All published articles of this journal are available on ScienceDirect.
Quality of Life in Menopausal Women with Dental Restorations and Implants
Abstract
Aim:
This multicenter study examined the relationship, possible interactions, and intermittent effects that dental implants and prostheses can have on menopausal women’s quality of life as well as provided information regarding the possible side effects of therapeutic regimens on menopause and osteoporosis or osteopenia.
Materials and Methods:
Questionnaires consisted of selected quality of life questions based on specific and additional medical and dental (mainly prosthodontic) questions, which were administered to 100 Greek menopausal/post-menopausal women (Age: Mean Value=63,62 years old) with osteopenia or with or without osteoporosis, with dental implants and implant restorations, or conventional prosthetic restorations visiting two University Hospitals. Menopausal/post-menopausal status was judged on the basis of either secondary, definitive amenorrhoea or based on follicular stimulation hormone (FSH) values, estradiol, and clinical risk factors.
Results:
Participants had a statistically significantly better “functional” and “psychological” feeling after prosthodontic rehabilitation with and without implants. Three out of four reported that their dentist informed them of the possible implant problems that might arise from osteoporosis and its treatment (medications). Moreover, osteopenia was found to be associated with a very lower problem percentage. The bisphosphonate treatment had the highest rate (80%) of reported implant problems than non-bisphosphonate treatment (30%). The hormone replacement therapy (HRT) for menopause was reported to be more associated with problems in implant placement (19%) than in those without treatment (27.3%).
Conclusion:
The questionnaires revealed a significant improvement concerning women’s life quality and well-documented information about the problems their dental implants and restorations may cause in association with menopause and/or osteoporosis.
1. INTRODUCTION
Rehabilitation with dental prosthetic restorations and implants is an important and commonly accepted treatment in dentistry [1-4], especially to functionally and esthetically restore the oral cavity of partially or completely edentulous patients [5, 6], to replace missing teeth, and stabilize and support a denture with low retention [7, 8], as also to solve the same problems in non-compromised patients [9].
Nowadays, implant treatment needs less invasive surgery with less risk of complications, and in many diseases, it is viable, with or without specific precautions [9, 10]. Very few specific medical conditions can increase the risk of peri-operative problems or treatment failure [11]. Risk factors, such as the use of specific medications, have been presumed for successful implant treatment [12-14]. However, in patients under medical treatment, implants are worthwhile and benefit the health-related quality of life and improve oral functioning [15], but some medically compromised conditions need to be taken into consideration [9].
The menopausal period occurs at an average age of 51 years, and it marks the natural and permanent end of the woman’s reproductive cycle. During this time, various symptoms and medical problems occur in women, such as osteoporosis and osteopenia, which may hamper both women's dental treatment and, consequently, their quality of life [16-18].
Menopause is characterized by loss of endogenous estrogen (deficiency) and osteoporosis, identified by a bone mineral density (BMD) reduction in the jaw, bone tissue microarchitectural deterioration, and susceptibility to fractures [2, 6, 19-21]. Post-menopausal women could face a greater risk of tooth loss, and because of the bone healing process and the bone quantity’s reduction at implantation sites, the predictability of dental implants is volatile [2, 6, 22-24].
The dental treatment may be affected by the increasing uncertainty of age-related changes, like osteoporosis in the rising percentage of the population aged over 55. This rise occurs in about one-third of the western women aged over 65 years [2, 22, 23].
The World Health Organization (WHO) defines osteoporosis as a generalized skeletal disease resulting in the fragility of the bone tissue with a subsequent greater risk of fractures [24-26], and the dual-energy X-ray absorptiometry (DXA) is considered the “gold standard” for the diagnosis of osteoporosis or osteopenia as it measures the bone mineral density (BMD) [4, 27].
Considering that systemic osteoporosis has been a contraindication for treatment with dental implants, the initial view has gradually changed over the years because many reports showed that treatment is successful in osteoporotic subjects. Furthermore, no real difference was found concerning dental treatment results between non-osteoporotic and osteoporotic subjects [4, 28-30].
There is little data about dental implant placement techniques in the special group of menopausal women with and without osteoporosis. Their quality of life (QoL) has not been studied in detail [23]. The importance of oral-health-related QoL is mostly recognized by the World Health Organization (WHO). Related campaigns depicting esthetic images of bright smiles and images of pain-free living as a well-being profile are common [23, 31]. Recent investigations have focused on how oral health affects different aspects of life, such as self-esteem, psychosocial interaction, overall health, intimacy, and performance at work [23].
The risks associated with the medications used to treat post-menopausal osteoporosis and their effects complicate the decision-making during the planning phase of dental implant therapy and the final decision [23].
Bisphosphonates, as bone-sparing medications, have been related to a condition called osteonecrosis of the jaws (ONJ). Dental implant therapy is suggested to improve esthetics and self-image [32, 33]. As post-menopausal women age, they mostly undergo esthetic procedures in the lower third of their face [23, 34].
Τhe aim of this (multicenter) research was to examine the relationship and the possible interactions and intermittent effects that dental implants and dental prostheses can have on oral health and mainly on menopausal women’s quality of life, with or without osteoporosis or osteopenia in Greek women.
