Comparative Analysis of Methods for Surgical Treatment of Ankyloglossia: A Review Article
Abstract
Aim:
Ankyloglossia is a congenital oral anomaly characterized by a short frenulum of the tongue, which can cause nutritional, speech, and developmental problems. The limited movement of the tongue may lead to the development of various anomalies of dentition. Thus, the purpose of this work is to compare the existing methods for surgical treatment of ankyloglossia that involve either laser technologies or scalpels.
Methods:
We analyzed literature sources about patients with ankyloglossia treated with various surgical methods, such as the use of a scalpel, diode laser, CO2 laser, Er:YAG laser and Nd:YAG laser.
Results:
The results showed that lasers have multiple advantages over the scalpel: bloodless surgery, which provides good visualization of the surgery field; no need for suturing; the reduction of inflammation and pain in the postoperative period due to the bactericidal properties of the laser; minimal or no scar tissue; decreased surgery time.
Conclusion:
Thus, the laser technique is an alternative to conventional surgery, and, considering the upper mentioned benefits, it can be stated that the laser beam is more effective than a scalpel or scissors.
1. INTRODUCTION
Ankyloglossia, or tongue-tie, is a congenital anomaly, in which a child is born with a short and/or thick lingual frenulum, which limits the tongue’s movement (Fig. 1). This affects the mechanism of fixation and sucking during breastfeeding of infants, and later, in childhood and adulthood, often causes problems associated with the psyche of children and their cognitive behavior [1-4]. Ankyloglossia makes it difficult to articulate some sounds, which leads to difficulties with speech and general development [5, 6]. If this pathology is not diagnosed in a timely manner, this disorder can lead to the development of various pathologies, e.g., atypical swallowing, oral breathing, and sleep disturbance in childhood and adolescence [7, 8]. A short frenulum can also contribute to the development of anomalies in the dental system. These include a decrease in the size of the upper respiratory tract; the formation of an open bite; periodontal diseases (deep destruction of the supporting structures of the parodontium on the lingual side of the incisors, gum recession), shortness of breath due to displacement of the epiglottis forward [9-11]. In addition to these problems, a defective lingual frenulum can contribute to increased plaque formation, which negatively affects oral health [12, 13]. A short lingual frenulum is an obstacle to lifting the tongue, which results in the narrowing of the upper jaw due to the lack of transverse growth and the development of a cross-bite in some cases or abnormal growth of the lower jaw in others. In some patients, a short and hypertrophied lingual frenulum can lead to a diastema between the central incisors of the lower jaw [14]. In old age, a highly attached frenulum of the tongue on an edentulous jaw worsens the fixation of a removable prosthesis.

A classification of ankyloglossia was proposed by Kotlow L.A. in 1999 [15]:
Class I: Mild ankyloglossia: 12 to 16 mm;
Class II: Moderate ankyloglossia: 8 to 11 mm;
Class III: Severe ankyloglossia: 3 to 7 mm;
Class IV: Complete ankyloglossia: Less than 3 mm.
There is also another classification of ankyloglossia by Coryllos [16]:
Type I: Fine and elastic frenulum; the tongue is anchored from the tip to the alveolar ridge, and it is found to be heart-shaped;
Type II: Fine and elastic frenulum; the tongue is anchored 2-4 mm from the tip near the alveolar ridge;
Type III: Thick, fibrous non-elastic frenulum; the tongue is anchored from its middle to the floor of the mouth;
Type IV: The frenulum cannot be seen but palpated; it has a fibrous and/or thick and shiny submucous anchoring from the base of the tongue to the floor of the month.
To correct ankyloglossia, a surgeon dissects the frenulum (frenotomy) or excises it (frenectomy), and moves the frenulum attachment site apically and/or laterally to the gingival margin (frenuloplasty). Frenectomy can be performed with a laser, scalpel, or surgical scissors, although, according to some authors, excision of the lingual frenulum with laser radiation is more effective [6, 13, 17]. Often, the dissection of the frenulum is performed in children immediately after their birth in the maternity hospital, but there are cases when the need for surgery arises in children later at preschool age. Correction of the lingual frenulum can also be indicated for adults at some stages of orthodontic treatment, dental implantation, and in the cases of periodontal diseases [18-20].
When performing surgery on newborns, children of preschool and older age, and adult patients, the risks are not identical. Therefore, doctors should carefully monitor and evaluate the treatment process, and inform patients and their families about the advantages and disadvantages of various treatment techniques [21].
