All published articles of this journal are available on ScienceDirect.
Transalveolar Sinus Lift and Implant Site Preparation using Motorized Threaded Bone Expanders: A 2-year Retrospective Study
Abstract
Background and Objectives:
The pneumatization of the maxillary sinus presents serious challenges to the dentist, and the management of such cases is essential for the rehabilitation of the posterior maxilla.
The aim of this study was to evaluate the clinical and radiographic outcomes of using motorized threaded bone expanders in transalveolar sinus lift procedures.
Materials and Methods:
This retrospective study was conducted on patients presented to the Department of Oral and Maxillofacial Surgery at Tishreen University who had transalveolar sinus lift using motorized threaded bone expanders with simultaneous dental implant placement between January, 2020, and August, 2022. The patients were followed up regularly for six months until loading. Statistical analyses were performed to assess intrasinus bone gain, marginal bone loss, implant diameter, and insertion torque. The correlation coefficient was used to measure the relationship between marginal bone loss and insertion torque value.
Results:
Three membrane perforations were observed in 34 procedures (8.82%). The survival rate for all implants was 100%. The main insertion torque was 32.58 N.cm. The mean intrasinus bone gain was 1.69 ± 0.44 mm. The mean marginal bone loss was 0.27 mm. The difference between IBH and bone height after 6 months showed a statistically significant difference. No correlation was found between marginal bone loss and insertion torque value.
Conclusion:
According to the results of this study, transalveolar sinus lift using motorized bone expanders showed effective lifting of the sinus floor with minimum marginal bone loss, thus presenting a good solution for pneumatization of the maxillary sinus to achieve a successful rate for implant placement.
1. INTRODUCTION
The posterior maxilla presents several constraints for dental implant placement due to the limited residual bone height and poor bone quality. Insufficient alveolar bone height is attributed to alveolar bone resorption and increased sinus pneumatization following tooth loss [1].
A sinus augmentation is the most frequently executed pre-prosthetic technique to attain an adequate bone volume in the atrophic maxilla [2, 3]. This predictable technique is employed to address the loss of vertical bone height in the posterior maxilla. Moreover, it can be performed using two common techniques: the lateral window approach and the transcrestal approach [4].
In 1986, Tatum performed a sinus lift, which used a transalveolar approach to the sinus; the sinus membrane was dissected by fracturing the sinus floor using special tools called “socket former” [2]. In 1994, Summer introduced a less aggressive approach to sinus floor elevation, which involved the immediate placement of implants and is commonly referred to as Osteotome Sinus Floor Elevation (OSFE) [3, 4]. This technique has been modified by many researchers to make the procedure more comfortable for the patients and easier for the practitioners. Furthermore, it is also used to reduce the risk of membrane perforation and increase intrasinus bone gain [5-8].
Threaded bone expanders are the instruments used to spread out a dental implant osteotomy. They are used as an alternative to osteotomes in cases of expansion of the atrophic alveolar ridge [9, 10]. Several studies confirmed the superiority of threaded bone expanders over the osteotomes in the expansion and splitting of the alveolar ridge [11, 12].
The threaded bone expanders are also used for rehabilitation of the posterior maxilla as an alternative to sinus lift techniques in the atrophic maxilla. The implant bed can be safely prepared near the anterior wall of the maxillary sinus. This technique is called the “sinus bypass technique” [13].
The properties of these expanders impetus the practitioners to employ them in transalveolar sinus lift [14-16]. The specific aims of the study were to evaluate the bone gain, the intra- and post-operative complications rate, the implant success rate and marginal bone loss in transalveolar sinus lift using threaded bone expanders and analyze the correlation between marginal bone loss and insertion torque in transalveolar sinus floor elevation (TSFE) procedures using motorized threaded bone expanders without bone graft materials.
2. MATERIALS AND METHODS
2.1. Study Sample and Design
This retrospective study was approved by the Ethics Committee of Tishreen University and was conducted in accordance with the Declaration of Helsinki for Human Studies. This study was conducted on patients who presented to the Department of Oral and Maxillofacial Surgery at Tishreen University and who had transalveolar sinus lift using motorized threaded bone expanders with simultaneous dental implant placement between January, 2020, and August, 2022. The patients were informed about the details of the surgery, and all subjects gave their written informed consent for inclusion prior to the study. Patient files were carefully reviewed to identify individuals who met the following inclusion criteria.
