Surface Roughness of Er, Cr: YSGG Laser Etched Enamel Compared to Phosphoric Acid Etched Ename: An In Vitro Study
Abstract
Objectives:
Erbium-based lasers have been used in dentistry with different parameters for enamel conditioning with controversial results on the optimum parameter. This study aims to compare the surface roughness of enamel after conditioning by erbium, chromium-doped: Yttrium scandium-gallium-garnet (Er, Cr: YSGG) laser or 37% phosphoric acid and after remineralization, using a scanning electron microscope (SEM).
Materials and Methods:
Forty-five extracted premolars for orthodontic purposes were divided into three groups according to the conditioning technique. Group 1 conditioning by Er, Cr: YSGG laser 4.5 watts/30 Hz, Group 2 conditioning by Er, Cr: YSGG laser 4.5 watts/ 20 Hz, and Group 3 conditioning by 37% phosphoric acid. Surface roughness was measured using SEM after conditioning and after remineralization using Recaldent GC MI Paste Plus. Statistical analysis was done by one-way analysis of variance ANOVA test used to compare between groups, followed by Tukey’s post hoc test.
Results:
Enamel surface conditioned by Er, Cr: YSGG 4.5 watts/20 Hz laser had significantly less surface roughness than 37% phosphoric acid conditioned. After remineralization both the laser groups produced significantly lower surface roughness compared to acid conditioning.
Conclusion:
Er, Cr: YSGG laser conditioning of enamel surfaces (with 4.5 watts and 20 Hz/ 30 Hz frequency) produced less surface roughness which could be used as a promising alternative for acid conditioning.
Clinical Relevance:
laser conditioning of enamel using Er, Cr: YSGG with 4.5 watts could be a promising alternative for acid conditioning since it produces less surface roughness, less plaque accumulation on the surface, and less bacterial adhesion.
1. INTRODUCTION
With the advancements of technology in the dental world, different types of lasers have been introduced to various fields of dentistry, including the restorative field with the potential application for enamel surface etching and its effect on surface roughness and adhesion [1]. Surface roughness denotes irregularities or small indentations and projections that influence the surface characteristics such as its wetting capabilities, quality of adhesion, and brightness. A roughened surface provides a larger surface area for the adhesive infiltration, which provides a stronger bond [2, 3].
More recently, questions have been postulated regarding lasers' efficacy in carrying out enamel surface treatment before bonding. The main question is whether laser etching (with different types and parameters) provides a rougher enamel surface than acid etching. Do changes in the laser frequency contribute to any significant difference in the surface treatment [4].
For dental procedures involving hard tissue, Erbium lasers have the upper hand when it comes to the choice of lasers. The main two types with regards to safety and efficiency are Er: YAG (yttrium aluminium garnet 2940 nm) and Er,Cr:YSGG (yttrium scandium gallium garnet 2790 nm), for they exhibit optimum absorption of infrared lasers in hydroxyapatite and water, which are the main components of enamel and dentin. Er:YAG and Er,Cr:YSGG have very similar designs and properties [5].
The process of remineralization involves the provision of calcium and phosphate ions from an external source to the tooth. This helps fill gaps in demineralized enamel and ultimately leads to a net gain of minerals [6]. Recently, new methods of delivering calcium-phosphate-based remine-ralization have been developed for use in clinical settings. One such method is Recaldent™, which combines casein phosphopeptides and amorphous calcium phosphate (CPP-ACP). This system has been touted as a way to prevent and even reverse white spot lesions. Casein phosphopeptides (CPP) are produced from milk protein casein and are believed to enhance the levels of calcium phosphate in dental plaque, thereby reducing demineralization and promoting remineralization [7].
In the literature, Er, Cr: YSGG laser has been used with different power settings, frequency, and time of exposure for enamel etching with controversial results regarding surface roughness and bond strength compared to acid etching of enamel [4, 8-11]. While, one study [11] used Er, Cr: YSGG with an energy output of 4.5 watts/50 Hz but, assessed the shear bond strength, not surface roughness. Thus, the objective of this in vitro study is to quantify and compare the surface roughness of enamel after etching by Er, Cr: YSGG laser (with different frequencies) or 37% phosphoric acid and after a remineralization protocol, using a scanning electron microscope (SEM). The null hypothesis stated in this study is that there are no differences in the mean surface roughness values after etching with Er, Cr: YSGG laser with different frequency parameters, and acid etching.