In the last few decades, laser surgery has become widely utilized in dentistry in the treatment of ankyloglossia in both adults and children [10, 22]. The laser beam is more effective than a scalpel or scissors, as it has many intraoperative and postoperative advantages, provided that all stages of laser surgery meet all the requirements to prevent the development of a recurrence of the disease. Photothermal interaction with biological tissues is the basis of the concept of laser application in surgery. During the operation of the laser, the radiation interacts with the tissue and is converted into thermal energy that changes the structure of the tissue. By choosing different modes of the laser, one can get the desired effect, from coagulation to incision [23, 24].
The wavelength plays an important role in all types of lasers used in the treatment process. The values of absorption and scattering, which determine the depth of radiation penetration, depend on it. The length is comparable to the absorption spectrum of tissue chromophores (specific acceptors of strictly defined wavelengths of light radiation). The part of chromophores can be played by water, hemoglobin, hydroxyapatite, pigment deposits, and proteins, which determine the depth of light penetration into biological tissues and the volume in which energy is released [25-27]. There are numerous manuscripts dedicated to the effective utilization of dental CO2, Er:YAG, Nd:YAG, and diode lasers for tongue frenectomy [1, 11, 28-30]. The advantages of laser surgery in comparison with conventional approaches include higher accuracy during the surgery, no intraoperative bleeding, a decrease in the surgery duration, and no need for suturing after manipulation in most cases. In the postoperative period, there is a complete absence of pain, or it is less intensive, and the same can be applied to the severity of edema and the formation of an inconspicuous scar. In addition, laser radiation has bactericidal properties, which ensures the absence of contamination during operation in contrast to scalpel surgery [25, 31-34].
The aim of our research was the analysis of scientific literature dedicated to the surgical methods of treatment of patients with ankyloglossia.
The literature review was carried out by searching through the PubMed database, Google Scholar; ResearchGate, and Elibrary for the following keywords and their combinations: ‘ankyloglossia’, ‘frenulotomy’, ‘frenectomy’, ‘laser’, ‘scalpel’, ‘surgery’.
The selected articles included studies and/or clinical cases of surgical methods of treatment of ankyloglossia using various lasers and a scalpel in patients within the period from 2011 to 2021. Most of the articles were published in the period from 2013 to 2021. Experimental studies were not taken into account. The total number of articles on this topic was 57, of which 13 articles included specific clinical cases and clinical trials, and 44 represented review articles and meta-analyses from earlier years, published between 2013 and 2020.
1.1. Scalpel
Conventionally, a frenectomy is performed under local anesthesia. The operating surgeon vertically retracts the lower lip, applies a hemostat to the middle of the frenulum, and makes two converging incisions on both sides of the clamp using a scalpel or scissors. Subsequently, the surgeon peels off the edges of the resulting wound along the entire perimeter by 1-3 mm, then brings them together, and puts the stitches (Figs. 2, 3). After the surgery, patients are prescribed antibiotics and painkillers.

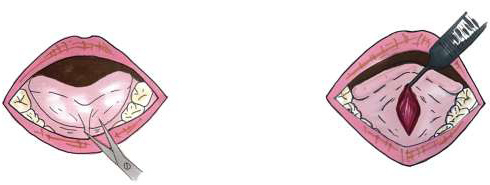
Reddy, N.R. and co-authors performed a conventional frenectomy under local anesthesia with 2% lidocaine hydrochloride solution using a scalpel with a blade Nº15. First, a clamp was applied to the frenum, after which two cuts were made on its upper and lower sides, thus removing the intermediate frenum. Then the muscle fibers were removed with forceps and the edges of the wound were sutured with 4.0 silk thread. In the postoperative period, the patient was prescribed analgesics and antibiotics. Swelling and pain appeared on the 1st postoperative and subsequent days, which subsided due to the administration of an anesthetic drug. The patient was recommended to perform tongue exercises after a week. Complete healing was noted a month after the surgery [35].
In the traditional technique, sutures are one of the causes of postoperative pain and discomfort in patients [12]. In addition to that, the severity of pain mostly depends on the depth of the incision [36]. Suturing the floor of the mouth can sometimes lead to blockage of the Wharton's duct, causing swelling of the corresponding area, and possible damage to the lingual nerve, accompanied by numbness of the tip of the tongue [18, 33, 37]. There may be postoperative complications such as bleeding, formation of a ranula or hematoma, and, therefore, prolonged postoperative healing and discomfort, although these complications occur infrequently if the surgeon is careful enough [19, 38]. Incomplete excision of the frenulum of the tongue, also separation often occurs insufficient rehabilitation, is one of the main reasons for the lack of clinical improvement, leading to fibrosis and recurrent ankyloglossia [39].
