The Correlation between Trigeminal Neuralgia and Local Anesthetics Neurotoxicity Associated with Acute Inflammation: A Cross-sectional Study
Abstract
Background:
Trigeminal neuralgia (TN) represents a subject of importance in oral medicine due to the large number of patients complaining of TN who are aware that the orofacial pain has a dental origin and therefore seek initial care from the dentist. The reasons for the majority of TN cases remain controversial, but nearly 10% of patients have an obvious pathological condition, such as intracranial pathology.
Aim:
This study aimed to assess the correlation between idiopathic trigeminal neuralgia and local anesthetic overdose and/or repeated injections caused by dental malpractice.
Patients and Methods:
An adequate sample of thirty-four patients was selected from the teaching clinic of oral medicine in the College of Dentistry, the University of Karbala, Iraq. All patients were fit for the inclusion criteria and subjected to a thorough oral examination to exclude any organic diseases that cause orofacial pain. Also, they were subjected to a medical examination by multiple neurologists using magnetic resonance imaging and other medical investigations to ensure that all patients did not suffer from intracranial pathology.
Results:
The patients were statistically distributed by their ages into two sub-groups. The first group (25-48 years old) represented 52.94% of all patients, and the second group (49-72 years old) included 47.06%. The percentage of disease according to sex was 79.4% in males and 20.6% in females. 3-6 dental carpules containing lidocaine (2%) with epinephrine were given to patients. The data of the studied sample were analyzed by using the statistical package of social sciences (SPSS) version 25. The chi-square test was used to test the effect of the type of dental procedure before pain in the two age groups and the two sex groups. For the age group, the difference was significant (p-value < 0.05), which indicated an increased incidence of nerve damage caused by local anesthesia in older patients. For the sex group, the chi-square test exhibited a value of 2.45, with no significant difference (p-value > 0.05). The main theory suggested for the occurrence of local neuropathies and the initiation of TN was the demyelination of nerve, which may be due to the neurotoxic effects of local anesthesia administered at high concentrations and for prolonged exposure times (repeated injections at the site of the dental infection after failure of LA) that may activate the intrinsic pathway of apoptosis through cytochrome C release. The local anesthetic-related neurotoxicity has thus been found to have harmful effects on the nerve tissue, including demyelination and axonal degeneration.
Conclusion:
The malpractice of local anesthesia in dentistry may lead to dysesthesia, allodynia, and trigeminal neuralgia with different degrees and severity due to the neurotoxicity of the peripheral nerve fiber. The nerve damage may occur in many forms, such as demyelination, apoptosis, axonal degeneration, and hypoxia due to thrombosis. So, dentists should recognize the risk of repeated injections or high dose solution (4%) of LA in the inflamed tissues when inducing analgesia for their dental operations that might initiate the primary trigeminal neuralgia.
1. INTRODUCTION
Trigeminal neuralgia (TN) is an infrequent illness with an incidence of 3–5 patients per 100,000 (the evidence of the increased risk in older patients raises the incidence by threefold to 6–12 humans per 100,000). Despite being infrequent, trigeminal neuralgia represents a subject of importance in oral medicine due to the large number of patients complaining of TN. The patients experiencing this pain are aware that orofacial pain has a dental origin, so they seek initial care from the dentist. The pain arising from TN is severe, sharp, paroxysmal, and stabbing in character, but it persists for seconds or minutes and may be described as a sudden attack. However, attacks may occasionally or rapidly recur at short intervals. There is a special area called the trigger zone within the distribution of the trigeminal nerve; when it is stimulated, it can provoke an attack at intraoral or extraoral points. The common stimuli include currents of cold air when brushing teeth and the mastication force that can induce pain. Therefore, TN is considered neuropathic pain. The common positions of trigger zones are the nasolabial fold and infra-orbital regions. The pain commonly radiates to areas outside the trigger zone as a form of orofacial pain. The incidence rate of this pain is different, starting from several episodes per day to some incidences per month; in some advanced cases, the orofacial pain may become constant. The TN pain is permanently located unilaterally, and it occurs mainly in the second (superior dental nerve) rather than the third (inferior dental nerve) trigeminal divisions, but less frequently in the ophthalmic division [1].