2.1.1. Inclusion Criteria
1- an edentulous in the posterior region of the maxilla. 2- initial bone height (5-8) mm, 3- Cone Beam Computed Tomography (CBCT) scans available before and 6 months after transalveolar sinus lift, 4- transalveolar sinus lift using motorized threaded bone expanders with simultaneous dental implant placement.
2.2. Surgical Procedure
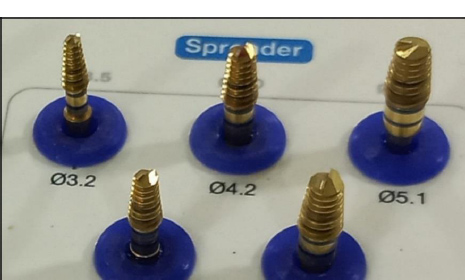
The kit used in this study (Sinus Lift Kit; Cowellmedi Inc, South Korea) included five conical threaded bone spreaders with different diameters. The tip of the spreaders had U shape blade (Fig. 1).
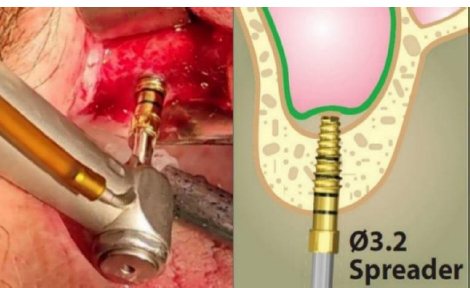
All surgical procedures were performed by the same surgeon under local anesthesia with 2% lidocaine and 1:100,000 epinephrine. A full-thickness flap was raised to expose the alveolar ridge. The implant bed was first prepared with a 2.2 mm pilot drill. The drill depth reached approximately 1 mm below the sinus floor. The preparation of the implant bed was then continued with a 2.9 twister drill. Transalveolar sinus lift was first performed using a 3.2 mm spreader at 50 rpm (Fig. 2). The amount of lifting and implant length were planned previously. The preparation of the osteotomy site was then continued with larger diameter spreaders until reaching the planned diameter. Valsalva maneuver was used to examine the integrity of the sinus membrane. The implant was inserted using a motorized handpiece. All implants were inserted to be at the level of crestal bone (upper surface of the implant's shoulder at the level of crestal bone). The flap was closed with 4-0 silk sutures. Sutures removal was done after 1 week.
2.3. Measurement of Insertion Torque
All implant bed preparation procedures were performed using an advanced implant motor (DTE Implanter; Woodpecker; China) (Fig. 3). The torque was controlled at 50 N.cm as a maximum insertion torque value to prevent it from being exceeded. The implant was inserted via a motorized handpiece. The torque value on the motor screen increased as the implant was inserted further into the bone. The insertion torque value on the motor screen was recorded when the implant reached the level of crestal bone.

2.4. Radiographic Measurements
The following variables were assessed using CBCT scans that were taken preoperatively and 6 months postoperatively:
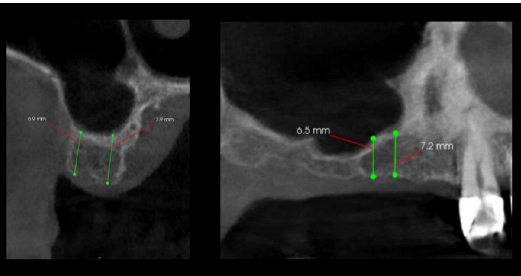
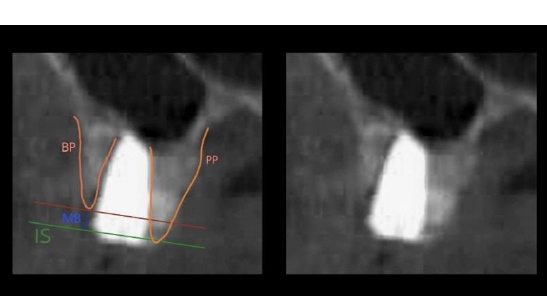
Initial bone height (IBH) was measured at preoperative CBCT as the distance between the alveolar bone crest and sinus floor at the planned implant placement site in four aspects: medial, distal, buccal and palatal. The mean height was calculated for these measurements (Fig. 4).