1.2. CO2 Laser
A CO2 laser represents a water- or air-cooled gas discharge containing a gas mixture with CO2 molecules that are involved in the creation of an infrared light beam. The energy of laser radiation with a wavelength of 10600 nm can be easily absorbed by water, so the depth of penetration into biological tissues largely depends on the presence of water in it. CO2 lasers have a small depth of penetration of laser energy into biological tissues (0.03 mm), which greatly reduces the risk of thermal damage to underlying tissues. The emission of CO2 laser energy is possible in either constant or pulsed modes. It provides a wide range of different types of effects on biological tissue, such as dissection, excision, resection, coagulation, and evaporation. Since CO2 lasers absorb water, they generate a lot of heat, which creates a carbonized layer that serves as a biological dressing [40, 41]. Laser surgery with this kind of lasers is an indication for the treatment of oral mucosal lesions, as it has a limited penetration depth of 0.2–0.3 mm. Postoperative pain is usually minimal or absent due to laser radiation reducing the release of pain mediators [42]. This type of laser also causes reduced myofibroblast invasion of the wound in contrast to one made with a scalpel, which results in minimal scarring and a near zero risk of bacteremia [28]. A CO2 laser can be used for several tongue surgeries, including the treatment of ankyloglossia.
Thus, Baxter R. and co-authors examined and treated children with limited tongue functions, and problems with speech, feeding and sleep. Thirty-seven patients aged from 13 months to 12 years underwent tongue frenectomy with a CO2 laser combined with myofunctional exercises. After the implementation of this treatment protocol, there was a functional improvement. Overall, according to parental reports, improvement in speech happened in 89% of the cases; 83% of children could intake solid food, and 83% got rid of their sleeping disorders [43].
The utilization of CO2 laser has several advantages, which include the decrease in postoperative pain, swelling, and intraoperative bleeding, provision of a dry surgical field, minimal scarring, and no need for sutures [38, 44, 45]. However, there are also some disadvantages described in the literature, such as a slight decrease in the regeneration rate due to thermal damage to the tissues surrounding the irradiation site, the high cost of equipment and the need for the surgeon to have certain skills to work with a laser.
During the procedure, the tip of the tongue should be fixed and restricted from any movement. The surgeon uses a CO2 laser with a wavelength of 10600 nm and output power of 1.6W in contactless mode with a distance of 1-2 mm above the tissue surface. Decontamination of the wound surface is achieved through high temperature generated by the laser, which reduces the risk of contamination of the surgical field and allows for avoiding antibiotic therapy. Cauterization of nerve endings leads to a decrease in postoperative pain, which helps to prevent the patient from using painkillers. Another important aspect of the laser, especially in children, is the reduction of the overall surgery time and the decrease in stress experienced by the child during the surgery. The latter can be considered as a significant criterion for managing patient behavior [46].
1.3. Diode Laser
A diode laser is one based on solid semiconductor crystals, consisting of a combination of aluminum (with a wavelength of 800 nm) or indium (900 nm), gallium and arsenic with a penetration depth of 1 mm. Since laser radiation of these wavelengths is poorly absorbed by hard tissues, this type of laser is intended for soft tissues. Moreover, laser radiation of these wavelengths can stimulate the proliferation of fibroblasts at low-energy levels [42]. Diode laser radiation is well absorbed by hemoglobin and melanin, but it is poorly absorbed by water; therefore, it has a significant ability to seal capillaries by denaturing the protein and stimulating the production of coagulation factor VII. For tongue frenectomy with a diode laser, the recommended parameters include a wavelength of 810-980 nm, a fiber diameter of 320-400 microns, power of 1.8-3.0W and energy of 272J; the surgery should be carried out in the continuous mode [28].
Laser frenectomy of the tongue is a simple and safe surgical operation, which is less traumatic than a scalpel surgery [47]. Due to the numerous advantages of laser technology, such as a bloodless surgical field, the absence of sutures, minimal swelling, and moderate postoperative pain, the utilization of a high-intensity diode laser is a reliable alternative for soft tissue surgery [2, 17, 48].