There are three types of TN, idiopathic, classical, and secondary. The classical form is considered the most common and is initiated by intracranial pressure of the “superior cerebellar artery” on the trigeminal nerve root. The secondary TN accounts for about 15% of the cases related to many neuropathological conditions. Idiopathic TN accounts for about 10% of all cases of TN, and this type has an unclear reason for nerve pathology or damage.
The reasons behind the majority of TN cases are still controversial, but nearly 10% of patients have an obvious pathological cause, like a cerebellopontine angle neoplasm, a demyelinating plaque of multiple sclerosis, or a vascular malformation [1, 2]. Several theories exist regarding the etiology of TN. The commonly accepted reason is the presence of abnormal superior cerebellar artery anatomy, which presses against the root of the trigeminal nerve in the posterior fossa of the cranium [3]. Microvascular decompression has been used for treating blood vessel abnormalities in TN.
The demyelination of nerves has regularly been proposed as one of the pathological causes that lead to orofacial pain and atypical electrical excitability. This theory is questionable as managing the site of the root of the trigeminal nerve by neurologists may result in the removal of painful periods despite the atherosclerotic blood vessels not compressing the nerve root. On the other hand, some other investigators state that the main reason that causes TN is trigeminal ganglion degeneration instead of nerve root pathology [4]. Also, TN occurs as a result of primary cranial diseases, such as intracranial neoplasm or any other space-occupying lesion, multiple sclerosis, and head trauma. The remainder of TN cases are classified as idiopathic; therefore, this study was conducted to highlight and explain the cause of the occurrence of idiopathic TN.
Local anesthesia is usually harmless in dental practice for healthy people as it acts by inhibiting the excitation and conduction process in peripheral nerves at a normal dose. However, its high doses or concentrations may cause poisonous effects on the neural tissues, neuromuscular junction, cell metabolism, and cardiovascular system. Different neurological problems occurring postoperatively have been recognized to be a result of the cytotoxicity of LA, but the essential mechanisms are still vague. A detailed medical investigation may disclose a variety of symptoms and signs of neuropathological distress, like dysesthesia, allodynia, hypoesthesia, impulsive electrical shock, and defects associated with gustation [2, 5].
Numerous theories have been projected to describe the reduced or failed effect of LA in tissues, producing acute inflammation. These include a fall in the pH of the anesthetic, thus leading to an ionized formula having a lesser action; a rise in the vascularity of the inflammatory region, thus leading to quick elimination of the LA from the place of injection [6]; an increase in extracellular fluid due to increased vascular permeability in inflammatory tissues, leading to dilution of the LA solution; and the occurrence of inflammation altering the sensory nerve activities and ion channels to probably cause afferent nerve hyper-excitability or hyperalgesia [7]. Furthermore, there was reported a reduction in the lidocaine’s inhibitory effect via the production of peroxynitrite by inflammatory cells, thereby leading to the failed effect of LA in the inflamed tissues [8]. The above reasons may enable dentists to consider repeating or increasing the dose of LA to achieve analgesia for performing dental operations, thus reducing the neuro-pathological problems that may happen. Therefore, the aim of this cross-sectional study was to assess the correlation between idiopathic trigeminal neuralgia and local anesthetic overdose and/or repeated injections caused by dental malpractice.
2. PATIENTS AND METHODS
2.1. Study Design and Participants
This cross-sectional study was conducted to highlight the reasons for idiopathic TN and the use of high doses of LA (2% lidocaine) in dental clinics due to repeated injections after the failure of analgesia in the presence of acute inflammation at injection sites. The data were obtained from dental offices that included a history of disease from patients and symptoms of the disease after previous dental treatment. The patients complaining of dysesthesia and then TN were observed for several days following the dental operations. The investigations and recording of dental histories led to suggestions regarding the reasons for the occurrence of this disease and its relation to LA injections in the inflamed area. The targeted population or participants included an adequate sample of thirty-four patients (27 males and 7 females), selected from the teaching clinic of oral medicine at the College of Dentistry, the University of Karbala. The sample was collected from February 2015 to March 2021. The ages of patients ranged from 25 to 71 years, with a mean age of 49.3.