This study also investigated the extent of information provided by dentists on menopausal women undergoing the mentioned dental prostheses, as well as the information on the possible side effects of therapeutic regimens on menopause and osteoporosis.
The working hypothesis was that the use of dental prostheses and dental implants on this specific group of menopausal women improved their life quality in relation to the type of medication for osteoporosis (bisphosphonates and non-bisphosphonates), hormone replacement therapy, and problems on implants or on prosthetic restorations due to osteoporosis.
2. MATERIALS AND METHODS
This cohort study included a population of hundred menopausal women. The protocol was approved by the University Hospital of Ioannina, Greece. The patients came to the Obstetrics and Gynecology Clinic of the University Hospital of Ioannina and the Department of Climacteric and Menopause of the Second Obstetrics and Gynecology Clinic of the National and Kapodistrian University of Athens, Greece. Participants in this multicenter study were interviewed, and they provided their consent to participate in this study.
The method involved collecting demographic data; the study was conducted by a single examiner through personal communication. Questionnaires were administered in Greek to participating menopausal/post-menopausal women (Greek women) aged 43 years and over, with osteopenia or with or without osteoporosis, with or without dental implants and implant restorations, or conventional prosthetic restorations. Menopausal/post-menopausal status was judged on the basis of either secondary, definitive amenorrhoea or based on follicular stimulation, hormone values (FSH), estradiol, and clinical risk factors (e.g., history of osteoporotic fractures). The mean age of women who participated was 63-62 years (deviation 43 - 94 years).
Patients included were fully informed, orally and in writing, to complete a standard questionnaire on life quality, the Oral Health-Related Quality of Life (OHQoL), which was depicted by utilizing the short form of Oral Health Impact Profile Index (OHIP-14) [35-37]. It was modified with additional questions tailored to the needs of our study.
The questionnaire included selected quality of life questions in such a way as to escalate from introductory questions to more personal ones. Participants were given the necessary time and conditions to feel comfortable completing the questionnaire, including medical and dental (mainly prosthodontic) questions.
Data collection began with the development of a database that allowed the storage and processing of information regarding each patient and implant.
The main result variable in our questionnaire was the association between oral health and life quality, and it was measured by the Oral Health Outcome Profile -14 (OHIP-14). OHIP measures the attitude of individuals towards the social impact of oral disorders on their well-being. Our questionnaire consisted of seven dimensions containing two elements, in total 14 (OHIP 1-14). The seven dimensions of the questionnaire included limitations of pain, function, chewing, speech (pronunciation), self-esteem, functional state and psychological well-being, psychological distress, physical and mental disability, social disability, and handicap. Patient answers had to be recorded as one of five categories, i.e., never (0), almost never/hardly ever (1), occasionally (2), quite/fairly often (3), and very often (4). In our study, the questionnaire was adapted with the inclusion of additional questions [35-37].
The data were statistically analysed using computer software and t-test (IBM-SPSS v.25) and MS Excel 2019 and Statistica v.12.5 Enterprise were used for the diagrams/figures. The values were submitted to a one-way Variance Analysis (ANOVA) and a t-test equality check (independent groups/pairs). The X2 statistical check was applied to the nominal or operative variables. Finally, regarding the multiple correlations between variables, a Multiple Factorial Match Analysis was used with a significance level of P <0.05.
Bivariates and multivariate analyses were performed involving two or more variables, providing results concerning statistical tests on their possible correlation.
3. RESULTS
3.1. Demographic Results of our Sample
The patient sample consisted mainly of married women, i.e., 75%, 13% were unmarried, 9% were widows, and 3% were divorced. Regarding the educational level, the largest percentage (35%) was at the level of university education with a further 21% having postgraduate studies, while the smallest percentage (only 3%) represented the participants who were primary school graduates. Moreover, 15% declared a graduate of compulsory education (High School) while a fairly significant percentage (26%) declared a graduate of Lyceum.
Regarding the professional status of the participants during the survey, half (50%) were retired, while another 20% declared housekeeping as a professional occupation. Of the participants who declared themselves active professionally, 12% (out of the total) were civil servants, while 6% declared themselves private employees. Finally, 8% said that they were self-employed and 4% were unemployed. In an attempt to incorporate this information in a frequency table, we integrated all working participants in one category while leaving the other categories as they were.
3.2. Results Regarding Habits and Mmedications
In terms of personal habits that could affect the variables examined, emphasis was given to smoking. The majority of the sample (61%) were non-smokers; 11% said they smoked 6 to 10 cigarettes a day, while another 12% smoked 11 to 20 cigarettes daily. Nine percent seemed to smoke rather limited (1-5 cigarettes per day), while an even smaller percentage (7%) seemed to exceed one (typical) pack of cigarettes (> 20) daily.
From the analysis of the results, it was found that 31% received hormone replacement therapy (HRT), while 69% did not, while 74.2% received HRT in less than 5 years and 25.8% more than 5 years. Substitution therapy was given orally (per os) at 77.4% and 22.6% by the other routes. The above results were in line with the international literature. In the studied menopausal women, vasomotor disorders were found in 54%, psychosomatic disorders in 34%, and sexual and urinary disorders in 62%. These percentages were about the same as those mentioned in the international literature. Moreover, HRT intake and the above symptoms were not statistically related.
