simple preventive issues or are choosing to select the pieces of the preventive message which suit them best. There appears to be an incredible lack of association between fluoride and the prevention of caries, as well as tooth erosion and the consumption of acidic foods and beverages, and in some patients, an inability to replace rather dated messages with more contemporary ones, such as clove oil to heal gum inflammation, reduce hypersensitivity, and stop tooth decay, and milk and calcium to help make teeth stronger.
Due to the recent pandemic, patients have found it more difficult than ever to attend a dental office [30]. As a result, routine dental care is sometimes postponed, causing patients to use over-the-counter alternatives or homemade remedies that may not be necessarily recommended or appropriate to address dental problems [31]. This is easily understood, given the circumstances of the pandemic. However, the use of unprescribed antibiotics in the management of gum problems is a major issue. It will require extensive preventive campaigns as well as active support from dentists and dental public health professionals [32].
Root caries will continue to be a prevalent oral problem in the future, and approaches for successful prevention and control are required [7]. These approaches will benefit from identifying vulnerable individuals or populations. While our study uses cross-sectional data and cannot forecast an individual's future risk of acquiring root caries, it can enlighten us about potential disease indicators, guiding clinicians' diagnostic processes and directing public health efforts.
Are patients content to go along with what dentists consider high plaque levels, accepting the inevitability of replacement restorations and root caries? If patients are content, should a well-meaning dentist disturb them? If we disturb them, who should pay for the preventive treatment? This delusion will not last forever — dentists are locked onto the treadmill, unable to devote enough time to preventing disease in patients who feel vulnerable but are largely unaware of the implications of the ageing process on their oral tissues. We believe that some dentists, at least the ones in our institution, are uncomfortable with this situation, and others are prepared to collude with patients until change is forced upon them.
This work has demonstrated that the key factor in a preventive package to be used with regular attendees is the dentist. The dentist is crucial in the delivery of preventive advice, in tailoring it to each individual patient, in determining the frequency of reinforcement, and in the financing process.
Given that dentists do not appear to be as effective at influencing changing behaviour in their patients as the results of this work suggest, those dentists committed to effective change must invest time and effort in determining what influences behaviour change in patients. There is ample evidence in the literature that suggests strategies which may be of assistance when affecting behaviour change [33-36]. This must be a crucial component of the preventive package. The present arrangement, which can be seen as producing satisfied patients, is failing to establish the desired levels of oral cleanliness and caries prevention.
Other key features in this preventive package are the simplicity of the preventive message and the acknowledgment of the limitations of the patients’ power of assimilation. A simple preventive message is required, which, while tailored to the purpose of preventing root caries, echoes the message used in all other areas of oral health promotion. It is essential to reduce the confusion prevalent in the minds of patients. Patients should be aware of the following points in regard to root caries prevention: gingival recession and ways to minimise it; the importance of regular dental care; the use of fluoride in caries control; methods to use in the adequate removal of plaque; the same things causing caries in adults as in children; the association of caries with sugar frequency and total sugar consumption; food and drinks that contain sugar; and the necessity for adequate saliva and xerostomic effects of medication.
As highlighted above, the dentist has to advise and tailor the preventive message for each individual. The dentist must then decide on the most appropriate technique for passing this message to the patient, who should be involved in this process, and how often the process is repeated or modified. An understanding of the theories of behaviour change, especially the TransTheoretical Model, might be of value to the dentist in this regard [37].
What would emerge is an individual “preventive prescription” for each patient, which could be incorporated into the individual’s overall treatment plan. This is an approach that is likely to be acceptable to Dental Public Health experts and might easily be taken to be representative of the dental profession. If acceptance was gained, preventive treatment planning could be included in the fee scale narrative. This move, if adequately funded, would encourage dentists to adopt a more preventive outlook on their work.
A patient advice leaflet (digital or printed) may be of benefit in reinforcing the simple preventive message. Once again, the dentist is considered crucial in this part of the package, in that many patients expressed the preference for their dentist to go through the contents of such a leaflet with them before they take the leaflet home.