2.2. Inclusion and Exclusion Criteria
A sample of 53 patients complaining of dysesthesia, allodynia, and different types of TN was initially sought to be included in the study. 19 patients were excluded from this study because they did not match the inclusion criteria; in addition, some of them did not agree to participate in the study, while the remaining 34 patients were found to match the inclusion criteria. The inclusion criteria were as follows: no intracranial diseases, including neurological diseases and vascular malformation; absence of any organic diseases causing orofacial pain; the symptoms matching the International Headache Society (HIS) diagnostic criteria for TN; the presence of data for past dental treatments, including the type of dental infection in the treated tooth along with the number of LA carpules injected, and good response to carbamazepine, which has been prescribed by other dentists or neuro-physicians as it has been established to be a diagnostic and successful treatment for most cases. Therefore, the good response to this medication was considered as additional confirmation for the diagnosis [9, 10]. It was difficult to collect a large number of patients suffering from idiopathic TN and select a sample out of them to conduct the cross-sectional study because most of these patients look for help or treatment in the neuro-medicine clinics, and many of them lack dental history regarding their dental treatment prior to the attack. Therefore, this study took a long period of time and involved a limited number of patients.
2.3. Diagnostic Criteria
34 patients included in this study were subjected to complete diagnosis by using International Headache Society (HIS) diagnostic criteria [11] for TN, as listed in Table 1, to ensure that all patients complained of idiopathic TN. The patients' symptoms were found to fit the criteria of the classical type of TN but without any arterial compression on the trigeminal nerve root, so this study used these criteria to diagnose the patients with idiopathic TN.
| A. Paroxysmal episodes of orofacial ache remain from several seconds to several minutes, disturbing one or more branches of the trigeminal nerve. |
| B. Orofacial pain includes the two features listed below:1. Sudden, sharp, superficial, or stabbing pain.2. Triggered by stimulation of the trigger point. |
| C. Attacks are stereotyped in the individual patient. |
| D. There is no clinical obviousness for any neurologic diseases. |
| E. There is no correlation to any systemic disorders. |
2.4. Oral and Neurological Examinations
The patients were subjected to a thorough oral examination by two oral physicians to exclude any organic diseases that cause orofacial pain and to decrease the bias in diagnosis. Then, the patients were subjected to a medical examination by multiple neurologists using magnetic resonance imaging and other medical investigations to ensure that all patients were not suffering from brain tumors, multiple sclerosis, or vascular malformations (most commonly the superior cerebellar artery).
2.5. Case Sheet and Data Collection
The case sheet of this study was used to record the information related to medical and dental history to collect data regarding age, sex, number of trigger zones, site of trigger zones, number of LA carpules, duration of disease, dental extractions, root canal therapy, pulpotomy, and history of periapical pathology due to dental infection that leads to inflammation. Most of the dental infection data during dental treatments were collected from dental offices after the acceptance of both the dentists and the patients.
2.6. Analysis of Data
The data were analyzed to sort the patients into the categories of age, sex, number of trigger zones, site of trigger zones, duration of TN pain, and dental procedures under acute inflammation conditions, and then the data were statistically analyzed to discuss the correlation between LA overdose and idiopathic TN. The data of the studied sample were analyzed by using the statistical package for social sciences (SPSS) version 25. Descriptive statistics are presented in tables and bar charts in terms of mean, standard deviation, frequencies, and percentages. All continuous variables were tested for statistically normal distribution by using the normal distribution curve, and statistical tests were applied according to the distribution and type of variables. The chi-square test was used to compare the frequency distribution between two groups for categorical qualitative data. A level of significance at 0.05 was considered a significant difference or correlation.