Of all participants, 44% received some treatment for osteoporosis. Of these, 77.3% of participants had been receiving osteoporosis medications for less than a decade and 22.7% for more than a decade. Moreover, almost three out of four (34/44) took medication with non-bisphosphonates, while about 7% took a combination of bisphosphonates/non-bisphosphonates, and the remaining 18% took bisphosphonates only.
3.3. Osteoporosis: Results of Diagnostic Test
Eighty-five percent of participants underwent osteoporosis testing. More specifically, 68% of participants performed a DEXA (Dual Energy X-ray Absorptiometry) test for bone mass in the OMSS (Lumbar Spine), and 64% had a DEXA test in the hip (Femoral Head).
The two bone mass tests were cross-checked to see if it was more common for participants to undergo both tests. Τwenty-six participants did not perform either test. Moreover, 85.3% of the participants who had undergone DEXA OMSS had also done DEXA hip. It turned out that the two tests were usually done together.
From the diagnosis of osteoporosis test, 4.7% of the participants did not show clinical features related to the presence of osteoporosis. 32.9% were diagnosed with osteoporosis, while 62.4% were with osteopenia.
3.4. Dental Implants
Next, the sample’s dental clinical status focused on the placement of dental implants and other prosthetic restorations was presented, as described/mentioned by the participants themselves.
Fifty-seven percent of the participants had dental implants, and out of this sample, in 28.1% of the participants, implants were placed in both jaws. Implants only in the maxilla were placed in 28,1%, while 43.9% of the participants had implants only in the mandible.
Of these dental implants, in terms of the maxilla, 25% were placed anteriorly and 28.1% posteriorly in the mouth, while 46.9% were in both the posterior and anterior parts. Regarding the mandible, 14.6% of the implants were placed anteriorly and 63.4% posteriorly in the mouth. Moreover, 22% of the implants were placed in both the front and back of the mouth. 49.1% of the implants that have been placed were used to support fixed restorations, while 26.3% of the implants were used to support overdentures.
3.5. Prosthetic Restorations
Seventy-six percent of all participants had prosthetic restorations without dental implants. 36.8% of the participants had restorations on the maxilla, 23.7% on the mandible, and, finally, 39.5% on both the maxilla and mandible. Overall, 76% of participants underwent prosthetic restorations apart from dental implant placement. On average, these restorations were carried out 13.97 years ago with SD ± 8.19 years. Regarding the placement of restorations in the maxilla, 35,5% were single crowns, 44,7% were fixed partial prosthesis, and 7,9% were removable partial dentures. In the mandible, 26,3% were single crowns, 36,8% were fixed partial prosthesis, 13,2% were removable partial dentures, and 6% were complete dentures.
3.6. Quality of Life (before and after dental intervention)
3.6.1. Perceived Difference before and after Restoration
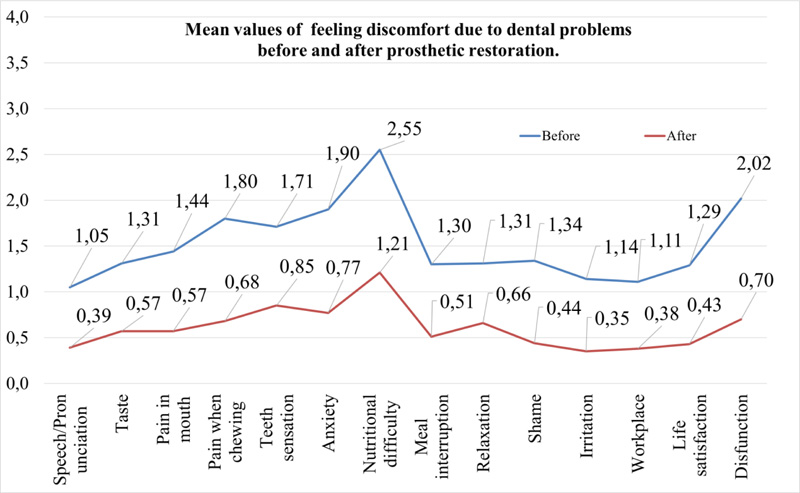
This was followed by answering the questions concerning perceived discomfort from dental problems before and after prosthetic restoration. Fig. (1) depicts the results of all studied parameters, such as:
1) The “nutritional difficulty” (mean 2.55) had the highest average both before and after prosthetic restoration (average mean 1.21 after).
As can be seen in Fig. (1), the orange line is firmly below the blue line. The orange line depicts the means of the perceived discomfort “after” the prosthetic restoration, while the blue line is the means “before.”
2), We can also observe in Table 1 that all answers were correlated with “before” and “after” with positive and statistically significant correlation indices.
3), Regarding the psychological discomfort (anxiety), the participants were asked to further clarify what they meant. Most participants (29%) meant functional reasons, while a smaller percentage (10%) probably referred to esthetic reasons.
