All published articles of this journal are available on ScienceDirect.
Latest Evidence on Orthognathic Surgery Techniques and Potential Changes in Oral Microbiota related to Intermaxillary Fixation in Orthodontic Patients: A Systematic Review
Abstract
Background:
Orthognathic surgery is often applied for the correction of facial dysmorphia, and different findings were highlighted regarding the techniques applied. After surgical treatment, intermaxillary fixation is placed, which compromises oral hygiene and, consequently, can lead to increased plaque accumulation and microbiological changes, promoting the proliferation of periodontopathogenic bacteria. Therefore, the aims of the present review are to describe the main evidence from the last 20 years of clinical studies concerning surgical techniques applied to orthognathic surgery and, finally, to analyze potential changes in the oral microbiota.
Materials and Methods:
An electronic search was conducted in the PubMed (MEDLINE) and Scopus databases; the MeSH (Medical Subject Heading) terms are bacteria, dental plaque, evidence-based practice, maxillomandibular fixation, microbiota, operative procedures, and orthognathic surgery.
Results:
At the end of the search process, 31 relevant articles were finally included and analyzed in this systematic review, which has a low risk of bias. Clinical studies on humans have been considered in this review. Based on the studies included it would be preferable to use piezoelectric technology in osteotomies because of its many advantages, “surgery-first” technique allows for results comparable to the standard technique in Class III malocclusions while improving quality of life more rapidly, the “mandible-first” technique seems to have more advantages than the “maxilla-first” technique, Computer-Aided Design and Manufacturing (CAD/CAM) could provide more accurate and precise results, and finally, Laser can be applied with different advantages. Regarding intermaxillary fixation, no long-term increase in the concentration of periodontal bacteria was recorded.
Conclusion:
Several findings still need to be confirmed with reference to the best suturing technique to reconstitute the nasal wing base, the real effectiveness of “surgery-first,” “maxilla-first,” and “mandible-first” approaches in patients with Class III malocclusion, the use of CAD/CAM and Laser, more studies should be conducted to evaluate quantitative and qualitative changes in other microorganisms following intermaxillary fixation.
1. INTRODUCTION
Disharmonious growth of the jaw bones is called a “dentoskeletal deformity,” which results in patients' functional, aesthetic, and psychological impairment [1].
Correction of this malocclusion is managed through orthognathic surgery by improving masticatory function [2], preventing periodontal disease [3], worsening tempo- romandibular disorders [4], and, finally, improving phonetics and appearance [5].
However, rare surgical and periodontal complications may be associated with oral and maxillofacial surgery, which could be partially or totally corrected by the introduction of several regenerative materials [6-8].
After orthognathic surgical treatment, the initial process of postoperative wound healing occurs. Patients may present with pain, swelling, and reduced mouth opening due to an interocclusal splint, which can immobilize the dental arches to allow undisturbed bone healing of osteotomy sites [9, 10].
There are some systematic reviews in the literature regarding the results of orthognathic surgery techniques concerning long-term airway evolution [11], root resorption [12], and bone grafting [13]. To date, there are no systematic reviews having addressed microbiota change in orthodontic patients undergoing intermaxillary block.
In the last two decades, with the evolution of digital technology, several clinical studies on humans have been performed to evaluate the impact of certain techniques on final aesthetics and patient psychology and compare the utilization of piezoelectric and computer-assisted surgery with traditional surgery. In addition, intermaxillary fixation associated with orthognathic surgery leads to obvious impairment of oral hygiene and, as a result, could lead to increased plaque accumulation and microbiological changes, promoting the proliferation of periodontopathogenic bacteria and, conse- quently, the periodontal pockets formation [14].
Therefore, the aims of this review were to describe the main evidence from the last 20 years of clinical studies on humans regarding surgical techniques applied in orthognathic surgery, and, finally, to analyze potential changes in the oral microbiota in orthodontic patients undergoing orthognathic surgery with intermaxillary fixation.
2. MATERIALS AND METHODS
2.1. Focused Questions
What is the main evidence from the last 20 years regarding surgical interventions in a patient population undergoing orthognathic surgery? Regarding changes in the oral microbiota, does comparison with patients who have not undergone orthognathic surgery result in changes in the outcome?
2.2. Eligibility Criteria
