All published articles of this journal are available on ScienceDirect.
A Lipoma of Large Proportion in the Oral Cavity: A Case Report
Abstract
Background
Lipoma is a benign neoplasm that can affect the whole body and rarely occurs in the oral cavity. It is slow-growing and asymptomatic, and conservative surgical treatment with total removal of the lesion is the treatment of choice. It originates from epithelial cells of mature adipose tissue.
Case Presentation
The aim of this study was to report a clinical case of a large lipoma in a 21-year-old male patient with melanoderma who presented a nodule in the region of the buccal vestibule extending from the region of the second molar to the ipsilateral canine, with an approximate size of 40 mm in its largest diameter in the anteroposterior direction and approximately 20 mm in diameter in the buccolingual direction. The initial diagnostic hypothesis was based on an ultrasound of the face, which detected a solid, circumscribed, echogenic nodule compatible with a lipoma of the face. Surgical treatment with excisional biopsy was chosen. The histopathological examination revealed fragments with the presence of discrete acanthosis and clear hyperkeratosis in the epithelium, along with the proliferation of mature adipocytes constituting a neoplastic parenchyma surrounded by a stroma.
Conclusion
The findings have confirmed the diagnosis of oral lipoma. The patient has evolved with a good prognosis and remained under follow-up without recurrence or sequelae. The present report has corroborated what has been observed in similar cases described in the literature regarding recurrence and excellent prognosis.
1. INTRODUCTION
Lipoma is a benign tumor of mesenchymal origin, with mature adipose cells found inside and normally covered by a fibrous connective tissue capsule [1]. The etiology of oral lipoma is unclear, and some studies have suggested that mechanical factors, endocrine system, inflammatory processes, obesity, chromosomal abnormalities, radiation, trauma, mucosal infections, and chronic irritations may contribute to the development of the tumor [2, 3].
Lipomas represent approximately less than 5% of all benign tumors of the mouth, with the oral mucosa, a region that is normally rich in adipose tissue, followed by the tongue, lips, floor of the mouth, palate, and gums being the most affected sites [3-5]. They generally occur in the fourth and fifth decade of life with a higher incidence at 40 years of age and a predilection for the male sex [6]; however, some authors have reported no predilection for sex [4].
The lesions appear as asymptomatic, well-defined, slow-growing masses, with a consistency that varies from soft to firm on palpation, and they may be floating, yellowish nodules [4, 5]. They may present a variant form with the potential to infiltrate skeletal muscle tissue or even a bone variant [2]. The color of oral lipomas can vary from yellow to pink, depending on the depth of the lesion [6]. Most lesions are approximately 10 mm in diameter. However, in some cases, lesions can reach larger diameters, compromising speech and chewing and compressing important anatomical structures [3].
Although rare, lipomas can affect the maxilla and mandible, corresponding to approximately 3% of all intraosseous lipomas in the body [7]. Mandibular symphysis, body, and ramus are the most common sites for mandibular injuries [2]. Total surgical excision of the lesion without the need for a safety margin is the treatment of choice for resolving the lesion, with recurrence being rare [8-10].
2. CASE REPORT
A 21-year-old male patient with melanoderma and without associated systemic diseases was referred to the Stomatology service of the DSC (Dental Specialties Center) of Praia Grande City Hall complaining of a “bump on the cheek”, without painful symptoms, lasting approximately one year. At the time of the consultation, he reported feeling a certain discomfort due to the bump on the cheek, damaging the “aesthetics”. During the anamnesis, he reported having boxed years ago.