2. MATERIALS AND METHODS
Forty-five maxillary first and second premolars were extracted for orthodontic purposes, collected, and stored in a thymol solution with 0.1% concentration. Caries-free teeth with no cracks and intact buccal enamel surfaces (with no prior surface treatment) were selected. This study was approved by the ethics committee, Faculty of Dentistry – Cairo University, approval number: 28223.
One clinician placed the selected teeth vertically in a self-cure acrylic resin cylinder (Rapid Repair, Detrey Dentsply Ltd, Surrey, U.K.). A standardized area of 4 mm width and 4 mm height in the middle third of the buccal surface was selected for surface treatment. The surface treatment done was as follow (with each group having 15 teeth):
- Group (1): Er, Cr: YSGG laser with an energy output of 4.5 watts and 30 Hz frequency.
- Group (2): Er, Cr: YSGG laser with an energy output of 4.5 watts and 20 Hz frequency.
- Group (3): 37% phosphoric acid (3M Unitek, Monrovia, USA) for 30 s and rinsed for 60s with distilled water and gently air dried.
In groups 1 & 2, Er, Cr: YSGG laser (2.78 μm wavelength) was used for 15 s at a 45-degree angulation with a working distance of 5 mm on a 4 mm x 4 mm square on the buccal surface. The same remineralizing protocol was used for all groups: A single layer of Recaldent GC MI Paste Plus (GC Corp., Tokyo, Japan) approximately 0.5 mm in thickness was applied for 3 minutes. It was applied twice a day followed by synthetic saliva rinsing, which was composed of NaCl (0.400g/l), KCl (0.400 g/l), CaCl2 · H2O (0.906g/l), NaH2PO4 · 2H2O (0.690 g/l), Na2S · 9H2O (0.005 g/l) and urea (1 g/l) with a pH of 7.1. The tooth was kept in synthetic saliva between the remineralizing paste applications, followed by fresh synthetic saliva rinsing daily for 15 days [12]. Rcaledent GC MI Paste Plus is a casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) based paste with 900ppm Fluoride [7]. The artificial saliva was prepared at the Laboratory of Biochemistry, Faculty of Pharmacy, Cairo University, Egypt. The artificial saliva was prepared by dissolving the following composition in water: 1.5 mmol/L CaCl2, 0.9 mmol/L KH2PO4, 130 mmol/L KCl, 1.0 mmol/L NaN3, and 20 mmol/L4-(2-hydroxyethyl)-1-piperazine ethane sulfonic acid. The pH 7.0 was adjusted with KOH (1 mmol/L). The prepared artificial saliva has a close similarity to human saliva which can act as a source of Ca and P ions in the remineralization cycle.
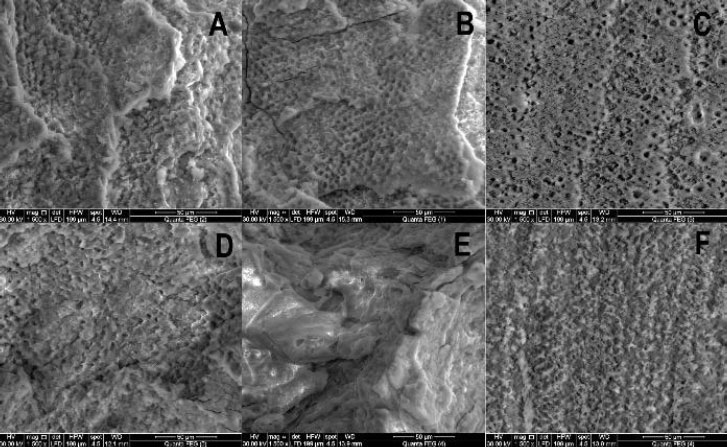
SEM images were taken after both etching and remineralization. The SEM Model Quanta 250 FEG (Field Emission Gun, FEI Company, Philips Electron Optics, Eindhoven, Netherlands) was used for this purpose attached to the energy dispersive x-ray unit (EDX) with an accelerating voltage of 30 KV and magnification of X250 and X1500. Measurements to quantify surface roughness were taken after etching and remineralization.
2.1. Statistical Analysis
The surface roughness values were presented as mean and standard deviation (SD) values measured in millimetres (mm). Data were explored for normality using the Kolmogorov-Smirnov test. The Kolmogorov-Smirnov test was insignificant which indicated that the data were normally distributed. One-way analysis of variance ANOVA test was used to compare mean values of surface roughness between different groups, followed by Tukey’s post hoc test in case of significant results.