The following inclusion criteria guided the analysis of the studies: (I) study design—clinical trials, randomized clinical trials, case-control studies, cross-sectional studies, cohort studies, (II) participants—orthodontic patients undergoing orthognathic surgery with subsequent application of the intermaxillary fixation, (III) interventions—assessment of the main evidence from the last 20 years of clinical studies on humans regarding surgical techniques applied in orthognathic surgery, and finally, qualitative assessment of the oral microbiota in patients undergoing orthognathic surgery with intermaxillary fixation, (IV) outcome— evidence of clinical studies on humans regarding surgical techniques applied in orthognathic surgery, and changes in the oral microbiota in orthodontic patients undergoing orthognathic surgery with intermaxillary fixation. Only studies that met all inclusion criteria were included. However, the following exclusion criteria were included: (I) abstract of articles published in non-English languages, (II) duplicate studies, (III) not pertinent studies, (IV) in vitro or in vivo studies on animals, (V) absence of Ethics Committee approval, and (VI) case report, case series, narrative reviews, scoping reviews, systematic reviews, or systematic and meta-analysis reviews.
2.3. Search Strategy
The PICO model [15] (Population, Intervention, Comparison, Outcome) was used to perform this review, through a literature search of the PubMed (MEDLINE) and Scopus electronic databases, which is based on the following three elements: population (people with skeletal malocclusions undergoing orthognathic surgery), concept (evidence from clinical studies on humans related to orthognathic surgery techniques and possible changes in the oral microbiota following intermaxillary fixation), and context (in this case, the review has not been limited to any specific cultural factor or setting). Abstracts of studies that evaluated the main evidence from the last 20 years of clinical studies on humans regarding surgical techniques applied in orthognathic surgery, and changes in the oral microbiota in patients undergoing orthognathic surgery with intermaxillary fixation were reviewed.
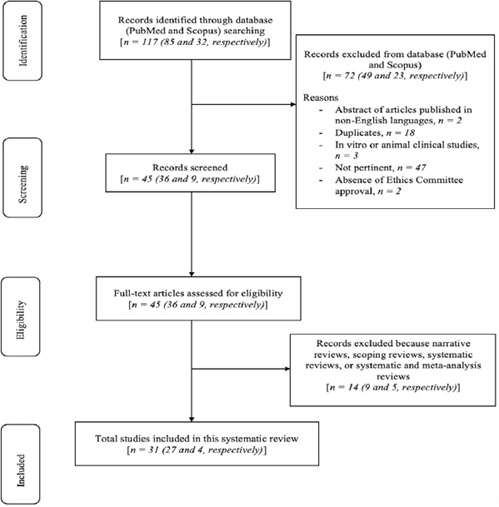
During the systematic literature review, the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) consensus were followed (Table S1) [16].
The medical subject heading (MeSH) terms were bacteria, dental plaque, evidence-based practice, maxillomandibular fixation, microbiota, operative procedures, and orthognathic surgery; an electronic search was carried out with PubMed (MEDLINE) and Scopus databases. Articles published in the years from 2002 to 2022 were targeted. The duration of data extraction was between 10 and 12 weeks. The last search was performed on 19 December 2022. Three calibrated reviewers (M.P., M.G.N., and F.P.) performed the search. Disagreements and discrepancies were resolved by consensus and three other reviewers were consulted (A.S., U.G., and F.S.). Quality assessment was performed by two reviewers (M.P. and A.S.). Relevant articles were reviewed by reading the full texts, recording the results, and identifying any similar studies that met the inclusion criteria. Non-relevant studies were excluded by thoroughly analyzing the titles and abstracts of the articles searched.
The strategies developed and used for each electronic database are presented in Table S2.
2.4. Flow Chart of the Systematic Review Process
The primary search identified 117 articles based on MeSH terms. Following this, 72 articles were removed because 2 abstracts of articles published in non-English languages, 18 duplicates, 3 in vitro or animal clinical studies, 47 because they were not pertinent (not useful to answer focused questions, content not corresponding to abstract, more focused on pain and/or complications related to orthognathic surgery), 2 because of the absence of Ethics Committee approval, and 45 articles were screened based on title and abstracts. The remaining 45 full-text articles were assessed for eligibility. Additionally, 14 full-text articles were further excluded as case reports, narrative reviews, systematic reviews, or systematic and meta-analysis reviews. The 31 relevant articles were finally included and analyzed in this systematic review. The flow chart of the review process is described in Fig. (1).
Table S3 shows the studies excluded from this review and the reasons for exclusion [18-31].
The studies were from three categories: controlled intervention studies [32-52], before-after (pre-post) studies with no control Group [53-55], and observational cohort and cross-sectional studies [56-62].
2.5. Risk of Bias
The Cochrane Collaboration tool for assessing the risk of bias was used to evaluate the reviewed articles (Table 1). Table S4 shows the criteria for judging the risk of bias in the “risk of bias” assessment tool. This review has a low risk of bias since the number of green symbols (low risk of bias, 103) prevails over the number of yellow symbols (high risk of bias, 52).
| - | Random Sequence Generation | Allocation Concealment | Blinding | Incomplete Outcome Data | Selective Reporting |
|---|---|---|---|---|---|
| Chen et al., 2015 [32] |