4), Regarding psychological discomfort (shame), esthetic reasons prevailed in both “before” and “after” (before 31% and after 16%). However, in the previous significant percentage (14%), they also had both categories of reasons (esthetic and functional), but in the aftermath, this percentage decreased significantly (in 4%).
Overall, it can be concluded that the participants showed a much better condition after the prosthetic restoration than before. The differences in means referring to a marked reduction in dental discomfort after prosthetic restoration were found to be statistically significant (Table 2).
| N | Correlation | Sig. | ||
|---|---|---|---|---|
| Pair 1 | Pain in mouth before and pain in mouth after | 100 | ,480 | ,000 |
| Pair 2 | Pain when chewing before and pain when chewing after | 100 | ,407 | ,000 |
| Pair 3 | Teeth sensation before and teeth sensation after | 100 | ,492 | ,000 |
| Pair 4 | Anxiety before and anxiety after | 100 | ,348 | ,000 |
| Pair 5 | Nutritional difficulty before and nutritional difficulty after | 100 | ,487 | ,000 |
| Pair 6 | Meal interruption before and meal interruption after | 100 | ,563 | ,000 |
| Pair 7 | Relaxation before and relaxation after | 100 | ,566 | ,000 |
| Pair 8 | Shame before and shame after | 100 | ,525 | ,000 |
| Pair 9 | Irritation before and irritation after | 100 | ,370 | ,000 |
| Pair 10 | Workplace before and workplace after | 100 | ,504 | ,000 |
| Pair 11 | Life satisfaction before and life satisfaction after | 100 | ,327 | ,001 |
| Pair 12 | Disfunction before and disfunction after | 100 | ,386 | ,000 |
| Pair 13 | Pronunciation/Speech before and pronunciation/speech after |
100 | ,478 | ,000 |
| Pair 14 | Taste before and taste after | 100 | ,464 | ,000 |
| Paired Differences | t | df | Sig. (2-tailed) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | Std. Deviation | Std. Error Mean | 95% Confidence Interval of the Difference | ||||||
| Lower | Upper | ||||||||
| Pair 1 | Pain in mouth before - Pain in mouth after |
,87000 | 1,20315 | ,12032 | ,63127 | 1,10873 | 7,231 | 99 | ,000 |
| Pair 2 | Pain when chewing before - Pain when chewing after |
1,12000 | 1,37275 | ,13728 | ,84762 | 1,39238 | 8,159 | 99 | ,000 |
| Pair 3 | Teeth sensation before - Teeth sensation after | ,86000 | 1,30283 | ,13028 | ,60149 | 1,11851 | 6,601 | 99 | ,000 |
| Pair 4 | Anxiety before - Anxiety after | 1,13000 | 1,45404 | ,14540 | ,84149 | 1,41851 | 7,771 | 99 | ,000 |
| Pair 5 | Nutritional difficulty before - Nutritional difficulty after | 1,34000 | 1,39422 | ,13942 | 1,06336 | 1,61664 | 9,611 | 99 | ,000 |
| Pair 6 | Meal interruption before - Meal interruption after | ,79000 | 1,18317 | ,11832 | ,55523 | 1,02477 | 6,677 | 99 | ,000 |
| Pair 7 | Relaxation before - Relaxation after | ,65000 | 1,16667 | ,11667 | ,41851 | ,88149 | 5,571 | 99 | ,000 |
| Pair 8 | Shame before - Shame after | ,90000 | 1,32192 | ,13219 | ,63770 | 1,16230 | 6,808 | 99 | ,000 |
| Pair 9 | Irritation before - Irritation after | ,79000 | 1,20013 | ,12001 | ,55187 | 1,02813 | 6,583 | 99 | ,000 |
| Pair 10 | Workplace before - Workplace after | ,73000 | 1,17082 | ,11708 | ,49768 | ,96232 | 6,235 | 99 | ,000 |
| Pair 11 | Life satisfaction before - Life satisfaction after | ,86000 | 1,41436 | ,14144 | ,57936 | 1,14064 | 6,081 | 99 | ,000 |
| Pair 12 | Disfunction before - Disfunction after | 1,32000 | 1,54971 | ,15497 | 1,01250 | 1,62750 | 8,518 | 99 | ,000 |
| Pair 13 | Pronunciation/Speech before - Pronunciation/Speech after | ,66000 | 1,20789 | ,12079 | ,42033 | ,89967 | 5,464 | 99 | ,000 |
| Pair 14 | Taste before - Taste after | ,74000 | 1,20286 | ,12029 | ,50133 | ,97867 | 6,152 | 99 | ,000 |
3.6.2. Dental Practice Issues
Finally, the answer was searched in a series of questions regarding dental practice concerning the treatment of patients with osteoporosis/osteopenia. Ninety-five percent of the participants stated that their dental practitioner recommended dental implant placement and informed them about possible implant problems that might occur due to medication for osteoporosis.
When they were asked if there were problems with the dental implants due to osteoporosis, 84% of the participants answered that there was no such situation.
Finally, 43% of the participants stated that, in financial terms, the cost/benefit ratio was positive, while an additional 44% described it as “reasonable.” However, 13% of the participants reported a rather negative cost/benefit ratio.