3. RESULTS
The patients were statistically distributed into two sub-groups according to their age and sex data, as shown in Table 2. The first group (25-48 years old) represented 52.94% of all patients, and the second group (49-72 years old) included 47.06% of patients. While the percentage of disease according to sex was 79.4% for males and 20.6% for females. The data collected for the long term revealed TN to be a common disease in the adult and elderly male patients, so the age results matched the findings of the epidemiological studies, while the sex results were found to differ [12].
| Items | Sub-groups | Study GroupTotal = 34 | |
|---|---|---|---|
| Frequency | Percentage | ||
| Age/Years | 25-48 | 18 | 52.94 |
| 49-72 | 16 | 47.06 | |
| Sex | Male | 27 | 79.4 |
| Female | 7 | 20.6 |
As presented in Table 3, the chi-square test was used to test the effect of this type of dental procedure before pain on the two age groups and the two sex groups. For the age group, the difference was significant (p-value < 0.05), which indicated an increased incidence of nerve damage caused by local anesthesia in older patients. For the sex group, the chi-square test value was 2.45, indicating no significant difference (p-value > 0.05).
| Demographic Data | Chi-square | Contingency Coefficient | Significance(P-value > 0.05) |
|---|---|---|---|
| Age | 19.8 | 0.65 | 0.02 |
| Sex | 2.45 | 0.29 | 0.34 |
The duration of the disease (Table 4) was measured in months, and it was sorted into three sub-groups. The largest percentage of patients was recorded in the sub-group of 3 months with 47.1% percentage, while the lowest percentage (23.5%) was recorded in the sub-group of 12 months. More patients were found in the sub-group with 3 months’ duration of the disease than the others, and due to the short disease term, these patients remembered their history and provided the data with respect to the initiation of the disease and type of dental treatment along with the number of LA carpules administered.
The attacks of TN originate via the non-painful physical stimulus of definite zones (trigger points), which are located on the same side of the orofacial pain. When the episode is finished, usually there is a refractive time during which the stimulus to the trigger point does not prompt the orofacial pain. Most of the patients (94.1%) were found to have one trigger point, while the percentage of patients with two trigger zones was 5.9%, as shown in Table 4. The location of the trigger zone has been classified into intraoral, which was found to be less common, i.e., in 5.8% of cases, and extraoral, which was estimated to be in 100% of cases due to the fact that there were two cases with double trigger points, intraoral and extraoral. The nasolabial trigger zone was recorded in 85.2% of the patients, while the infraorbital trigger zone was recorded in 14.7% of the cases. All the trigger points were located in the upper jaw, as shown in Table 4, so these results may explain the effect of direct contact between the LA technique achieved by infiltration and the infected maxillary teeth. Therefore, all the patients collected had the upper jaw trigger zone rather than the lower jaw trigger zone. As shown in Table 5, there was a significant correlation (p-value < 0.05) recorded between dental procedures before pain and the clinical data of pain after the dental procedures in terms of the number of trigger zones of pain. While the chi-square test was non-significant for the duration of the disease by months and the site of trigger zones.
| Items | Sub-groups | Study GroupTotal = 34 | |
|---|---|---|---|
| Frequency | Percentage | ||
| Number of trigger zones | One | 32 | 94.1 |
| Two | 2 | 5.9 | |
| Duration of the disease (months) | 3 | 16 | 47.1 |
| 6 | 10 | 29.4 | |
| 12 | 8 | 23.5 | |
| Site of trigger zones | Intraoral | 2 | 5.8 |
| Extraoral | 34 | 100 | |
| Nasolabial | 29 | 85.2 | |
| Infraorbital | 5 | 14.7 |
| Demographic Data | Chi-Square | Contingency Coefficient | SignificanceP-value |
|---|---|---|---|
| Number of trigger zones | 6.23 | 0.64 | 0.04 |
| Duration of the disease (months) | 0.18 | 0.07 | 0.99 |
| Site of trigger zones | 0.07 | 0.04 | 0.96 |
| Items | Sub-groups | Study Group (Total = 34) | |
|---|---|---|---|
| Frequency | Percentage | ||
| History of dental extraction or operative procedure before the pain | Extraction | 17 | 50 |
| Pulpotomy | 9 | 26.47 | |
| Endodontic | 8 | 23.5 | |
| Percentage of premolar teeth | Premolar teeth | 17 | 50 |
| Percentage of molar teeth | Molar teeth | 15 | 44.11 |
| Percentage of anterior teeth | Anterior teeth (canine) | 2 | 5.88 |
As presented in Table 6, the dental history of the 34 patients reported 50% of patients to have undergone an extraction of multiple teeth, mostly the upper premolars, and the upper molars, and a few treatments have been done for upper canine extraction (5.88%). Pulpotomy procedures have been reported in 26.47% of the patients, and 23.5% of the patients have reported to have undergone root canal therapy. All these dental procedures have been done on the upper teeth only, from the canine to the third molar teeth, indicating an increased percentage of premolar teeth in 50% of all cases. Some of the patients have reported to have a history of multiple dental procedures at the same appointment or for a short period of time (several days) between the first and second visits, such as dental extraction with root canal therapy. The high incidence of TN pain due to dental extraction (50% of patients) in this study may be due to the fact that dental extraction requires a higher dose of LA injections than root canal therapy and pulpotomy, and the failure of the effect of LA in these infected teeth leads the dentist to repeat the LA injections in order to achieve analgesia.