Junqueira, M.A. et al. conducted a study using a diode laser in a patient with this pathology. Speech therapists sent a seven-year-old boy to a pediatric dentistry clinic because of a speech disorder caused by a tongue tie. The dissection of the frenulum was performed under local infiltration anesthesia with a diode laser in a contactless mode, with a wavelength of 800 nm and a power of 2.0 W. The light guide was continuously moved from the central region of the frenulum toward the base of the tongue. Aspiration was not required, except for the products of evaporation obtained during the operation by the radiation of the diode laser. No sutures were applied, the postoperative period was uneventful [49].
In comparison with the conventional method of a frenectomy, the correction of the lingual frenulum with a diode laser results in the reduced duration of the operation [17, 50]; the complete absence of intraoperative bleeding [4, 51]; an apparent bactericidal effect, which is preferable in patients with a high risk of postoperative wound infection [41, 52]; better tissue regeneration [30, 47]; less apparent postoperative pain [53, 54]. In addition, according to some authors, the diode laser with a wavelength of 450 nm and 980 nm can produce highly efficient tissue vaporization with low thermal damage to adjacent tissues [51, 55].
1.4. Er:YAG Laser
Er:YAG laser can effectively cut or remove hard tissues of teeth, which is confirmed by the results of various studies. It can also be used in operations on soft tissues in cases where an apparent coagulation effect is not required [40, 41]. Er:YAG laser radiation is well absorbed by structures with a high content of water and collagen, including soft tissues. The Er:YAG laser is particularly selective for the fibrous tissue that forms the lingual frenulum. Er:YAG laser is considered optimal for pediatric oral surgery in the cases of small interventions, as it provides high efficiency with little blood loss. For the lingual frenum surgery, the recommended operating parameters of the Er:YAG laser are: a wavelength of 2940 nm with a penetration depth of 0,003 mm, power of 1-3 W, frequency of 20 Hz, and energy of 50-80 mJ. In the pulse mode, the frenulum incision is performed with a frequency of 10-30 pulses per second and a pulse duration of 300-600 microseconds [28].
Excision of the lingual frenulum using an Er:YAG laser radiation is quite effective, safe, and minimally invasive for the patient. The duration of the surgery can be significantly reduced, it is better tolerated than the conventional operation, and relapses are minimal. Regardless of the patient's age, in the case of a fibrous and thicker frenulum, the utilization of erbium lasers with wavelengths of 2780 nm and 2940 nm with a spray is the best option among other wavelengths due to minimal thermal exposure [26, 56, 57]. Er: YAG laser selectively and effectively affects fibrous tissues; there is no thermal damage when using the laser radiation with a spray, which minimizes the temperature increase in the tissue and, consequently, the formation of scar tissue and postoperative pain [56, 58].
Lamba, A.K. et al. performed frenectomy using an Er,Cr:YSGG laser with a wavelength of 2780 nm. Local anesthesia was used, after which the frenulum was dissected with Er,Cr:YSGG laser radiation in the pulsed mode, with a 600 μm sapphire tip with a power of 1.5 W. The intermediate part of the frenulum was removed, and a diamond-shaped wound was created. The muscle fibers were also released from the attachment to the inner surface of the lower jaw using the laser tip. The wound was dressed with 0.5 W laser radiation with air and water turned off. Analgesics and antibiotics were not prescribed. The postoperative period was uneventful, the wound healed without the formation of scar tissue, after which the patient was referred to speech therapy sessions. Three months after the surgery, a good reorganization of the scar was noted. The protrusion of the tongue behind the lower lip reached 16 mm, and the boy could speak normally. No recurrence was observed after 1 year [19].
Other authors have also noted the positive aspects of Er:YAG lasers. Thus, when using one for frenectomy, the intraoperative bleeding and heating of the tissues of neighboring areas are minimal. There is no carbonization, which allows for speeding up the healing process, with the formation of less amount of connective tissue, and a subsequent inconspicuous scar by reducing collagen remodeling [56, 59, 60].
With the development and introduction of Er:YAG lasers in medicine, dentists have received a safe and effective laser for the treatment of hard and soft tissues of the oral cavity. The small depth of penetration, high affinity for water, lack of thermal damage and minimal reflectivity, make this type of laser an ideal choice for dentistry. Also, an important advantage in the treatment of patients with Er: YAG laser is the bactericidal effect in the affected area, which ensures the sterility of the surgical field [19].