3.7. The Intersection between “Type of Medication for Osteoporosis” and “there have been Implant Problems Due to Osteoporosis”
We proceeded with the correlation between possible problems that (according to the participants) arose during the placement of dental implants and the type of medication for the treatment of osteoporosis.
As shown in Table 3, bisphosphonate medication had the highest rate of reporting implant placement problems (4 out of 5 participants or 80%). With a much smaller quota (30%), participants receiving non-bisphosphonate medication reported problems during implant placement. In a similar percentage (33%), participants who received a combination of medication with non-bisphosphonates and bisphosphonates also reported problems with implant placement. Finally, the fewest problems (only 13.5%) were reported by participants who did not receive any treatment for osteoporosis.
From Table 4, it can be seen that this correlation gave statistically significant results (X2=11.158, BE=3, p=0.011<0.02). Therefore, according to the participants, bisphosphonates actually seemed to cause more problems with implant placement than other types of medication.
3.8. Cross-check between “Osteoporosis Diagnosis” and “Osteoporosis Implant Problems”
Apart from the type of medication, the actual diagnosis of osteoporosis could be an indicator of the “severity” of osteoporosis, and so, when cross-checked with the statement of implant problems, we would have some possible evidence of the disease itself and the implant problems compared to “the association of implant problems and medication.”
As shown in Table 5, the highest reported rate of implant problems (39.1%) was found in participants diagnosed with osteoporosis. The corresponding percentage of participants diagnosed with osteopenia was only 21.4%.
| There have been implant problems due to osteoporosis | Total | ||||
|---|---|---|---|---|---|
| Yes | No | ||||
| Medication for Osteoporosis | No therapy | Count | 5 | 32 | 37 |
| % Medication for osteoporosis | 13,5% | 86,5% | 100,0% | ||
| % There have been implant problems due to osteoporosis | 31,3% | 65,3% | 56,9% | ||
| Bisphosphonates | Count | 4 | 1 | 5 | |
| % Medication for Osteoporosis | 80,0% | 20,0% | 100,0% | ||
| % There have been implant problems due to osteoporosis | 25,0% | 2,0% | 7,7% | ||
| Non-bisphosphonates | Count | 6 | 14 | 20 | |
| % Medication for osteoporosis | 30,0% | 70,0% | 100,0% | ||
| % There have been implant problems due to osteoporosis | 37,5% | 28,6% | 30,8% | ||
| Bisphosphonates + Non-bisphosphonates | Count | 1 | 2 | 3 | |
| % Medication for osteoporosis | 33,3% | 66,7% | 100,0% | ||
| % There have been implant problems due to osteoporosis | 6,3% | 4,1% | 4,6% | ||
| Total | Count | 16 | 49 | 65 | |
| % Medication for osteoporosis | 24,6% | 75,4% | 100,0% | ||
| % There have been implant problems due to osteoporosis | 100,0% | 100,0% | 100,0% | ||
| Value | df |
Asymptotic Significance (2-sided) |
|
|---|---|---|---|
| Pearson Chi-Square | 11,158a | 3 | ,011 |
| Likelihood Ratio | 9,985 | 3 | ,019 |
| Linear-by-Linear Association | 2,575 | 1 | ,109 |
| N of Valid Cases | 65 |
| There have been implant problems due to osteoporosis | Total | ||||
|---|---|---|---|---|---|
| Yes | No | ||||
| Osteoporosis Test Diagnosis | Nothing | Count | 0 | 4 | 4 |
| % Osteoporosis Test diagnosis | 0,0% | 100,0% | 100,0% | ||
| % There have been implant problems due to osteoporosis | 0,0% | 10,0% | 7,3% | ||
| Osteoporosis | Count | 9 | 14 | 23 | |
| % Osteoporosis Test diagnosis | 39,1% | 60,9% | 100,0% | ||
| % There have been implant problems due to osteoporosis | 60,0% | 35,0% | 41,8% | ||
| Osteopenia | Count | 6 | 22 | 28 | |
| % Osteoporosis Test diagnosis | 21,4% | 78,6% | 100,0% | ||
| % There have been implant problems due to osteoporosis | 40,0% | 55,0% | 50,9% | ||
| Total | Count | 15 | 40 | 55 | |
| % Osteoporosis Test diagnosis | 27,3% | 72,7% | 100,0% | ||
| % There have been implant problems due to osteoporosis | 100,0% | 100,0% | 100,0% | ||
| Receiving Hormone Replacement Therapy | Total | ||||
|---|---|---|---|---|---|
| Yes | No | ||||
| Type of Osteoporosis Medication | No therapy | Count | 13 | 43 | 56 |
| % Type of Osteoporosis Medication | 23,2% | 76,8% | 100,0% | ||
| % Receiving Hormone Replacement Therapy | 41,9% | 62,3% | 56,0% | ||
| Bisphosphonates | Count | 4 | 3 | 7 | |
| % Type of Osteoporosis Medication | 57,1% | 42,9% | 100,0% | ||
| % Receiving Hormone Replacement Therapy | 12,9% | 4,3% | 7,0% | ||
| Non-bisphosphonates | Count | 11 | 23 | 34 | |
| % Type of Osteoporosis Medication | 32,4% | 67,6% | 100,0% | ||
| % Receiving Hormone Replacement Therapy | 35,5% | 33,3% | 34,0% | ||
| Bisphosphonates + Non-bisphosphonates |
Count | 3 | 0 | 3 | |
| % Type of Osteoporosis Medication | 100,0% | 0,0% | 100,0% | ||
| % Receiving Hormone Replacement Therapy | 9,7% | 0,0% | 3,0% | ||
| Total | Count | 31 | 69 | 100 | |
| % Type of Osteoporosis Medication | 31,0% | 69,0% | 100,0% | ||
| % Receiving Hormone Replacement Therapy | 100,0% | 100,0% | 100,0% | ||
3.9. Cross-check between “Receiving Hormone Replacement Therapy” and “Type of Osteoporosis Medication”
Having already recognized the correlation between the type of medication for osteoporosis and the reported implant placement problems, it would be interesting to examine if there was a correlation between the type of medication and the estradiol level since the participants in our sample were all in menopause state. Therefore, the focus was whether hormone replacement therapy is related to osteoporosis medication?