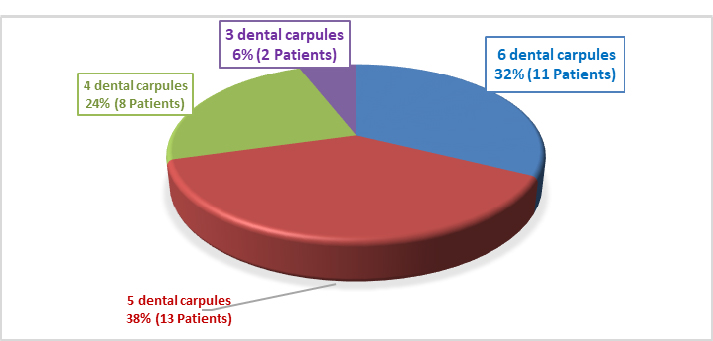
Information has been obtained from the dentists and/or study participants about the number of injections of LA given to each patient, and the type of LA administered has been reported to be lidocaine (2%) along with epinephrine, as listed in Fig. (1). A large group of patients (13) have received 5 dental carpules, while a small group, i.e., 2 patients have received 3 dental carpules.
3.1. Practical Methodological Considerations
As Haas and Gaffen [13], Haas [14], and Jensen and Hillerup [15, 16] have investigated and described, the reason for trigeminal nerve injury is associated with LA administration, as LA injections in dentistry to acute inflammation sites is methodologically difficult. Moreover, the neurotoxicity and neuro-injury associated with local anesthetic injections by infiltrations into the acutely inflamed jaw bone due to dental infections are probably difficult and underreported. The risk and severity of trigeminal neuralgia may cause difficulties in treatment and relapse in some cases, and the necessary number of participants in the experiment and control groups would thus be unrealistic. Therefore, the investigators need to depend on further procedures, such as long open observational recordings of idiopathic TN cases [17], animal experiments [18], research related to the neurotoxicity of LA in neurons [19], and research related to the neurotoxicity of a high dose of LA to the inflamed site of jaw bones during repeated injections after the failure in the effect of local anesthesia.
The limitations of the study are as follows: the collection of data took a very long time (approximately seven years), and hence, all patients were not thoroughly examined to exclude intracranial causes. Moreover, the recording of dental infection history before the nerve injury or damage by multiple local anesthesia injections was difficult and tiring as some of the patients did not have data regarding dental operations, some patients did not agree to participate, and some dentists did not agree to give information about the dental operations, the presence of dental infection at the time of operation, and the number of dental LA given to the patients.
4. DISCUSSION
This study has focused on a new non-conventional reason for the occurrence of trigeminal neuralgia, which is an extracranial cause that initiates the TN rather than the intracranial causes and trigeminal nerve root demyelination of the TN. The addition of the local trigeminal nerve branch neuropathy concept is due to the malpractice of local anesthetics (LA) in dentistry by some dentists, which includes both the use of high concentrations of local anesthetics (LA) and/or repeated injections of them in some pathological conditions in the oral cavity, such as acute periapical abscess or cellulitis due to dental infection.