|

|

|

|

|
| Barbosa Cavalcanti et al., 2022 [33] |

|

|

|

|

|
| Ruf et al., 2004 [34] |

|

|

|

|

|
| Bertossi et al., 2013 [35] |

|

|

|

|

|
| Choi et al., 2015 [36] |

|

|

|

|

|
| Li et al., 2022 [37] |

|

|

|

|

|
| Mahmoud et al., 2022 [38] |

|

|

|

|

|
| Van Hemelen et al., 2015 [39] |

|

|

|

|

|
| Chen, H. et al., 2021 [40] |

|

|

|

|

|
| Li et al., 2021 [41] |

|

|

|

|

|
| Schneider et al., 2019 [42] |

|

|

|

|

|
| Cui et al., 2022 [43] |

|

|

|

|

|
| Wang et al., 2022 [44] |

|

|

|

|

|
| Chen, C. et al., 2021 [45] |

|

|

|

|

|
| Pelo et al., 2017 [46] |

|

|

|

|

|
| Bengtsson et al., 2018 [47] |

|

|

|

|

|
| Hanafy et al., 2019 [48] |

|

|

|

|

|
| Jaeger et al., 2020 [49] |

|

|

|

|

|
| Camacho et al., 2020 [50] |

|

|

|

|

|
| de Rezende et al., 2018 [51] |

|

|

|

|

|
| Bevilacqua et al., 2016 [52] |

|

|

|

|

|
| Gruber et al., 2005 [53] |

|

|

|

|

|
| Baan et al., 2016 [54] |

|

|

|

|

|
| Badiali et al., 2020 [55] |

|

|

|

|

|
| Cascino et al., 2021 [56] |

|

|

|

|

|
| Kee et al., 2022 [57] |

|

|

|

|

|
| Borikanphanitphaisan et al., 2021 [58] |

|

|

|

|

|
| Chen et al., 2022 [59] |

|

|

|

|

|
| Weinspach et al., 2012 [60] |

|

|

|

|

|
| Haffajee et al., 2008 [61] |

|

|

|

|

|
| Farronato et al., 2014 [62] |

|

|

|

|

|
2.6. Quality Assessment of Included Studies
This review was carried out by assessing the risk of bias by performing quality analysis of the clinical studies through the National Heart, Lung, and Blood Institute (NHLBI) Quality Assessment of Controlled Intervention Studies, Before-After (Pre-Post) Studies with No Control Group, and for Observational Cohort and Cross-Sectional Studies [17].
NHLBI Quality Assessment of Controlled Intervention Studies is shown in Table S5. NHLBI Quality Assessment for Before-After (Pre-Post) Studies with No Control Group is shown in Table S6. NHLBI Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies is shown in Table S7.
3. RESULTS
Table 2 shows the baseline characteristics of patients included in the selected studies. In the selected studies, the number of patients ranged from 7 to 300, the % of women ranged from 37.5% to 82.61%, the mean age (SD or range) ranged from 23.10 ± 3.3 to 54.1 ± 10. 5 and, finally, the types of malocclusions considered ranged from skeletal classes I-II-III malocclusions, class II division 1 malocclusion, dentoskeletal deformity and/or mandibular prognathism, maxillary deficiency with mandibular excess, maxillary excess with mandibular deficiency, and asymmetric deformity to anterior open bite.
| Authors | No of Patients | % Women | Mean Age (Years), Mean (SD or Range) | Type of Malocclusion |
|---|---|---|---|---|
| Chen et al., 2015 [32] |
Trial Group: 24 Control Group: 24 | Trial Group: 70.83% Control Group: 66.67% |
Trial Group: 23.78 (18-34) Control Group: 24.13 (19-57) |
Skeletal class III malocclusion |
| Barbosa Cavalcanti et al., 2022 [33] |
Trial Group: 20 Control Group: 20 | 26/40 (65%) | Trial Group: 30.25 (18-49) Control Group: 28.6 (18-41) |
Skeletal class III malocclusion |
| Ruf et al., 2004 [34] |
Group 1: 46 Group 2: 23 |
Group 1: 82.61% Group 2: 82.61% |
Group 1: 26 (15.7-47.6) Group 2: 21.9 (15.7-44.4) |
Class II division 1 malocclusion |
| Bertossi et al., 2013 [35] |
Trial Group: 55 Control Group: 55 |
NR | NR | Dentoskeletal deformity and/or mandibular prognathism |
| Choi et al., 2015 [36] |
Trial Group: 32 Control Group: 24 |
40/56 (71.43%) | 22.4 | Skeletal class III malocclusion |
| Li et al., 2022 [37] |
Trial Group: 49 Control Group: 49 |
58/98 (59.18%) | 24.4 (18-33) | Mandibular prognathism |
| Mahmoud et al., 2022 [38] |
Trial Group: 12 Control Group: 12 |
Trial Group: 33.33% Control Group: 58.33% |
18-26 | Skeletal III class malocclusion |
| Van Hemelen et al., 2015 [39] |
Trial Group: 31 Control Group: 35 | 37/66 (56.06%) | NR | Skeletal classes II–III malocclusions |
| Chen, H. et al., 2021 [40] |
DOS Group: 21 DT Group: 20 CROS Group: 20 |
DOS Group: 71.43% DT Group: 75% CROS Group: 70% |
DOS Group: 23 (19-27) DT Group: 24 (19-32) CROS Group: 23 (19-31) |
Maxillary deficiency with mandibular excess, maxillary excess with mandibular deficiency, asymmetric deformity |
| Li et al., 2021 [41] |
Trial Group: 27 Control Group: 31 |
Trial Group: 55.55% Control Group: 67.74% |
Trial Group: 23.8 (19-32) Control Group: 23.6 (19-33) |
Skeletal classes II–III malocclusions |
| Schneider et al., 2019 [42] |
Conventional Planned Group: 12 Virtual Planned Group: 9 |
12/21 (57.14%) | 31.1 (23-52.1) | Skeletal class II malocclusion |
| Cui et al., 2022 [43] |
Trial Group: 20 Control Group: 20 |
