A Case Report of Different Management Protocols for Uncomplicated Crown Fracture in Young Permanent Teeth; Fragment Reattachment vs. Resin Restoration
Abstract
Introduction:
An uncomplicated crown fracture (enamel-dentin fracture) is the most clinically reported traumatic injury. Many techniques have been reviewed to manage this traumatic injury. The literature has no consensus on the best strategy to establish optimal biological, functional, and esthetical success.
Objective:
This clinical case reports different management of uncomplicated crown fractures in young permanent teeth that were successfully treated using both tooth fragment reattachment and composite build-up.
Case Report:
A 9-year-old female presented as an emergency patient with immature fractured upper central incisors. She hit her mouth into a solid wall and broke her front teeth during playing. Upon parental advice, the fragments were stored in a container of milk since the incident. For dental management, two treatment approaches were used.
Conclusion:
After a two-year follow-up, the treatment is considered successful and the traumatized teeth are vital, functional and presented with a complete root development.
1. INTRODUCTION
Crown fractures of the anterior teeth are the most frequent traumatic injuries affecting permanent teeth. The prevalence of crown fracture is very high compared to other traumatic dental injuries, which comprise 26% up to 76% [1]. Among all school children, 25% had experienced dental trauma [2]. The most frequent age reported in children affected by dental trauma is between 8 and 12 of age. This could be attributed to the activities that were usually practiced during this period. Of these traumatic injuries, about 92% are reported to be maxillary anterior teeth (central followed by lateral incisors) [3-5]. Fractured anterior permanent teeth in a young patient with an immature root development often represent a challenge for achieving function and aesthetics conservatively. One of the desirable management is by re-attachment of the fractured fragment to the injured tooth [6]. This approach allows the dentist to restore the original anatomy of the tooth, and it is considered very conservative, especially if the fragment is available, intact, and has good adaptation to the injured tooth [7-10].
However, in case of a missing, fractured fragment or the fragment is severely injured, other treatment options need to be considered. The most commonly used approach in children is restoring the traumatized tooth with a composite resin restoration. This is a valuable option also as it had good esthetic results and an acceptable retention rate.
According to the international traumatology guidelines, the management of such injuries as early as possible is highly recommended. Immediate dentin coverage is preferable to minimize bacterial ingress through the dentinal tubules or any thermal/chemical stimulation and subsequent pulpal inflammation [1, 11]. Maintaining the vitality of the pulp in the traumatized tooth is very critical in a young patient with immature root development. This is to allow the continuation of root development [12, 13]. In general, the risk of complications increases if the crown fracture is associated with luxation injury [14, 15].
This case report aimed to present two treatment approaches to manage uncomplicated crown fracture in a young patient that consisted of fragment reattachment and a composite restoration buildup.
The treatment results, in this case, are considered successful after a two- years follow up and the overall prognosis is good as the clinical and radiographic evaluation revealed an intact restoration, positive pulp response, negative response to percussion, normal mobility, and continued root development.
2. CASE OPERATION PROCEDURE
A 9-year-old girl came to the emergency department with a history of uncomplicated crown fracture in the maxillary central incisors, as shown in Fig. (1).

Basic trauma history of loss of consciousness, head trauma, amnesia, drowsiness, vomiting, or headache was taken and ruled out in the emergency department (ER). A clinical and radiographic examination was done by the first author in the ER, and a dental appointment on the same day was given for management. A detailed trauma history was obtained in the dental clinic several hours after the traumatic injury. The American Academy of Pediatric Dentistry (AAPD) trauma form was filled out, which has the advantage of approaching the case systematically. Table 1 presents the dental trauma history and the assessment that was carried out.
| Type of injury: Enamel-dentin fracture (uncomplicated crown fracture) of teeth #11 + #21 |
|
|---|---|
| When | 2 hours ago. |
| Where | At home |
| How | She was playing with her cousins, covering her eyes with a scarf and running trying to catch them, when she hit her mouth into a solid wall and broke her front teeth. |
| Clinical examination: | |
| Tooth displacement | None |
| Abnormal mobility | None |
| Tooth color | Normal (matching with adjacent non-traumatized teeth) |
| Tenderness to percussion | Negative |
| Percussion sound | Normal |
| Occlusal disturbance | None |
| Response to sensibility testing | Positive in both electrical and thermal |
| Radiographic examination: | |
| Enamel-dentin loss of right and left maxillary central incisors (#11 + #21). Intact PDL spaces and lamina dura. Not associated with tooth displacement. No signs of periapical radiolucency or inflammatory resorption. Immature apex of both maxillary incisors #11 and #21 “incomplete apical development”. No concomitant root fracture. |
|
A review of medical history revealed no significant findings with no history of previous hospitalizations and the vaccinations are up to date. The dental history indicated that this patient brushed her teeth irregularly and did not regularly follow up with the dentist. Also, she has a tongue thrust habit. No history of previous trauma to oral dental hard and soft tissues. The extraoral examination was within normal limits with no contusions, lacerations, or any other soft tissue injury as a consequence of the trauma. Intraoral examination was carried out with findings of severe MIH affecting all the first permanent molars and the lower central incisor, multiple carious teeth (primary and permanent including nonrestorable tooth #36), and the patient at a late mixed dentition stage. Assessment of occlusion indicated that; the patient has class II molar relation on the right side. Increased overjet and anterior open bite secondary to tongue thrusting habit. Constricted maxilla with protrusion of upper anterior teeth. She has poor oral hygiene and is at high risk according to the caries risk assessment tool with cooperative behavior (Frankl III).