Some dentists need to induce local anesthesia to perform multiple dental operations, such as dental extraction and conservative treatments, but they face some difficulties, such as failure of analgesia, especially in some painful cases, including acute pulpitis, acute periapical abscess, and cellulitis, in which the dentist tries to relieve the pain at the first visit. Therefore, they try to achieve analgesia by increasing the dose and injections of LA to manage these painful cases despite the post-pathological risks, such as neurotoxicity and the spread of infections. The failure of local anesthesia at the infected sites in the oral cavity mainly occurs upon using the local infiltration techniques in the upper jaw, which makes the dentists give repeated injections to achieve the analgesia that might cause maxillary branch neurotoxicity or neuropathy, thus eliciting the trigeminal neuralgia.
Numerous studies have indicated neurotoxicity to be associated with the concentration and dose of LA, as lidocaine and articaine solutions with 4% of concentration have indicated significant neurotoxicity compared to the lesser concentration solutions [20-22]. An experimental study in 1986 on the effect of multiple lidocaine infusions on the rat peripheral nerve demonstrated an infusion of 1 to 4% lidocaine in volume given 3 times per day for 3 days to be enough to inhibit motor nerve function [21]. In the above study, the researchers gave 4% lidocaine solution 3 times per day for 3 days without the presence of inflammation. On the other hand, the patients in this study were exposed to 3 to 6 dental carpules of the same LA (lidocaine) in a short period of time in the presence of dental infection (inflammation) at the sites of injections; thus, the possibility of neurotoxicity in this study has been greater.
Several studies have suggested the injury or pathology of the trigeminal nerve to be correlated to LA injections as a block technique [23-26]. Evidence indicates that the recurrence of inferior dental block injections may raise the danger of damaging the trigeminal nerve, and it may be a direct trauma caused by a needle or indirect neurotoxicity caused by a high concentration of LA [17]. Repeated blocks for an inferior alveolar nerve are most likely necessary because this nerve is not adequately anesthetized in many dental procedures, such as dental extraction and acute pulpitis in upper and lower molar teeth. Surely, increasing the LA concentration may increase the neurotoxicity in vitro despite that it can be administered in vivo by infiltration and block techniques [27, 28]. The researches conducted by Haas and Lennon [5], Hillerup and Jensen [15], and Gaffen and Haas [13] propose that highly concentrated (4%) solutions of LA are more likely to produce nerve injury or damage. Despite this fact, many dentists insist on using a high concentration of LA (4%) in their clinics to achieve high analgesia for a long duration. Some dentists may need to give a high dose or repeated injections of LA to patients to obtain the perfect analgesia in the inflamed tissue after the failure of the first LA injection. The failure of analgesia may be due to different biomechanical theories that have been projected for an explanation of lowering LA effects in the existence of inflammation [29, 30]. However, some researchers state that the acidity arising from inflammation is not significant enough to reduce the LA's effectiveness as documented above, but it may be due to the presence of peroxynitrite involved in the inflammatory process, which may interact with the LA, altering its pharmacological actions [8].
There are different opinions regarding the etiology of trigeminal nerve damage or injury by LA injection, and no proof can be established for each opinion. Pogrel et al. [31] proposed three theories as follows: mechanical trauma produced by a sharp needle to the nerve conductive tissue; mechanical damage producing intraneural hemorrhage, leading to the creation of granulation tissue and hematoma with constrictive scarring; hypoxia that may generate pressure on the nerve tissue [31, 32]. The first mechanical trauma theory does not match the results of this study because the patients included in this research may have local neuropathy due to the neurotoxicity of an overdose of LA injections infiltrated to the upper jaw without direct trauma (needle injury) to the nerve tissue as occurring in the inferior dental block and mental injections. The majority of TN cases occur in the maxillary nerve branch, so all the patients in this study complained of maxillary trigger zones [33]. The third theory states that the LA dose may cause degeneration along with neurotoxicity of myelin or axon cellular structures or both [15, 22, 31, 34]. Indeed, there is another theory of thrombosis or coagulation as the reason for neuropathy due to repeated overdose of LA at the site of inflammation, which states that the inflammation initiates clotting, damages the fibrinolytic system, and decreases the normal anticoagulant activity, so the cytokines released during the process of inflammation are the main mediators involved in activating the coagulation system [35]. Hence, depressed regulation of the anticoagulant pathway does not stimulate thrombosis only, but also magnifies the route of inflammation. The interactions of coagulation and inflammation may overcome the normal defense system. Normal anticoagulant mechanisms block the thrombotic response; however, these paths are decreased or lowered by inflammatory messengers, which promote inflammation. Hence, the dental infection reported in the patients of this study might be the cause of multiple injections of LA that may have caused more thrombosis in the region of superior alveolar dental nerves, making that region suffer from hypoxia and neuropathy subsequently.