16/40 (40%) | 16-35 | Maxillary-mandibular malformations |
| Wang et al., 2022 [44] |
Trial Group: 14 Control Group: 14 |
Trial Group: 71.43% Control Group: 57.14% |
Trial Group: 21.36 ± 4.53 Control Group: 22.43 ± 3.37 |
Maxillary deficiency, maxillary excess, maxillary asymmetry deformity |
| Chen, C. et al., 2021 [45] |
Trial Group:> 26 Control Group: 26 |
24/52 (46.15%) | 23.4 (18-37) | Skeletal classes I–II–III malocclusions, facial asymmetry and/or malformation, anterior open bite |
| Pelo et al., 2017 [46] |
Trial Group: 15 Control Group: 15 |
20/30 (66.67%) | 30.2 (19-45) | Skeletal classes II–III malocclusions |
| Bengtsson et al., 2018 [47] |
Trial Group: 28 Control Group: 29 |
Trial Group: 53.57% Control Group: 41.38% |
Trial Group: 20.5 Control Group: 21.1 |
Skeletal III class malocclusion |
| Hanafy et al., 2019 [48] |
Trial Group: 16 Control Group: 16 |
Trial Group: 56.25% Control Group: 56.25% |
Trial Group: 22.56 (19-28) Control Group: 22.69 (19-28) |
Skeletal classes II–III malocclusions |
| Jaeger et al., 2020 [49] |
Scalpel Group: 10 Electrocautery Group: 10 Diode Laser Group: 10 |
20/30 (66.7%) | 28.8 (18-50) | Dentofacial deformities with SARME or bimaxillary orthognathic surgery indications |
| Camacho et al., 2020 [50] |
Group 1 19 Group 2 18 Control Group: 19 |
Group 1 63.2% Group 2 72% Control Group: 58.4% |
Group 1 25 (20-40) Group 2 24.7 (20-40) Control Group: 23.8 (18-40) |
Dentofacial deformities with mandibular orthognathic surgery indication |
| de Rezende et al., 2018 [51] |
Trial Group: 40 Control Group: 42 |
53/82 (64.63%) | 31.5 (17-54) | Dental-skeletal facial deformities |
| Bevilacqua et al., 2016 [52] |
Group 1: 20 Group 2: 20 Group 3 20 |
Group 1: 50% Group 2: 65% Group 3 60% |
Group 1: 54.1 ± 10.5 Group 2: 48.5 ± 15.2 Group 3 47.5 ± 14.4 |
NR |
| Gruber et al., 2005 [53] |
7 | 5/7 (71.43%) | 16-37 | Skeletal classes II–III malocclusions |
| Baan et al., 2016 [54] |
10 | 6/10 (60%) | Females: 25.8 (17-40) Males: 27.5 (17-45) |
Skeletal class II malocclusion |
| Badiali et al., 2020 [55] |
22 | 15/22 (68.18%) | 26 (18-43) | Skeletal classes II–III malocclusions, class I facial asymmetry, anterior open bite |
| Cascino et al., 2021 [56] |
Group 1: 50 Group 2: 50 |
39/100 (39%) | 28.5 (21-44) | Skeletal classes II–III malocclusions |
| Kee et al., 2022 [57] |
Group 1: 32 Group 2: 32 |
Group 1: 37.5% Group 2: 46.87% |
Group 1: 21.3 ± 3.0 Group 2: 23.5 ± 6.2 |
Skeletal class III malocclusion |
| Borikanphanitphaisan et al., 2021 [58] |
Group 1: 31 Group 2: 26 |
Group 1: 64.5% Group 2: 65.3% |
Group 1: 24.6 ± 5.9 Group 2: 26.4 ± 7.4 |
Skeletal classes II–III malocclusions and skeletal class I asymmetry |
| Chen et al., 2022 [59] |
Cohort 1: 33 Cohort 2: 37 |
Cohort 1: 66.67% Cohort 2: 64.86% |
Cohort 1: 23.10 ± 3.3 Cohort 2: 23.15 ± 3.5 |
Maxillary deficiency with mandibular excess, maxillary excess with mandibular deficiency, asymmetric deformity |
| Weinspach et al., 2012 [60] |
15 | 8/15 (53.33%) | 24.9 ± 7.7 | Skeletal classes II–III malocclusions |
| Haffajee et al., 2008 [61] |
187 | 140/187 (74.87%) | 46.8 (22-74) | NR |
| Farronato et al., 2014 [62] |
300 | NR | 5-57 | Dental-skeletal facial deformities and edentulism |
Evidence of studies included in this systematic review (design, inclusion and exclusion criteria, aim, and results) is shown in Table S8.
After orthognathic surgery, the efficacy and subsequent postoperative changes in the nasolabial region of two-wing base cinch suture techniques were evaluated. The results showed an increase of 0.81 ± 1.87 mm in the cutaneous height of the upper lip a decrease of 0.76 ± 1.56 mm in the lower prolabial width, an increase of 0.31 ± 1.31 mm in nasal width, and an increase of 0.97 ± 1.60 mm in columellar length [32]. In addition, the nasal base enlargement of patients undergoing Le Fort I osteotomy was evaluated, and two suture techniques of the wing cinch were compared, showing an increase in the alar base width in both groups, with a significant difference between the means. It was observed that the external technique better controlled alar base width after Le Fort I osteotomy [33].
The extent to which Herbst treatment for adults is an alternative to orthognathic surgery was evaluated, showing that skeletal and soft tissue facial profile convexity was reduced significantly in both groups, but the amount of profile convexity reduction was larger in the surgery group. The success and predictability of Herbst treatment for occlusal correction were as high as for surgery [34].