As shown in Table 6, taking hormone replacement therapy appeared to be associated with not taking osteoporosis medication; 41.9% of participants taking hormone replacement therapy did not receive any treatment for osteoporosis. 35.5% of participants taking hormone replacement therapy also stated that they were taking non-bisphosphonates. Finally, bisphosphonates and combinations of bisphosphonates and non-bisphosphonates were taken by participants receiving hormone replacement therapy at significantly lower rates, i.e., 12.9% and 9.7%, respectively.
In Table 7, it can be seen that this correlation gave statistically significant results (X2=10.530, BE = 3, p = 0.015 <0.02). Thus, according to the statements of the participants, the participants who did not take hormone replacement drugs, in a percentage of 62.3%, did not follow any treatment related to osteoporosis. In contrast, participants taking hormone replacement therapy followed a significantly higher proportion of osteoporosis medications, i.e., 35.5% non-bisphosphonates and the rest in smaller doses.
| Value | df |
Asymptotic Significance (2-sided) |
|
|---|---|---|---|
| Pearson Chi-Square | 10,530a | 3 | ,015 |
| Likelihood Ratio | 10,766 | 3 | ,013 |
| Linear-by-Linear Association | 3,737 | 1 | ,053 |
| N of Valid Cases | 100 |
| There have been implant problems due to osteoporosis | Total | ||||
|---|---|---|---|---|---|
| Yes | No | ||||
| Receiving Hormone Replacement Therapy | Yes | Count | 4 | 17 | 21 |
| % Within Receiving Hormone Replacement Therapy | 19,0% | 81,0% | 100,0% | ||
| % Within There Have Been Implant Problems Due To Osteoporosis | 25,0% | 34,7% | 32,3% | ||
| No | Count | 12 | 32 | 44 | |
| % Within Receiving Hormone Replacement Therapy | 27,3% | 72,7% | 100,0% | ||
| % Within There Have Been Implant Problems Due To Osteoporosis | 75,0% | 65,3% | 67,7% | ||
| Total | Count | 16 | 49 | 65 | |
| % Within Receiving Hormone Replacement Therapy | 24,6% | 75,4% | 100,0% | ||
| % Within There Have Been Implant Problems Due To Osteoporosis | 100,0% | 100,0% | 100,0% | ||
3.10. Cross-check between “Taking Hormone Replacement Therapy” and “there have been Implant Problems Due to Osteoporosis”
Clearly, it was interesting to see if the variable “Taking Hormone Replacement Therapy” correlated statistically significantly with the variable “There have been implant problems due to osteoporosis.”
In Table 8, it can be seen that the participants who followed hormone replacement medication reported that there were problems in the placement of implants in 19%, while those who did not follow reported problems in 27.3%. Therefore, we could assume that taking hormone replacement therapy tended to “limit” the statement of the problems that arose in the placement of implants. However, this correlation did not give statistically significant results (X2=0.518, BE=1, p=0.551>> 0.05).
3.11. Cross-checks between “Smoking” and “There have been Implant Problems Due to Osteoporosis”
The harmful habit of smoking could affect the process of implant placement. Therefore, we made the correlation between “Smoking” and “There were implant problems due to osteoporosis.”
However, the results shown in Table 9 reported that regardless of the smoking category, approximately the same percentage of participants indicated problems with the implant placement. More specifically, with no smoking at all, 26.2% of the participants reported problems, while in the category of “heavier” smoking (more than one pack), the same percentage was 25%. Finally, in the “up-to-a pack” smoking category, 21.1% of participants reported implant problems.
However, this correlation did not yield statistically significant results (X2=0.186, BE=2, p=0.91>>0.05).
4. DISCUSSION
The present study was performed on a sample of patients consisting of a specific homogeneous population of menopausal women with or without osteoporosis or osteopenia and with conventional or implant prosthetic restorations and examined their quality of life before and after dental treatment assessed by means of questionnaires.