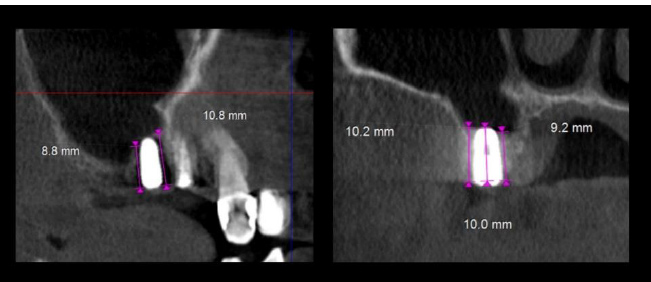
Bone height after 6 months was measured at postoperative CBCT as the distance between the implant's shoulder and the new sinus floor at the same site in four aspects: medial, distal, buccal and palatal. The mean height was calculated for these measurements (Fig. 5).
Intra-sinus bone gain was measured as the difference between bone height after 6 months and initial bone height.
Marginal bone loss was measured at postoperative CBCT as the distance between the implant's shoulder and alveolar bone crest in four aspects: medial, distal, buccal and palatal. The mean height was calculated for these measurements (Fig. 6).
2.5. Statistical analysis
Statistical analysis was performed using the statistical software package SPSS (Version 23.0, Armonk, NY, USA). Descriptive statistics included mean and standard deviations to assess initial bone height, bone height after 6 months, intrasinus bone gain, marginal bone loss, implant diameter, and insertion torque. The bone height differences between periods were assessed with a paired t-test. The correlation coefficient was used to assess the relationship between the marginal bone loss and the insertion torque.
3. RESULTS
3.1. Patient Characteristics
This retrospective study was done on 29 patients (18 males, 11 females) with an average age of 46.2 years (range, 37–57 years) who met the inclusion criteria for this study.
3.2. Clinical Analysis
A total of 34 implants were placed using motorized threaded bone expanders. The survival rate for all implants was 100%. The mean insertion torque was 32.58 N.cm (range, 24–41 N.cm) (Table 1). Three-membrane perforations were observed in 34 procedures (8.82%). No other intraoperative complications were observed.
| - | Bone Gain | Marginal Bone Loss | Insertion Torque | Implant Diameter |
|---|---|---|---|---|
| Mean | 1.69 | 0.22 | 32.58 | 4.42 |
| SD | 0.44 | 0.38 | 0.63 | 0.47 |
| Max | 2.62 | 1.1 | 41 | 5 |
| Min | 0.6 | 0 | 24 | 3.5 |
3.3. Radiographic Analysis
The initial bone height ranged from 5.1 to 7.8 mm with a mean of 6.37 ± 0.85 mm. The bone height after 6 months ranged from 6.8 to 9.7 mm, with a mean of 8.08 ± 0.89 mm. The intra-sinus bone gain ranged from 0.6 to 2.6 mm with a mean of 1.69 ± 0.44 mm (Table 1).
The difference between the initial bone height and the bone height after 6 months showed a statistically significant difference (P< 0.001) (Table 2).
| - | Initial Bone Height | Bone Height after 9 Months | Paired T-Test | P-Value |
|---|---|---|---|---|
| Mean | 6.37 | 8.08 | 21.32 | < 0.001 |
| SD | 0.85 | 0.89 |
3.4. Marginal Bone Loss in Relation to Insertion Torque
The marginal bone loss 6 months postoperative for the 34 implants included in the study ranged from 0 mm to 1.1 mm with an average of 0.22 ± 0.38 mm. Pearson correlation analysis showed that marginal bone loss was not significantly correlated with the insertion torque values (p value > 0.05).
4. DISCUSSION
Maxillary sinus augmentation aims to increase the vertical bone height in the posterior maxilla for dental implant placement. Various techniques and materials have been used in this procedure, which can be divided into lateral approaches and transalveolar approaches [17].