The use of piezoelectric osteotomy was compared with the conventional approach in terms of operative time, intraoperative blood loss, cut quality, nerve injury, and cost, concluding that surgical time in the Trial Group was reduced, with a mean for the mandibular osteotomy between 3 minutes 31 seconds and 5 minutes 2 seconds, whereas in Control Group, the surgical time was between 7 minutes 23 seconds and 10 minutes 22 seconds. The surgical time in the Trial Group for the Le Fort I osteotomy was between 5 minutes 17 seconds and 7 minutes 55 seconds in the Trial Group and between 8 minutes 38 seconds and 15 minutes 11 seconds in the Control Group. All patients in group A had a low blood loss (<300 mL) versus patients of the Control Group who had a medium to high blood loss (400 mL). Inferior alveolar nerve sensation was retained in 98.2% of the Trial Group versus 92.7% in the Control Group at 6 months postoperative testing [35].
A surgery-first approach without presurgical orthodontic treatment is possible and can give similar results to standard orthognathic surgery. The statistical analysis showed that changes in skeletal cephalometric landmarks were similar between the surgery-first and standard approach groups, according to each period. The cephalometric landmarks relating to the dental component showed changes between treatment groups at different time points but similar final values [36].
Comparing skeletal stability in anteroposterior and vertical dimensions between intraoral vertical ramus osteotomy (IVRO) and sagittal split ramus osteotomy (SSRO) as mandibular retraction surgery, within two years after surgery, it was found that more surgical relapse in the horizontal direction in the SSRO group than in the IVRO group (0.27 mm ± 0.34 mm) vs (0.10 mm ± 0.29 mm). More absolute changes in the SSRO group than in the IVRO group at postoperative 2 years. The amounts of change as percentages of total mandibular setback were 1.3% and 3.5% in the IVRO group and SSRO group, respectively. There were no differences in vertical changes between the two groups at any time points [37].
It was assessed whether the orthognathic maxilla-first or mandible-first sequence in bimaxillary orthognathic surgery results in greater jaw stability in patients with skeletal class III malocclusion, showing that statistical analysis of the lateral cephalometric measurements reached statistical significance differences immediately after surgery and 6-month after in both groups. Clinically, this was not significant as the mean difference at parameters concerned with maxillary advancement and rotation is about 2 mm only [38].
Comparing the accuracy of a traditional 2D technique and a 3D computerized prediction method showed that statistically significant difference between 2D and 3D soft tissue planning, but no statistically significant difference between 2D and 3D planning and the actual soft tissue outcome [39].
The accuracy of three methods for transferring the jaw plane to the surgical procedure was compared (conventional resin occlusal splints, CROS, digital occlusal splints, DOS, and digital templates, DT), concluding that the distance was significantly smaller in the DT group (1.17 ± 0.66mm) when compared to both the CROS group (2.55 ± 0.95mm, P<0.05) and DOS group (2.15 ± 1.12mm). However, the difference between the CROS group and the DOS group was not statistically significant. These findings indicate that using digital templates results in the best performance in transferring the surgical plan to the operating environment as compared to the other two types of splints [40].
Whether the use of patient-specific implants can result in more accurate jaw position than the use of CAD/CAM surgical splints in orthognathic surgery was evaluated, showing that maxilla position discrepancy was 1.41 ± 0.58 mm in the patient-specific implant group and 2.20 ± 0.94 mm in the splint group; the between-group difference was significant. For the Trial Group, the largest translation discrepancy was 1.02 ± 0.66 mm in the anteroposterior direction, and the largest orientation discrepancy was 1.85 ± 1.42 degrees in pitch. For the Control Group, the largest translation discrepancy was 1.23 ± 0.93 mm in the mediolateral direction, and the largest orientation discrepancy was 1.72 ± 1.56 degrees in pitch [41]. Furthermore, the accuracy of splints, time to surgery, and costs of virtual surgical planning (VSP) versus conventional surgical planning (CSP) in bimaxillary orthognathic surgery was analyzed, highlighting that VSP appears to be a more accurate method for orthognathic treatment planning with significant differences in the angle outcome. There were significant differences in splint accuracy in favour of CAD/CAM splints. VSP significantly reduced the duration of the operation. Nevertheless, VSP is more expensive than CSP [42].