The main suggested theory regarding the cause of the local neuropathies and the theory that almost coincides with this study with respect to the initiation of TN is the demyelination of the nerve [36] and the neurotoxic effects of LA due to high concentrations and prolonged exposure times (repeated injections at the site of the dental infection after failure of LA), which may activate the intrinsic pathway of apoptosis through cytochrome C release. The local anesthetic-related neurotoxicity has harmful effects on the nerve tissue, including demyelination and axonal degeneration [21, 34, 37]. Indeed, some patients who have received LA in an inflamed dental area caused by dental infections, either the first or second premolar, may undergo mental nerve neuropathy, and this may be demonstrable by variable grades of dysesthesia and hyperalgesia, which may over time transform into an electrical shock (trigeminal neuralgia).
The occurrence of dysesthesia in different areas of the oral cavity, such as the lingual nerve, after inferior dental block injections (4% prilocaine and 4% articaine), has been recorded in 89% of cases in the United States [28]. Rapid nerve cell death may be caused by LAs because of cell necrosis. Bupivacaine and lidocaine may prompt apoptosis by increasing their concentration or increasing the period of contact with nerve tissue, and these properties might correlate to nerve injury postoperatively. Lidocaine is associated with the maximum prevalence of temporary neuropathological symptoms, but it is not the greatest toxic LA, while bupivacaine, a medicine producing a very low occurrence of temporary neurological symptoms, has been reported as the greatest toxic LA in our cell model. These facts propose that nerve pathology is caused by cytotoxicity and may involve diverse tools for different LAs and different target(s) rather than neurons [19].
Further, studies on animals carried out by various investigators have determined the neurodegenerative features of this disease, for example, axonal degeneration and nerve demyelination, which have been related to a variety of preparations of LAs, and these have allowed the researchers to well recognize the essential mechanisms of neurotoxicity. In addition to the reversible blockade of Na+ channels and nerve transmission produced by LAs, several effects at the cellular level have also been identified. The results of in vivo and in vitro researches show cytotoxic properties of LA necrosis and pro-apoptotic events caused by LA [36].
CONCLUSION
The malpractice of local anesthesia in dentistry may lead to dysesthesia, allodynia, and idiopathic trigeminal neuralgia with different degrees and severity due to the neurotoxicity of a peripheral nerve fiber caused by repeated LA and/or a high dose of it despite the type of LA. The nerve damage may occur in many forms, such as demyelination, apoptosis, axonal degeneration, and hypoxia due to thrombosis. The proximity or direct contact between the maxillary infiltration techniques of LA and the site of inflammation in patients receiving a high dose of LA can cause damage to the nerve or the possibility of neurotoxicity, and it may explain why the most common site of trigger points is the second trigeminal branch (maxillary nerve). So, dentists should recognize the risk of repeated injections or high-dose solutions (4%) of LAs in the inflamed tissues when inducing analgesia for their dental operations as they may initiate the primary (idiopathic) trigeminal neuralgia.
LIST OF ABBREVIATIONS
| TN | = Trigeminal neuralgia |
| LA | = Local anesthesia |
| LAs | = Local anesthetics |
| SPSS | = Statistical package of social sciences |
| HIS | = International headache society |
ETHICS APPROVAL AND CONSENT TO PARTICIPANTS
This study was approved by the Ethics Committee of the College of Medicine/University of Kerbala (no. 83).
CONSENT FOR PUBLICATION
All participants provided their informed consent and voluntarily participated in the study.