The percentage of change was calculated by the following formula:
Paired t-test was used to compare mean values before and after mineralization within the same group. The significance level was set at 5%. Statistical analysis was performed with SPSS 16.0 (Statistical Package for Scientific Studies, SPSS, Inc., Chicago, IL, USA) for Windows.
3. RESULTS
3.1. Comparison between Different Groups
SEM images for different groups after etching and after remineralization are shown in Fig. (1). After etching, the highest mean value was recorded in group 3 (acid etched). This value was significantly greater (p=0.003) than that recorded in group 2 (20 Hz) which recorded the least mean value. Tukey’s post hoc test revealed no significant difference between groups 1 and 2, neither between groups 2 nor 3 (Table 1).
After remineralization, the highest mean value was recorded in group 3 (acid etched). This value was significantly greater (p=0.004) than that recorded in group 1 (30 Hz) and group 2 (20 Hz). Tukey’s post hoc test revealed no significant difference between groups 1 and 2 (Table 1).
Tukey’s post hoc test: Within the same comparison, means sharing the same superscript letter is not significantly different.
Paired t-test: within the same group showed a significant difference between before and after.
3.2. Comparison within the Same Group
Paired t-test revealed a significant difference between the mean before and after remineralization values (p<0.00001, p=0.24, P<0.00001) in groups 1 (30Hz), 2 (20 Hz), and 3 (acid) respectively (Table 1). The greatest mean percent change (increase) in surface roughness was recorded in group 1 (30 Hz), followed by group 3 (acid), while the least mean percent change (increase) was recorded in group 2 (20 Hz). ANOVA test revealed the difference between groups regarding the percent change (increase) in surface roughness was not significantly different.
| - | - | Mean | Std. Deviation | Std. Error | 95% Confidence Interval for Mean | F | P | |
|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||||
| Before | Group (1)30Hz | 21.58 a,b | 4.37 | 1.38 | 18.46 | 24.70 | 7.22 | .003* |
| Group (2)20Hz | 17.83 b | 3.71 | 1.18 | 15.17 | 20.48 | |||
| Group (3) acid | 26.72a | 7.06 | 2.23 | 21.67 | 31.77 | |||
| After | Group (1)30Hz | 12.65 b | 1.54 | .49 | 11.55 | 13.76 | 6.93 | .004* |
| Group (2)20Hz | 13.48 b | 2.52 | .79 | 11.68 | 15.28 | |||
| Group (3) acid | 16.67 a | 3.28 | 1.04 | 14.32 | 19.02 |
4. DISCUSSION
For a long time, the standard of etching enamel surfaces was done using 37% phosphoric acid which resulted in micro-porosities that enhanced the adhesive bonding via resin tags (micro-mechanical retention means). However, this etching technique resulted in more decalcification leaving the enamel susceptible to caries and discolouration after bonding [4, 13]. This is why laser etching techniques were developed to overcome these problems using different laser types [4]. Laser-etched enamel surfaces exhibit a porous surface close to that produced by acid etching which means it could be used as an alternative to acid etching [14]. Erbium lasers irradiated on enamel surfaces for different uses, cause the water content to heat up to the point of becoming steam which causes micro-explosions on the surface resulting in tissue ablation [5]. Er, Cr: YSGG laser has a higher absorption coefficient in water owing to its wavelength that coincides with water content in enamel, thus it is the most favourable erbium laser used for the ablation of hard tissues [5]. Er, Cr: YSGG power setting for enamel cutting ranges from 2.5 to 6 watts [1, 4, 15].
Previous studies [4, 8-11] used different parameters for Er, Cr: YSGG laser (power, frequency, and time of application) with different results regarding surface roughness compared to acid etching with one study only using 4.5 watts/ 50 Hz but assessed shear bond strength. Thus, the objective of this study was to quantify and compare the surface roughness after etching with laser or acid etching and the added effect of remineralization on both techniques.
The power setting of Er, Cr: YSSG laser used in this study was 4.5 watts with different frequencies of 20 Hz or 30 Hz and applied for 15 seconds compared to acid etching by 37% phosphoric acid for 30 seconds. In this current study, acid-etched enamel surfaces showed significantly more rough surfaces than laser-etched ones. Thus, the null hypothesis is rejected in favour of the alternative hypothesis which indicates a difference in mean surface roughness values after etching with a laser. This result agrees with a study by Faizee et al. 2022 [9] in which Er, Cr: YSGG laser was used with a power of 2 watts and different frequencies of 15 Hz and 25 Hz and the authors concluded that laser etching is more favourable than acid etching owing to decreased surface roughness which could make Er, Cr: YSGG laser etching an alternative to acid etching.