The accuracy of implanting an intermaxillary fixation screw (IMFS) with a digital guide to reduce root damage was evaluated, finding that in the Trial Group, there was no case of root damage, the incidence of the periodontal ligament injured was 22.1%, and 77.9% IMFSs were placed without contacting adjacent anatomic structures. In the Control Group, the incidence of root damage had been up to 20.8%, 31.7% of IMFSs injured the periodontal ligament, and only 47.5% of IMFSs were placed between the roots [43]. Moreover, the accuracy of a new type of osteotomy guide (EOG) was compared with the traditional osteotomy guide (TOG) by evaluating the control of osteotomy on the inner and posterior maxillary walls, concluding that all positioning deviations of both osteotomy guides were <0.3 mm. The osteotomy depths on the inner and posterior walls with the EOG and TOG deviated by 0.789 ± 1.179 mm, 1.811 ± 1.345 mm, and 0.648 ± 0.999 and 1.262 ± 0.942 mm, respectively. The angles of deviation of the osteotomy direction on the inner and posterior walls by the EOG and TOG were 2.025 ± 2.434 degrees, 5.069 ± 2.391 degrees, and 2.772 ± 2.979 degrees, and 8.653 ± 4.690 degrees, respectively [44].
The accuracy of a new navigation method called Ci-Navi compared with conventional navigation methods in bimaxillary orthognathic surgery was also evaluated, showing that in the Trial Group, the overall mean linear difference was 0.79 mm (0.62 mm for the maxilla and 0.88 mm for the mandible) and the overall mean angular difference was 1.20°. In 23 cases, the difference from the upper incisor point to the Frankfort horizontal plane, midfacial sagittal plane, and coronal plane was less than 1 mm. In the Control Group, the overall mean linear difference was 1.98 mm (1.76 mm for the maxilla and 2.02 mm for the mandible) and the overall mean angular difference was 2.08°. The difference from the upper incisor point to the Frankfort horizontal plane, midfacial sagittal plane, and coronal plane was less than 1 mm in 15 cases [45].
Regarding the Oral Health-Related Quality of Life (OHRQoL), the differences noted by patients between the traditional orthognathic approach and the first-choice surgical approach were investigated, concluding that significant differences in terms of the Orthognathic Quality of Life Questionnaire, and the Oral Health Impact Profile scores within groups between the first and last administrations of both questionnaires. Differences in the control group between the first and second administrations were also significant. Questionnaire scores showed an immediate increase in quality of life after surgery in the surgery-first group and an initial worsening during orthodontic treatment in the traditional approach group followed by postoperative improvement [46]. In addition, possible differences in OHRQoL after orthognathic treatment were investigated, depending on the 2D or 3D planning technique, highlighting that no statistically significant difference regarding OHRQoL was found between the studied planning techniques. The difference between pretreatment and posttreatment increased in both groups but to a higher level in the 3D group. A difference between pretreatment and posttreatment OHRQoL was shown for both groups, indicating the increased quality of life after treatment [47]. Finally, quality of life after orthognathic surgery using CAD/CAM bone splints versus classic occlusal wafers was evaluated in patients with dentofacial deformities, stating that the mean orthognathic quality of life questionnaire (OQLQ) overall score change of 24.375 ± 11.96 took place in Trial Group patients while Control Group showed a mean change of 23 ± 8.39 but computer-assisted surgery did not show any significant improvement over the classic approach [48].
The efficacy and safety of the diode laser during circumvestibular incisions for Le Fort I osteotomy in orthognathic surgery were evaluated compared with conventional electrocautery and scalpel techniques, showing that regarding bleeding, the incisions performed with diode laser promoted a lower bleeding rate compared with scalpel and electrocautery. The diode surgical laser was effective during the incision procedure but required a longer time to perform the incisions compared with the other techniques evaluated. No statistically significant difference was detected between groups regarding total surgical time or other safety parameters [49]. Moreover, the effect on post-surgical edema after mandibular orthognathic surgery was compared between two different laser power densities (Group 1 and Group 2), and oral medication administration with nonsteroidal anti-inflammatory drugs, showing