Lateral sinus augmentation has become a common and predictable procedure to increase bone height for dental implant placement in the posterior maxilla. However, the procedure is described as sensitive and requires surgical skill, particularly in Schneiderian membrane dissection. Studies have demonstrated that Schneiderian membrane perforation is considered the most frequent complication, with reported incidence rates ranging from 7 to 60% [18, 19].
The transalveolar sinus lift approach is described as less invasive and more conservative than the lateral approach. Osteotome sinus floor elevation (OSFE), which was introduced by Summer in 1994, was the first and standard transalveolar sinus lift technique [20, 21]. This technique uses tapered osteotomes and a hammer for green-stick fracturing of the sinus floor. Several studies have reported that hammering might result in postoperative vertigo and decrease the patients’ comfort [22]. Several alternative methods have been introduced in recent years to alleviate this issue. The addition of bone graft materials can contribute to absorbing the shock caused by hammering and decreasing the Schneiderian membrane perforation rate [23, 24].
Transalveolar sinus lift using sequential special drills, such as the cosci technique and osseodensification technique, is based on gradual perforation of the sinus floor instead of fracturing it [8, 25, 26]. Therefore, osteotomes and hammering are eliminated. Hydraulic pressure techniques have also been introduced as minimally invasive transalveolar sinus lift techniques without osteotomes [27, 28]. However, non-osteotome-based transalveolar techniques are intricate procedures that necessitate a high level of surgical proficiency, primarily because these methods involve direct contact of instruments with the delicate sinus membrane [25-28].
Threaded bone expanders have demonstrated the capacity to effectively and safely move the cortical plate of the sinus floor, similar to Summer's technique and without using the hammer [15].
Controversy persists regarding the essentiality of bone grafting in conjunction with the placement of dental implants during transalveolar sinus lift. Several studies reported the possibility of bone formation in sinus lift procedures with simultaneous dental implant placement without using bone graft material [29-31]. This can be explained by the implant fixture acting as a tenting pole for space maintenance beneath the Schneiderian membrane [32]. Nonetheless, upon contrasting the amount of intrasinus bone gain between the grafted group and the non-grafted group, it was observed that the grafted group exhibited a more significant degree of bone gain compared to the non-grafted group [33].
A systematic review [34] reported a mean intrasinus bone gain of 3.43 ± 0.09 mm, which was inconsistent with our results (IBG was 1.69 mm). This might be explained by the confirmed relationship between bone gain (IPL) and implant protrusion length (the mean of IPL in our study was 2.01 mm). This also explains the difference in intrasinus bone gain between our study and a study conducted by Kadkhodazadeh [15], who used the same surgical protocol.
High insertion torque values are associated with greater primary stability of dental implants and thus improve osteointegration [35, 36]. However, high insertion torque can generate micro cracks that could result in the progression of marginal bone loss [37]. A systematic review [38] and meta-analysis reported no association between insertion torque value and implant marginal bone loss, which is consistent with our results.
This is the first study that evaluated the motorized threaded bone expander without bone grafting materials in transalveolar sinus lift procedures. The previous study evaluated the bone expanders in transalveolar sinus lift procedures using bone graft materials or a manual method. The limitations of the study are 1- no control group and 2- no follow-up period after the functional loading.
CONCLUSION
According to the results of this study, transalveolar sinus lift using motorized bone expanders showed effective lifting of the sinus floor, and minimum marginal bone loss presented a good solution for pneumatization of the maxillary sinus to achieve a successful rate of implant placement.
LIST OF ABBREVIATIONS
| OSFE | = Osteotome Sinus Floor Elevation |
| TSFE | = Transalveolar Sinus Floor Elevation |
| TSFE | = Transalveolar Sinus Floor Elevation |
| IBH | = Initial bone Height |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This retrospective study was approved by the Ethics Committee of Tishreen University, Syria (Ethical Permission No. 707 on 17-12-2019).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patients for publication of this study.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author, [Z.A], on special request. The data supporting the findings of the article is available in the [Zenodo] at [zenodo.org], reference number [Doi:10.5281/zenodo.8251821].
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise
ACKNOWLEDGEMENTS
Declared none.