In another study by Hossain et al. 2001 [16], laser etched surfaces by Er, Cr: YSGG (3 watts power, 20 Hz frequency and applied for 6 seconds) produced significantly rougher surfaces than acid etching, which is against the current study results. However, this could be due to differences in the laser parameters and the way of measurement (color laser 3D microscope). A study by Dilip et al. 2018 [17], found that Er, Cr: YSGG laser etching exhibited non-significant higher surface roughness values compared to acid etching when using laser output power of 1.5 watts and 20 seconds of application and both had significantly higher surface roughness values compared with laser output powers of 1.5 watts/10 seconds, 1 watts with 10 or 20 seconds. These results agree with our study but the author used different power outputs, time of application, and measurement device (3D optical profiler).
A scoping systematic review done by Labunet et al. 2022 [4] for etching enamel surfaces with different types of laser including Er, Cr: YSGG concluded that several studies showed similar results between both Er, Cr: YSGG etching and acid etching and that Er, Cr: YSGG laser eliminates smear layer without cracking and produce rough surfaces, which could be a promising alternative for acid etching. In this study, the lower roughness values of the laser-etched surfaces compared to the acid-etched surfaces could be due to the ablation that the laser does on the enamel surface, analogous to the melting of a solid [18]. Furthermore, the higher mean surface roughness of the acid-etched enamel could be due to the concentration and duration of acid etching. Longer etching time results in a rougher surface topography as shown in a previous study [2].
Remineralization is based on the concept of replacing lost minerals from the tooth with minerals present in the natural saliva or, as in the case of this study, artificial saliva [19]. The patterns of mineral deposition influence the surface roughness of enamel [7, 19]. After remineralization with Rcaledent GC MI Paste Plus, the surface roughness measures decreased in all groups of this study compared to before. More specifically, the highest mean surface roughness recorded was in the group of teeth that were acid-etched before remineralization.
A study conducted by Al-Ani et al. 2020 [20] found that surface roughness decreased after the application of CPP-ACP-based paste, which agrees with the results of our study. Another study conducted by Poggio et al. 2014 [21] found that surface roughness increased after remineralization with CPP-ACP-based paste, which contradicts the study findings. However, the dissimilarity in such results could be due to the difference in methodology, where both studies followed a full demineralization protocol with pH cycling while in the present study, surface treatment for only a few seconds was done. In both studies mentioned above, the surface roughness after the remineralization was still higher than that measured at the baseline [20, 21]. demineralization and remineralization to different extents could result in different roughness values.
A systematic review and meta-analysis of in vitro studies investigating surface roughness of enamel after remineralization with CPP-ACP found a statistically significant reduction in surface roughness after CPP-ACP application when measured by atomic force microscopy [22] which agrees with our findings regardless of the different method of measurement. The studies included in this systematic review [23-25] were combined in a meta-analysis showing a standardized mean difference of -8.21 [95% CI -10.37, -6.04]. The author concluded that CPP-ACP-based paste has a desirable repair effect on enamel surfaces making them smoother and more aesthetically appealing.
The surfaces roughness measurements after remine-ralization are important and do not only affect aesthetics but also reveal bacterial adhesion and plaque formation on teeth surfaces [26, 27]. The limitations of our study include not being able to test different power outputs or different application times, that could show which chosen parameter is better. One of the limitations of this study is that it is an in vitro study which cannot be always correlated to clinical findings, so we need more clinical trials to assess the clinical performance of laser etching versus acid etching in clinical settings.
CONCLUSION
Taking into consideration the limitations of the current study, Er, Cr: YSGG laser etching of enamel surfaces (with 4.5 watts and 20 Hz/ 30 Hz frequency) produced less surface roughness which could be used as a promising alternative for acid etching. Laser etching showed smoother surfaces after remineralization which is important to prevent bacterial adhesion and plaque formation.
AUTHORS' CONTRIBUTION
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by Rashaa Raafat and Dina Mohamed. The first draft of the manuscript was written by Rashaa Raafat and Dina Mohamed commented on previous versions of the manuscript. All authors read and approved the final manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the ethics committee, Faculty of Dentistry – Cairo University, approval number: 28223.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.