that the differences between the groups were generally not significant except for commissure - right and left gonion when compared laser Groups vs Control Group. Initial changes between groups were significantly different except for the measurement from commissure to right tragus Group 1 vs Control Group and from commissure to left tragus Group 2 vs Control Group. The faster resolution of edema occurred in Group 2 [50]. The effect of PBMT with a GaAlAs diode laser (780 nm) as an adjuvant therapy to improve mouth opening in the postoperative period of different orthognathic surgery modalities was also tested, highlighting that there were no significant differences between the surgically assisted rapid maxillary expansion (SARME) and isolated maxillary/mandibular surgery groups. In the bimaxillary groups, average mouth opening was increased in all patients who received PBMT, significantly so in male patients [51].
The staining effect of a 0.2% chlorhexidine (CHX)-containing anti-discoloration system (ADS) mouthwash compared with a 0.12% and 0.2% CHX mouthwash after periodontal surgery was evaluated by spectrophotometric clinical analysis, showing that no statistical differences were found for dental pigmentation among the mouth rinses over time nor for discomfort at each follow-up examination. A slightly lower acceptance rate was observed for 0.2% CHX [52].
Preliminary results and experiences of using an ultrasonic bone cutting device in the bilateral sagittal split osteotomies of the mandible (BSSRO) were presented, with a focus on possible damage to the IAN, concluding that Subjective neurosensory disturbances of the IAN showed a continuous decrease from 57.1% (eight sides) 2 months after the surgical procedure to 14.3% (2 sides) after 5 months and to 7.1% 7 months after BSSRO [53].
A novel instrument, the OrthoGnathicAnalyser, has been validated in patients undergoing bimaxillary osteotomy, indicating that low intra-observer and inter-observer variations in measurement error (<0.25 mm) and high intraclass correlation coefficients (>0.97) were found, supportive of the observer-independent character of the OrthoGnathicAnalyser [54].
The quality of reproduction of mandibular anatomy was analyzed using a mandible-first guided procedure- patient-specific implants (PSI), showing that correlations between obtained rami and plate discrepancies and between planned rami displacements and obtained rami discrepancies were calculated. Intraoperatively, all PSIs were successfully applied [55].
Intraoperative time, facial swelling, degree of pain (VAS scale), recovery time, and neurosensory disturbances were evaluated in patients undergoing orthognathic surgery with piezoelectric or saw devices, suggesting that intra-operative time is unchanged, but patients operated with the Piezo devices requested fewer painkilling medication and were dismissed on the second day after the surgery. Neurosensory recovery was statistically significant in the Piezo group [56].
Changes in the alveolar bone around the mandibular incisors in patients with Class III skeletal malocclusion treated with a surgical (SFA) and conventional orthognathic (COS) approach were investigated using cone-beam computed tomography scans, revealing that the vertical bone levels and horizontal bone thickness of the labial and lingual sides and the area of the alveolar bone around the mandibular incisors were reduced after treatment in both SFA and COS groups. Vertical bone loss was more prominent than horizontal bone loss after treatment in both groups, and alveolar bone loss was greater on the lingual side than on the labial side. There were no significant differences in alveolar bone changes around the mandibular incisor between the SFA and COS groups [57].
The accuracy of bimaxillary orthognathic surgery was studied in relation to different sequences (maxillary first or mandibular first) and different intermediate splint thicknesses, revealing that mandible-first surgery resulted in more accuracy in the vertical dimension. Thick intermediate splints provided better control (less error) of upper central incisors in the sagittal position (thick splint, 1.38 ± 1.17 mm; thin splint, 2.13 ± 1.38 mm). Overall accuracy was not affected by splint thickness [58].
The accuracy of using molded occlusal splints versus templates in simple and complicated cases was compared, showing that the average deviation was significantly smaller in the complicated cases in the DT Cohort (1.37 mm; 95% confidence interval, 1.08-1.66 mm) than that in the DOS cohort (2.47 mm; 95% confidence interval, 1.92-3.02 mm). The deviations in the anteroposterior direction of complicated cases in the DT cohort were smaller than the corresponding values of the DOS cohort. There is no significant difference between the deviation values of simple and complicated cases using templates [59].