Upon clinical examination, both upper permanent right and left central incisors (teeth #11 and #21) had uncomplicated oblique crown supragingival fractures involving enamel and dentin. There was no spontaneous pain from the teeth. There is a mild reaction to thermal stimuli, “cold air and drinks.” The teeth were not tender to percussion test with normal mobility, and no disturbance in the bite was noticed. Both of these traumatized teeth give a positive response to the pulp vitality test.
Only one of the two fragments was available at the accident scene, as shown in Fig. (1). The other one was badly broken into small pieces. The patient’s father kept the fragments in a bottle of milk and was instructed to keep them in the bottle until the morning to be seen in the dental clinic.
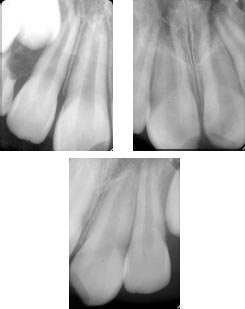
A periapical radiograph was taken for the radiographic examination as it is recommended by the International Association of Dental Traumatology, which revealed that Tooth #11 and #21 had an uncomplicated crown fracture (visible loss of enamel and dentin) with no signs of periapical radiolucency, no signs of tooth displacement, no signs of root fracture, had immature root development with an open apex (Fig. 2).
The treatment plan was made, which included comprehensive management of the traumatic injuries, restoring all carious lesions, monitoring of the tongue thrust habit, and improving overall oral hygiene.
The trauma documentation and the treatment of upper anterior central incisors were carried out in the emergency phase. To restore the esthetic and the patient’s self-esteem. Fragment reattachment of tooth #11 using over-contouring and beveling techniques. The fragment was checked for fit, cleaned, and maintained in normal saline. The following steps were used; tooth #11 and it is fragment etched with 37% phosphoric acid (Etchant Gel, 3M ESPE, USA) and rinsed with water. The adhesive-bonding agent was applied and air-dried gently, followed by light curing, the adjacent teeth were protected with a celluloid strip. An increment of flowable resin composite material (SmartCem2, Dentsply Maillefer, USA) A2 shade was placed over the tooth and the fragment to hold them in position and light-cured. Over-contouring and beveling techniques were used in fragment re-attachment to achieve retention and increase fracture resistance. Also, for retention purposes, a superficial preparation of about 0.3 mm depth is placed on the buccal surface extending about 2.5 mm coronally and apically in length from the fracture line. The preparation was then filled with a thin layer of composite. Margins were finished with white stone and diamond finishing burs and polished.
Regarding tooth #21; the treatment option was to resto the Class IV fracture site using composite resin restoration by applying the following steps; facial and lingual beveling was done, etched and bonded, then restored with Cl. IV composite resin restoration.
Post-operative instructions were given, which included; avoiding hard foods and maintaining good oral hygiene, and chlorhexidine gluconate 0.12% was prescribed.
The patient also undergoes a comprehensive treatment for other teeth, which includes restorations, extraction of un-restorable teeth, and myofunctional therapy for the tongue thrust habit. Clinical and radiographic examinations were carried out over two years, and the patient is showing much improvement in her oral care habits (brushing regularly and reducing sugary snacks). Also, The patient's occlusion was improved (the increased overjet and open bite had been corrected, and the tongue thrusting habit stopped). Overall prognosis is expected to be very good if the child maintains good oral hygiene and regular dental visits.
2.1. Eight-week Follow-up after Treatment
The patient was re-examined clinically and radiographically (Fig. 3). No complaints or changes were noticed. Diagnostic tests demonstrated no abnormal mobility, negative to percussion test, positive to sensibility tests, and no signs of crown discoloration. Oral hygiene measures and the need for more recall visits were reinforced.

2.2. Ten-month Follow-up after Treatmen
The patient was re-examined clinically and radiographically (Fig. 4). There was a defect in a part of the restoration related to the left maxillary central incisor, and a repair with a resin composite restoration to only that tooth was done.