Specific demographic characteristics, such as educational level, occupation, and habits (smoking), were investigated. Furthermore, the categorization of the women studied was based on diagnostic laboratory criteria for the characterization of menopause, osteoporosis, or osteopenia, as well as the different medications or no medication given for the case. The above parameters, either individually or in combination, were investigated in relation to the quality of life before and after the prosthetic restorations, conventional and with implants, in this specific sample of the population. Another originality was that the questionnaires used for the study were new, upgraded, and with additional questions version of the OHIP-14 methodology.
According to the above mentioned, the questionnaire of the present study was prepared to investigate parameters related to the changes, as expressed by the participants, before and after the dental prosthetic treatment and concerned with their quality of life (QoL). The QoL measurement can provide health care providers with valuable information regarding the deficiencies and needs in patients’ lives and the effects of interventions [38].
| There have been implant problems due to osteoporosis | Total | ||||
|---|---|---|---|---|---|
| Yes | No | ||||
| Smoking categories | No smoking | Count | 11 | 31 | 42 |
| % Smoking categories | 26,2% | 73,8% | 100,0% | ||
| % There have been implant problems due to osteoporosis | 68,8% | 63,3% | 64,6% | ||
| Up to a pack (20) | Count | 4 | 15 | 19 | |
| % Smoking categories | 21,1% | 78,9% | 100,0% | ||
| % There have been implant problems due to osteoporosis | 25,0% | 30,6% | 29,2% | ||
| More than one pack | Count | 1 | 3 | 4 | |
| % Smoking categories | 25,0% | 75,0% | 100,0% | ||
| % There have been implant problems due to osteoporosis | 6,3% | 6,1% | 6,2% | ||
| Total | Count | 16 | 49 | 65 | |
| % Smoking categories | 24,6% | 75,4% | 100,0% | ||
| % There have been implant problems due to osteoporosis | 100,0% | 100,0% | 100,0% | ||
The quality of life associated with oral health (OHQoL) is defined as “the absence of negative effects of oral conditions on social life and the positive sense of self-confirmed teething” [38, 39]. In our study using OHIP-14, the mono-parametric and multi-parametric total assessment of the results was made. Few studies have emphasized patient experiences concerning their oral health’s quality of life and dental implants [35, 36, 39, 40]. Our study included for the first time a specific population and investigated the responses of Greek women. OHIP has evolved and is one of the most widely used OHQoL indices internationally and has proven validity for different populations, especially for populations with prosthetic restorations [39].
The selection and implementation of the OHIP-14 questionnaire for our population, among other information, recorded the satisfaction and self-esteem of the women who participated in the study, which was in accordance with the findings reported in international literature. In accordance with the above mentioned, in our questionnaire, questions were included that assessed the effect of chewing hard foods, functional ability, and well-being before and after dental treatment in our specific population of women with or without osteoporosis or osteopenia and with or without medical treatment for these conditions.
In conclusion, the questionnaire applied in our study included not only the parameters related to OHIP-14 but also additional questions, such as occupational status, education, and habits (e.g., smoking), thereby exploring the multi-parametric combination of these. Such a questionnaire has never been multi-factorially investigated in other studies where either individual parameters or a number of fewer factors have been studied in combination.
In the present study, our results found statistically significant differences in quality of life for a large number of specific parameters before and after dental treatment, while other studies either deal with the quality of life of patients having single restorations [35] or reported follow-up results of patients who received at least one single implant [41].
In our study, the responses of our patients confirmed the positive change in the parameters included by OHQoL in relation to their both social life and self-confirmation as well as their good oral function, which is in agreement with other studies [36].
The correlation between age and preference for dental treatment was another parameter of our study. Age was found to be not associated with the preference for specific prosthetic rehabilitation like other studies [42, 43].
In Busenlechner’s study [43], a history of periodontal disease and smoking increased the risk of implant failure by 2 times and 3 times, respectively, and the survival rate in subjects suffering from osteoporosis did not significantly differ from the healthy subjects. In our study, surprisingly, smoking was not associated with being a possible contraindication for implant placement.
The methodology of the present study could be considered an important characteristic in the study of PROMs (Patient Reported Outcome Measures) and in results that expressed qualitative characteristics of changes in quality of life before and after dental prosthetic restorations. The quality of life of the participants measured and evaluated before and after treatment was found to be continuously improved, which was also in line with the findings of a study conducted by Reisine et al. [35].
It should also be highlighted that this is the first study on the quality of life based on the OHIP-14 questionnaire, which focused exclusively on post-menopausal women. This present research compared the quality of life in partially edentulous osteoporotic women, in which missing teeth have been restored with implant restorations, conventional fixed prostheses, and removable partial dentures before and after the restoration of missing teeth. Despite the nonsignificant difference in ages among the groups, there was a significant difference in all QoL areas, including health, occupational, emotional, and overall QoL scores between osteoporotic women with missing teeth replaced with implant restorations, conventional fixed, and removable restorations before and after treatment. These findings were in agreement with that of the study conducted by DeBaz [23].