The areas which could be usefully covered by such a leaflet are those listed above. Specifically, minimising recession, regular dental care, the use of fluoride, plaque removal, sugar frequency and consumption, and the importance of saliva. Such a leaflet might be a mixture of very simple text, simple diagrams, and photographs.
Recent research emphasizes the enduring challenges in oral health, particularly inequities in oral health status, access to care, and utilization, which have wider impacts on the economic wellbeing of societies [38]. This underlines the necessity of our proposed individualized 'preventive prescription' and further cement the importance of prevention and the need to improve access to care in order to mitigate these inequities. Moreover, there is a call to leverage new understandings of oral diseases and the economic value of oral health to inform better policy choices.
Furthermore, one study revealed the significant impact of dental instructions on daily oral hygiene practices [39]. Despite this, it found that only a small number of individuals recall receiving oral health prevention and promotion advice from a dentist. This underscores the necessity of improving communication between dental practitioners and their patients and the importance of providing detailed, repetitive, and tailored advice, as we have emphasized in our study. With digital technology becoming increasingly prevalent, it holds the potential for developing more effective, tailor-made educational strategies. This is in alignment with our suggestion for a patient advice leaflet (digital or printed) that reinforces simple preventive messages.
Educationally, as the only dental school in Oman, we hold the distinct honor and responsibility of educating young professionals who will carry dentistry's torch into the future. Therefore, we believe that the UK model, specifically the “Delivering better oral health” intervention [8], can serve as a reference and a source of ideas on how to further improve oral health among the Omani population. Incorporating these perspectives into our study, we argue for the necessity of a proactive preventive strategy against root caries in the Omani population, encompassing tailored patient advice, improved communication, leveraging digital technology for education, and an emphasis on prevention in policy decisions.
Cultural and socioeconomic factors, such as dietary habits, oral hygiene practices, access to dental care, and oral health awareness, can vary across regions and populations. Therefore, the findings of this study may not be directly applicable to populations with different cultural backgrounds or varying healthcare systems.
CONCLUSION
Based on the strong connection between root caries and a history of diabetes in families, the present study suggests screening patients with root caries for prediabetes or diabetes at the dental office. We suggest a chairside test would assist dental and medical healthcare professionals to identify patients who are not only at risk for diabetes-related periodontal disease but are also at risk of not being diagnosed and treated. Further research is needed to confirm our findings.
Patients had minimal knowledge about root caries and gingival health. The disease levels and lack of patient awareness back this up. The patients involved in the study were confused about the aetiology and prevention of root caries and expressed a high level of vulnerability to both caries and recession.
The results of this work indicate that the most important feature of a root caries prevention package is the motivation of the dentist. The preventive message delivered by a well-motivated dentist and selected members of the dental team would be simple and include advice on minimising recession, the use of fluoride, adequate plaque removal, the association of sugar with root caries and the importance of adequate salivary flow. This advice might be backed up by a simple leaflet. For a more realistic implementation of preventive advice, peer pressure or financial reward might be used as an incentive to encourage dentists to invest in appropriate interpersonal skills and adopt a more preventive approach to their practice.
The findings of this study have led to the development of a ‘prototype’ preventive strategy for use in general dental practice. In order to develop and refine this strategy further, it would be helpful to have more data in certain areas. From the patient's perspective, further research is required to determine the most effective methods of increasing the understanding of the role of regular dental care in caries prevention and informing patients of the expected age changes of the oral tissues.
A programme is required which would, in a positive way, make dentists aware of the shortcomings of the present approach to patient education and motivation and equip them with the necessary skills to implement a successful preventive strategy against root caries in their practice.