1.5. Nd:YAG Laser
Nd:YAG lasers have a solid active medium, which is a garnet crystal combined with rare earth elements yttrium and aluminum, doped with neodymium ions. This laser type provides good hemostasis and clear visualization of the surgical field during interventions on soft tissues [40-42]. It is characterized by a high level of absorption of radiation by hemoglobin, melanin and collagen, but it is poorly absorbed by water. It also demonstrates adequate penetration of radiation into the soft tissues of the oral cavity, providing coagulation, hemostatic and thermal effects with simultaneous decontamination and bactericidal action in surgical wounds, which ensures good clinical results. The 1064 nm neodymium laser with a penetration depth of 1,5 mm can operate at low and high output power, from 0.3 to 5.0 W, at 40 Hz, in pulsed or repetitive modes, transmitted by 320 µm optical fiber [28].
Surgery with an Nd:YAG laser has significant advantages over the conventional technique, one of which is minimal intraoperative bleeding or its absence. This, in its turn, also reduces the risk of postoperative bleeding to a minimum. Additionally, the laser beam ensures that the cut tissue is already decontaminated during the exposure itself. Thus, the risk of postoperative infection is reduced, pain and swelling are minimized, and the absence of sutures not only reduces the duration of the operation, but also prevents damage to neighboring healthy tissues.
In a study by Calisir M. and Ege B., patients preferred the Nd:YAG laser surgery in 77.5% of the cases and indicated the main reasons for this preference to such factors as less pain, no stitches, and no bleeding after the laser treatment. In the postoperative period, no complications associated with wound healing were observed. It has also been noted in the literature that after the conventional surgery, chewing and speech are more comfortable in contrast to the Nd:YAG laser surgery (Table 1). However, the results of the study suggest that Nd:YAG lasers are superior for oral soft tissue surgery in terms of increased patient comfort and pain reduction, especially in the early postoperative period [12].
| Authors | Year | Number of Patients | Age | Type of Surgery | Results and Conclusion |
|---|---|---|---|---|---|
| Randomized Clinical Trials | |||||
| Elvira Ferrés-Amat et al. [14] | 2016 | 101 | 4-14 yrs | Scalpel | 6% of patients had complications, 94% of patients with ankyloglossia had improvements |
| Komori, S. et al. [38] | 2017 | 21 | 6.0 yrs (Mean age) | CO2 laser(wavelength -10600, power - 2-5 W, penetration depth - 0,2-0,3 mm, continuous mode) | No complications, successful surgery in 100% of patients.Decontamination, coagulation |
| Zihoor El-Tayieb, A. et al. [41] | 2018 | 14 | 16-40 yrs | Scalpel,Diode laser(wavelength - 808 nm,power - 1,5-2 W, penetration depth - 1 mm, fiber diameter - 400 µm, frequency - 20.000 Hz, contact mode) | 50% of patients: decontamination,coagulation,no swelling, no pain, no sutures, no relapse |
| Zaghi, S. et al. [36] | 2019 | 348 | 29 mths - 79 yrs | Scissors | 45,1% of patients experienced pain, 12.6% had bleeding. 3,4% of patients encountered problems with salivary glands, 4.9% faced numbness of the tip of the tongue and 3.2% of patients reported deterioration in tongue mobility |
| Baxter, R. et al. [43] | 2020 | 37 | 4.2 yrs (Mean age; range from 13 mths to 12 yrs) | CO2 laser | Speech improved in 89% of patients, comfortable food intake and sleep restored in 83% of patients |
| Tripodi, D. et al. [9] | 2021 | 180 | 6-12 yrs (Mean age - 9.1 yrs) | Galbiati G25 diode laser (AlGaAs)(power - 4 W, fiber diameter - 320 µm, penetration depth - 1 mm) | Decontamination, coagulation, no swelling, no pain, no sutures, no relapse |
| Olivi, G. et al. [56] | 2021 | 30 | 8-18 yrs | Scalpel,Er:YAG laser(wavelength - 2940 nm, fiber diameter - 600 µm, energy - 120-160 mJ, frequency - 15 Hz, penetration depth - 0,003 mm) | Success rate was 96%, 4% of patients had complications |
| Shang J. et al. [59] | 2021 | 28 | - | Scalpel, Er:YAG laser (power - 3-4 W, penetration depth - 0,003 mm) | 54% of patients: decontamination,coagulation,no swelling, no pain, no sutures, no relapse |
| Other Types of Research(Clinical Case or Clinical Cases Series) | |||||
| Chiniforush, N. et al. [46] | 2013 | 1 | 12 yrs | CO2 laser(wavelength - 10600 nm, power - 1,5 W, frequency - 100 Hz, non-contact mode, penetration depth - 0,2-0,3 mm) | Decontamination, coagulation, no swelling, no pain, no sutures, no relapse |