In our population, a significant improvement was reported in chewing in general and in chewing hard foods after prosthetic restoration, which was consistent with the findings of DeBaz's study [23] and Fueki K. et al. [44].
Another issue was that OHIP-14 in our study revealed satisfied patients with dental implants with their life quality aligned with good health (OHQoL), agreeing with the study of Alzarea [36]. Despite excellent treatment with conventional dentures, this might not result in an improvement in a person's quality of life. Significant differences in subjective reactions to comfort, function, speech, aesthetics, and dental health are demonstrated when comparing implant overdentures in an unhappy patient with conventional complete dentures [32]. In relation to the above, the present study showed that menopausal women were pleased with the outcome of dental treatment either by implant placement and implant rehabilitation or by conventional prosthetic restorations and reported an improvement in speech and appearance.
Many investigations have been made concerning the relationship between skeletal bone density and bone density of the jaw [45] as also the implant osseointegration in osteoporotic female patients appears to indicate lower osseointegration in osteoporotic conditions. The same conclusion was drawn from the present investigation.
Another essential parameter is not only the patients’ information about their medication due to osteoporosis or other menopausal-post menopausal conditions but also the obligation of dental practitioners to inform them about the relationship between osteoporosis treatment and dental treatment. Therefore, if a doctor prescribes or intends to prescribe an anti-absorbent agent, the patient and the patient's dentist should be informed. It is necessary for clinicians and dentists to investigate and ask questions during the medical history of issues related to osteoporosis, osteopenia, and the use of various anti-absorbent agents [46]. Our study found satisfactory patient information from dental practitioners.
The onset of the jaw’s bisphosphonate osteonecrosis (BP-ONJ) had a huge impact on patients' quality of life, as patients reported a high negative feeling of pain, swallowing problems, and social behavior. Therefore, the prevention of BP-ONJ should be one of the primary objectives, which is also reported in a study conducted by Walter et al. [47].
Oral BP intake was related to a significantly higher risk of developing jaw osteonecrosis [48]. Considering this, our study found satisfactory patient information from dental practitioners.
In our study, 80% of women treated with bisphosphonates reported problems with implants, especially those women whose treatment lasted more than 4 years. Long-term prospective studies are still needed to determine the effectiveness of discontinuation of medication to reduce MRONJ risk for these subjects.
For patients who have received oral BPs for more than 4 years, we should contact the prescribing therapist to consider discontinuing anti-absorbent therapy for 2 months before oral surgery if general health conditions allow it. BPs should not start until healing is complete. The risks of long-term oral BP treatment require continuous monitoring [49].
Our study provided an assessment of patients' subjective responses to dental implants and prosthetic rehabilitation treatment in combination with the information they had from the gynecologist and dentist who, as demonstrated by their responses, correctly informed the menopausal osteoporotic women of our sample.
The DEXA method is currently recognized as the gold standard for measuring skeletal BMD and detecting osteoporosis. For the women included in the present study’s sample, DEXA was indeed the standard for measuring bone density and characterizing osteoporosis.
In our study, 85% of the women underwent the osteoporosis DEXA test. The above percentages showed a satisfactory control rate for osteoporosis, something very important for the following dental treatment.
By the term "problems" the patient perceived and expressed a number of difficulties/problems/complications that might have arisen without being able to separate biological problems, which might be associated with osteoporosis treatment, as opposed to technical problems (e.g., screw loosening, etc.), which were not clearly related to taking medication. To solve this question, extensive clinical and para-clinical examination and extensive interviews with the patient to separate biological and technical problems would be required. This could not be done under the existing conditions of the investigation. These limitations should also be taken into account in subsequent analyses and cross-checks of “implant osteoporosis problems.”
CONCLUSION
The questionnaires revealed a significant improvement concerning women’s life quality and well-documented information about the problems their dental implants and restorations may cause in association with menopause and/or osteoporosis.
Participants had a statistically significantly better “functional” and “psychological” feeling after prosthetic rehabilitation with and without implants and a statistically significant reduction in dental discomfort after prosthetic rehabilitation. The “psychological distress” expressed as “shame” was significantly reduced due to prosthetic, conventional, and implant restorations. The majority of participants characterized the cost/benefit ratio for implant restorations as “positive” or “reasonable.” The attending dentist recommended implant placement and informed the patients with osteoporosis-osteopenia of the possible implant problems that might arise from osteoporosis and its treatment with either bisphosphonates or a combination of bisphosphonates and non-bisphosphonates. Bisphosphonate treatment appeared to be associated with significantly more problems with implant placement. Osteoporosis and less osteopenia cause implant problems, while hormone replacement therapy eliminates them.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study received ethical approval No. 19/28-05-2015 (i.25) issued by the University Hospital of Ioannina, Greece.
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Participants in this multicenter study were interviewed and given their consent to participate in this study.
STANDARDS OF REPORTING
STROBE guidelines and methodologies were followed in this study..
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author, [S.S.], on special request.
FUNDING
None.
CONFLICT OF INTEREST
The authors confirm that this article's content has no conflict of interest.
ACKNOWLEDGEMENTS
All authors acknowledge the contribution of participants to this manuscript.