LIST OF ABBREVIATIONS
| BASCD | = British Association of Community Dentistry |
| DBOH | = Delivering Better Oral Health |
| COVID-19 | = Coronavirus Disease of 2019 |
| SD | = Standard Deviation |
AUTHORS' CONTRIBUTIONS
NAH: study design, data acquisition, analysis and interpretation of data, writing publication; AQ: study design, data acquisition, analysis and interpretation of data, writing publication; PP: conception and design; HC: conception and design, analysis and interpretation of data; EFR: conception and design, analysis and interpretation of data, critical revision of publication, supervision. All authors have read and approved the final manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Institutional Review Committee of Oman Dental College (ODC) (ODCNH/2021/4 – Jan 2021). Informed consent was obtained from all subjects involved in the study.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
All data supporting the results of this study are available from the corresponding author upon request [A.Q].
ACKNOWLEDGMENTS
The authors of this work would like to express their gratitude to Drs. R Al Nahdi and S Al Shereiqi for all the hard work and insightful feedback they provided.
APPENDIX
Questionnaire Questions
- Question 1 determines the sex of the patient in order that gender comparisons can be made ; caries and restorative experience, dental attendance patterns, knowledge of recession, caries prevention, dental experience, and attitudes to other dental issues.
- Question 2 was used to determine if the patients were regular, occasional, or emergency-only visitors. Patients from various backgrounds were compared in the manner described above.
- Question 3 “Do you think you have tooth decay?” is a very direct question designed to assess the patient’s perception of their oral condition and to correlate this with the dentist’s clinical findings on examination.
- Question 4 “Do you think you may get decay in the future?” explores the patient’s view of whether they are still susceptible to decay.
- Question 5 “Does the thought of getting decay, worry, or concern you?” explores the patient’s feelings of vulnerability to decay.
- Question 6 “Write down the things you think can cause tooth decay”. This open question allows an exploration of the patient’s knowledge of the aetiology of caries.
- Question 7, “Write down the things you think are good for teeth and make them stronger”. Another open question to investigate the patient’s knowledge.
- Question 8, “What do you feel you can do to stop your tooth decaying?” is an attempt to probe the knowledge of caries prevention.
- Following the same theme, questions 9-12 investigate patients’ knowledge of gingival problems.
- Question 13, “Have you ever had advice about looking after your teeth from; your doctor; a social media health expert; a nurse; hospital/clinic doctor; your dentist?” At one level, this question investigates the sources of oral health advice.
- Question 14, “Do you feel the advice you received in the past has helped you to: keep your teeth cleaner, prevent decay, stop shrinking gums?” Patients were asked to select yes, no, or don’t know as options to this question. Question 15, “Do you feel that the advice given to you in the past was: given to you in a way that was easy to understand, easy to remember, simple to follow?” Once again, the answer options are yes, no, or don’t know. This question explores patients; feelings about the delivery of dental advice which they had experienced. Did they feel the message had been pitched at the right level, or was it too complex? Questions 14 and 15 are intended to measure how useful oral health information has been to patients in the past.
- Question 16, “Where do you learn new ideas about looking after your teeth? Patients were asked to tick as many of the answers as they wish: being shown by the dentist; from radio; from television; from newspapers, from social media (YouTube; Instagram; Twitter; Facebook; LinkedIn; Snap Chat; TikTok); from friends or relatives; from waiting room leaflets; or other sources.
- Question 17, “When you learn new ideas about looking after your teeth, who would you most prefer to show and discuss the ideas with you?” The preferences were to be ordered 1-5: dental nurse, dentist, receptionist, dental specialist, dental student. This question explores whether the patient prefers to hear new ideas from the most senior member of the dental practice.
- Question 18, “How often do you need to be reminded about new ideas and ways of looking after your teeth?” Patients were asked to select one answer from: at every visit, once a year, only once, and never again.
- Question 19, “Would a take-home leaflet help you remember the new ideas told to you by the dentist?” Patients were asked to select from yes, no, or don’t know.
- Question 20, “If you were to have a new information leaflet would you prefer: to pick it up in the waiting room and read it privately at home, the dentist to go through the leaflet point by point explaining what each part meant and then taking it home as a reminder, or, to read the leaflet on your own and then the dentist giving you a brief explanation? Patients were asked to tick one box.