| De Santis, D. et al. [60] | 2013 | 2 | 9, 10 yrs | Scalpel, Nd:YAG laser (wavelength - 1340 nm, power - 8 W, penetration depth - 1,5 mm) | Decontamination, coagulation, no swelling, no pain, no sutures, no relapse |
| Lamba, A.K. et al. [19] | 2015 | 1 | 22 yrs | Er,Cr:YSGG laser(wavelength - 2780 nm, power - 1,5 W, fiber diameter - 600 µm, penetration depth - 0,003 mm) | Decontamination, coagulation, no swelling, no pain, no sutures, no relapse |
| Bolla, V. et al. [33] | 2016 | 2 | 27, 24 yrs | Scalpel, Diode laser (wavelength - 810 nm, penetration depth - 1 mm, contact mode) | Decontamination, coagulation, no swelling, no pain, no sutures, no relapse |
| Samvedi, A. et al. [51] | 2018 | 2 | 20, 35 yrs | Diode laser(wavelength - 980 nm, power - 2 W, fiber diameter - 200 µm, penetration depth - 1 mm, contact mode) | Decontamination, coagulation, no swelling, no pain, no sutures, no relapse |
De Santis, D. et al. performed frenectomy in two patients aged 9 and 10 years. In the first patient, the frenectomy was performed by the conventional method, while for the second one, an Nd:YAG laser radiation was utilized. In the postoperative period, the discomfort and healing characteristics were assessed. The results showed that Nd:YAG lasers have the following advantages in contrast to the traditional excision of the lingual frenulum: complete hemostasis was noted during the surgery and the surgical field was clearly visible; there was no need for suturing; the operation was completed faster; there is no postoperative infection and no need for analgesics or antibiotics, minimal or no scar tissue; despite the initial slowness of the healing process, full and final recovery was faster overall.
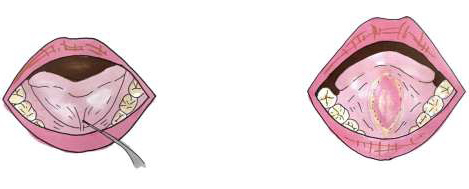
Given the above elements, it can be stated that laser lingual frenectomy has several undeniable advantages over conventional surgery [61]. A scheme of surgery involving a dental laser is provided in Fig. (4).
LIMITATIONS
In this study, we aimed to present the possibilities of laser surgery in the treatment and prevention of ankyloglossia at any age. Therefore, the limitation of the study is the analysis of all available articles dedicated to this topic, regardless of the type of the studies, number of patients, their age, gender, or place of residence.
CONCLUSION
There are many benefits to using a laser for a lingual frenectomy. Key advances reported in the literature include reduced inflammation and pain in the postoperative period, bloodless surgery that generates positive psychological feedback from the patients, reduced duration of surgery, and technical simplicity. The treatment of ankyloglossia in children should be carried out with a multidisciplinary medical approach, consisting of surgery, speech therapy and phoniatrics. When the lingual frenulum is released or excised with conventional instruments, an incomplete release may occur due to bleeding in this area, which not only makes the surgical field less visible but also complicates the surgery itself. Conventional surgery is performed using local anesthesia and sutures. The laser technique is an alternative to traditional surgery due to a simple and quick operation, requiring a minimum amount of anesthesia, with no need for suturing. Moreover, depending on the wavelength of the laser radiation used, a good hemostatic and disinfecting effect is provided, while access, visualization, and accuracy of the intervention are improved.
AUTHORS' CONTRIBUTIONS
Conceptualization, S.O. and E.M.; methodology, E.D.; software, Kh.M.; validation, E.A., A.D. and E.D.; formal analysis, S.O.; investigation, Kh.M.; resources, E.D.; data curation, E.A.; writing—original draft preparation, S.O.; writing—review and editing, E.A.; visualization, A.D.; supervision, A.D.; project administration, A.D. All authors have read and agreed to the published version of the manuscript.
LIST OF ABBREVIATIONS
| CO2 | = Carbon Dioxide |
| Er:YAG | = Erbium-Doped Yttrium-Aluminum-Garnet |
| Er,Cr:YSGG | = Erbium, Chromium-Doped Yttrium, Scandium, Gallium And Garnet |
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The schemes in this manuscript were created by the resident of the Department of Oral Surgery of E.V. Borovskiy Institute of Dentistry of Sechenov University, Do Phan Ngoc Minh.