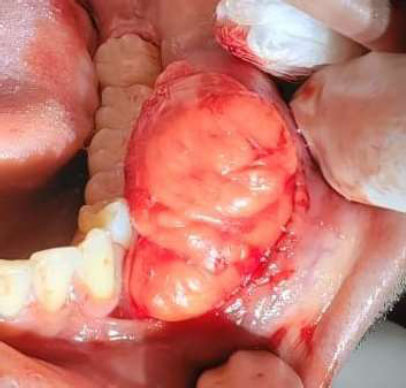
Intraoral clinical appearance of the lesion (initial photo).
Fonte: De Branco (2020).
On extraoral examination, an increase in volume was found in the region of the buccal mucosa and the body of the mandible on the left. In the intraoral clinical examination, an extensive, sessile, pinkish-colored, submucosal, smooth surface endophytic nodule was observed in the region of the buccal vestibule extending from the region of the second molar to the ipsilateral canine, with an approximate size of 40 mm in its largest diameter in the anteroposterior direction and approximately 20 mm in diameter in the buccolingual direction (Fig. 1).
The patient already had a definitive diagnosis of the lesion, obtained by incisional biopsy and histopathological examination that had been carried out in another stomatology service, where the diagnosis of lipoma was confirmed. The following complementary exams were requested for surgical planning: panoramic X-ray to rule out possible intraosseous variation of the lipoma, ultrasound of the region to aid surgical approach, and laboratory tests, including complete blood count, coagulogram, prothrombin time, partially activated thromboplastin time, and fasting blood glucose. The radiographic examination revealed the absence of bone involvement, ruling out the possibility of a bone variation of the lipoma (Fig. 2). The ultrasound examination revealed normal skin and subcutaneous tissue, with a preserved muscle layer, normal-looking lymph nodes in the region, and intact blood vessels. In the left region of the face, close to the depressor anguli oris muscle, a circumscribed solid nodule was found, with lobulated margins in the subcutaneous plane measuring 3.7x2.4x4.3 cm. The other complementary laboratory tests were within normal limits. Upon confirmation of the test results, surgical planning was carried out for total excision of the lesion through excisional biopsy.

Radiographic image showing the absence of bone lesion.
After the patient signed an informed consent form, he underwent a complete surgical excision of the mass under local anesthesia in an outpatient setting. Intraoral and extraoral asepsis was carried out beforehand. The anesthesia of choice was local infiltration in the region of the buccal vestibule of the mandible and in the region of the molars to promote anesthesia of the buccal nerve and deposition of anesthetic in the region of the mentonian foramen in order to anesthetize the mental nerve. Terminal infiltration was performed in the periphery of the lesion 3-4 mm away to avoid the formation of volume that would make it difficult to confirm the periphery of the lesion and compromise histopathology. Next, an elliptical incision was made in the mucosa on the surface of the lesion with a #15 blade mounted on a scalpel (Fig. 3).

Elliptical incision over the lesion.
Disinsertion of the lesion in the periphery after divulsion.
Intraoperative and macroscopic examination of the lesion revealed an encapsulated nodular lesion measuring approximately 3.5x2x4 with a soft, greasy consistency and a yellowish color. Divulsion was performed with a blunt-tipped instrument, separating normal tissue from the periphery of the lesion, a maneuver that proved to be easily performed due to the extensive fibrous capsule that surrounded the lesion, which is a very common feature in classic lipomas (Fig. 4). During the completion of the total exposure of the lesion, the appearance of the buccal branch of the facial nerve in close contact with the lesion showed the importance of prior topographic anatomical knowledge (Figs. 5 and 6).
After total enucleation of the lesion along its entire periphery with the aim of separating the surgical bed, excision was performed with an Allis-type grasping instrument (Fig. 7). The surgical field was washed abundantly with 0.9% saline solution and the surgical wound was carefully inspected to check for any resulting fragments and verify the integrity of the nervous branch of the facial nerve.