The overall prognosis was good for both traumatized upper central incisors (teeth #11 and #21); since there are:
Clinical Success; there were no symptoms of pain, tenderness to percussion, swelling, fistulation, or pathologic tooth mobility.
Radiographic Success; absence of pathologic internal or external resorption, furcation, or periapical radiolucency.
2.3. Two-year Follow-up after Treatment
The patient was re-examined clinically and radiographically (Fig. 5). No new complaints or changes were noticed. The reattached fragment and Cl. IV resin restoration was intact. This case showed predictable clinical and radiographic outcomes. Clinically there are no signs and symptoms of pain, discoloration, pain to percussion, or increased mobility. Give a normal response to the pulp sensibility test. Radiographic success was also observed, which included signs of root maturation and no signs of periapical radiolucency or root resorption. Oral hygiene measures and the need for preventive recall visits were reinforced.

3. DISCUSSION
With the advancement in adhesive materials, the possibility to restore both functions and esthetics has become more practical. Although there is no single technique that has long-term success in both retention and fracture resistance. The systematic review of Garcia et al. reported two strategies that are preferable among others; simple reattachment of the tooth fragment compared to over-contouring and dentine grooves and the use of material over the dentine to increase the bond strength [16].
Bonding is affected by many factors; which include how much of the tooth structure remains; fragment hydration status; the material used; perpendicular and oblique fractures are unfavorable patterns due to less tooth structure support [17, 18]. On the other hand, many variables were reported to increase the success rate, such as using of grooves and over-contour composite technique [19], and the use of the total-etch technique [20, 21]. About 97% of the strength of a natural tooth was obtained by using the over-contour technique [19].
Previous studies used variable techniques for re-attaching a fragmented tooth. AlQhtani used retentive holes as a measure of retention before re-attachment of the fragment [22]. Another study assessed different materials and techniques, and they concluded that the technique used had affected the fracture strength more than the materials used [23]. Panchal D used a double chamfer technique and the treatment was satisfying and successful over a one-year follow-up [24]. However, others found the use of additional preparations does not enhance the retention of the re-attached fragment [16, 25, 26].
Interestingly, a recent study that assessed the survival rate of both fragment reattachment technique and direct composite restoration found that the survival of direct composite restoration (65%) over 2 years is significantly higher than that of reattachment (42.9%). The failures that were mostly reported with fragment reattachment were related to the restoration and pulp necrosis. They explained this by the increased bonding surface of composite restoration compared to reattachment with means of mechanical preparation of the tooth surface [27].
In contrast to this study, others reported high satisfaction, success, and survival rate of the fragment reattachment technique [4, 5, 10, 28-31]. This difference can be explained by different factors that might affect the survival analysis. For example, the type of fracture is a significant influencing factor. Crown fractures with pulp involvement were reported in a more biological failure that resulted in a higher prevalence of pulp necrosis [27].
Overall, in both trauma types (complicated or uncomplicated) and both techniques (reattachment or direct composite restoration), the two variables that could increase the probability of the complications are concomitant luxation injury and a second trauma [4, 9, 32, 33].
The hydrated fragment in milk, as shown in this case, is a very important thing to be done in traumatic injuries. This has a beneficial effect on the boning strength and color. Increasing awareness in the management of dental injuries is very important for both the emergency physicians because, in most cases they are first to see the patient, and the parent of the pediatric patient. One study on the effect of the different storage mediums on the bond strength of the fractured fragment found that; milk and saliva are the best compared to other environments [34]. Another study found no effect of the medium on the bond strength nor on the survival of the fragment [35].
Rehydrating a fragment in water or saline is recommended before reattachment. This moisture was reported to increase the bond strength, color, and fracture resistance. The time needed to rehydrate the fragment is 15-20 minutes [6, 36, 37].
The International Association of Dental Traumatology recommends a one-year follow-up of the patient. Because most of these failures occurred during the first year following the trauma [4, 5]. However, a two-year follow-up could be beneficial for the patient to detect early biological or restoration complications [27].
The prognosis and success of fragment reattachment depend on many factors. One of the most important to be considered is pulp vitality, but this complication is very rare (0%-6%) in cases of the tooth with a crown fracture without concomitant luxation injury. The esthetic concern which also reported to be acceptable to the patient. Lastly, fragment retention seems to be good if the patient does not face a second trauma or nonphysiologically fragment use [1].
CONCLUSION
Fragment re-attachment is a viable technique in repairing fractured tooth structure following a traumatic experience. However, the operator must understand the basic principle of adhesive bonding and the necessity for auxiliary retention features. In this case, both methods provide similar retention and esthetics results and are reliable treatment options.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.