Buccal branch of the facial nerve (blue arrow; diagonal view).
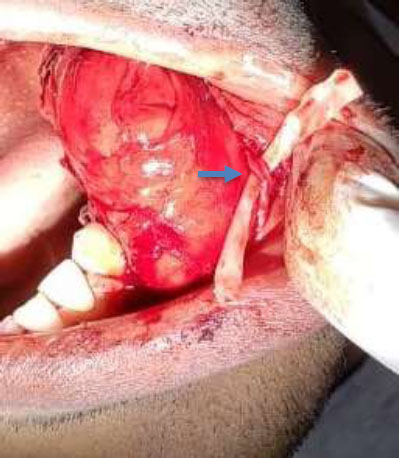
Buccal branch of the facial nerve (blue arrow).
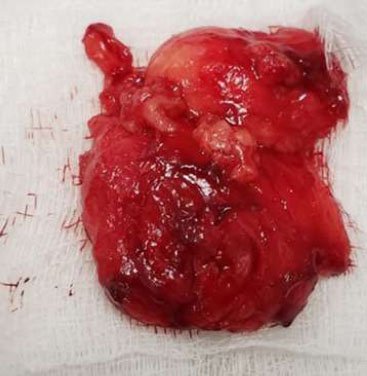
Photograph of the lesion after its removal.
Soon after, the suture was placed with continuous scalloped stitches using 4.0 mononylon (Fig. 8). Upon completion of the procedure, the patient was instructed on post-operative care and prescribed analgesic (dipyrone 1 g in 6 hours) and steroidal anti-inflammatory agent (dexamethasone 4mg in 8 hours). The patient's postoperative period took place 7 days after the procedure when the sutures were removed (Fig. 9). The removed material was stored in a bottle containing 10% formaldehyde and sent to the oral pathology service at the University of São Paulo (USP-SP). The histopathological examination revealed fragments with discrete acanthosis and clear hyperkeratosis in the epithelium, along with the presence of proliferation of mature adipocytes constituting a neoplastic parenchyma surrounded by a stroma, thus confirming the diagnosis of oral lipoma. The patient was re-evaluated 45 days after the operation, where he showed excellent healing, no sensory or motor nerve deficit, and was followed up for 2 years without recurrence and with an excellent recovery (Fig. 10).
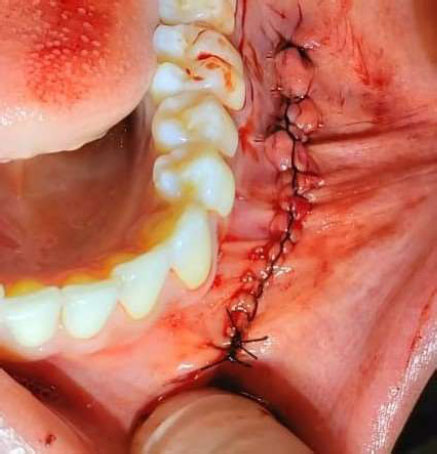
Photograph of the area after suture.

Photograph of the area 7 days post-operation.

Photograph of the area 45 days post-operation.
3. DISCUSSION
Although lipomas are common in other regions of the body, they occur with little incidence within the oral cavity [2, 3]. Their etiology is quite uncertain and variable [10], with the most varied causes reported to be trauma, hormonal changes, inflammatory processes, and obesity [3, 5]. The diagnosis is normally based on the clinical characteristics through a careful anamnesis and the previous history of the injury. In the case of larger and infiltrating lesions, it is necessary to use imaging tests, such as ultrasound, computed tomography, and magnetic resonance imaging, to assist in diagnosis and mainly in surgical planning [9]. Depending on their intraoral location, they can present with dysphagia, hoarseness, dyspnea, a foreign body sensation, and a painless cervical mass [10]. Massive sublingual lipomas can cause a range of functional problems, such as dysphagia, impaired speech, and mastication [11, 12]. They rarely result in compressive symptoms. Clinically, differential diagnoses include mucoceles, pleomorphic adenoma, and fibromas [10]. The differential diagnosis can also include granular cell tumors, neurofibroma, traumatic fibroma, and salivary gland diseases (mucocele and mixed tumor) [12].
The diagnosis should be based on the characteristic histopathological findings of the benign tumor. Histopathological examination of the lesion often provides a definitive diagnosis. Histopathological findings demonstrate arrangements of mature adipocytes divided by lobules of connective tissue, surrounded by a thin fibrous capsule [4, 7]. Several histological variants are also described, such as angiolipoma, spiny cell lipoma, pleomorphic lipoma, spindle cell lipoma, intramuscular lipoma, and myxoid lipoma [1, 9, 11]. However, the most common type is fibrolipoma, which is the classic form of the lesion [2, 10, 11].
Adequate surgical excision without the need for a safety margin is the treatment of choice for this tumor, which has a rare recurrence, with the exception of the infiltrating type of lipoma, which shows a more recurrent recurrence rate.
CONCLUSION
The present report has corroborated what has been observed in similar cases described in the literature regarding recurrence and excellent prognosis of lipomas.
AUTHORS’ CONTRIBUTION
V.B.G.: Study conception and design; Y.K.: Methodology; C.R.T: Investigation; S.B., M.G., W.S.: Drafting of the manuscript.
ABBREVIATION
| DSC | = Dental Specialties Center |
CONSENT FOR PUBLICATION
A written informed consent was obtained from the patient before proceeding with the publication of this case report.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.