Finally, the influence of orthognathic surgery on the development of periodontal and microbiological changes was evaluated, concluding that a significant increase in plaque index (T0-T1) was followed by a significant decrease (T1-T2). Apart from Eikenella corrodens (P=0.036), no significant microbiological changes were recorded. PPD significantly increased on oral sites (P=0.045) and gingival recession (GR), especially on buccal sites. In the incision area, the development of GR was significantly higher on the buccal than on the oral sites. Both gingival biotypes were affected by GR [60]. In addition, microbial communities in supragingival biofilm samples were examined, showing that six complexes were formed for the baseline samples. Similar complexes were formed for the samples taken 3-24 months post-therapy. However, distinct changes were observed in microbial communities in samples taken during the 7 days of plaque redevelopment. The complexes related to clinical parameters of periodontal disease were evaluated [61]. Lastly, qualitative and quantitative changes occurring within the oral bacterial flora of different groups of patients following oral preventive protocols during dental treatment phases required, assessing that the Mean Plaque Index Score of most patients generally decreased during the various treatment phases and hence the overall bacterial count. However, there was a slight increase in the plaque index in patients undergoing orthodontic surgery after placement of the orthodontic appliance and patients undergoing combined orthodonticsurgical treatment during the intermaxillary fixation phase. It was found that the coccoidal bacterial form was the most prevalent [62].
4. DISCUSSION
Orthognathic surgery allows the correction of a wide variety of anomalies of the jaws and face, producing, in addition to the correction of malocclusion, significant aesthetic changes along with other benefits, such as chewing and breathing, which are often improved [63]. Patients who can benefit from orthognathic surgery have an established dysgnathia, so orthodontic treatment is not considered conclusive [64]. Severe open bite, skeletal class II anomalies, skeletal class III anomalies, prognathism with reverse bite, obstructive sleep apnea syndrome (OSAS), as well as facial and mandibular asymmetries, can be treated through surgical therapy [65].
A good understanding of facial growth, the different treatment options, and the effects of surgery on the post-operative growth pattern will enable the practitioner to use the most appropriate technique for each of their patients and improve long-term treatment results [66].
4.1. Clinical Studies on Humans’ Evidence of Orthognathic Surgery Techniques
Le Fort I osteotomy is the most used surgical technique to correct maxillary deformities and, despite the good skeletal results obtained, it causes a muscular detachment of the nasal region promoting enlargement of the nasal wing base [32]. External and internal suture techniques can be used to reconstitute the nasal wing base, and in particular, recent studies have shown that the external technique appears to be more effective than the internal technique in controlling wing base widening, although future studies are needed to confirm these findings [33].
Regarding adult Class II Division 1, the comparison of the effects of dentoskeletal treatment achieved by a combined surgical-orthodontic approach versus the application of Herbst's appliance alone was performed, obtaining nonsignificant results [34].
Furthermore, it has been shown that piezoelectric osteotomy has reduced surgical time, blood loss, inferior alveolar nerve injury in a bimaxillary osteotomy, postoperative swelling, use of pain medication, faster healing, greater recovery of lower lip sensitivity, and the absence of macrovibration makes the instrument easier to use and allows for greater intraoperative control with increased safety in cutting in difficult anatomic regions [35, 53, 56].
A simulation of pre-surgical orthodontic treatment was performed to determine the final occlusion between the maxilla and mandible, and subsequently, changes in cephalometric landmarks were compared in patients with Class III dentofacial skeletal deformity undergoing “surgery-first” versus standard orthognathic surgery [36]. Significant results demonstrated how the “surgery-first” approach is predictable and applicable for treating class III dentofacial deformities [36]. However, it is important to point out that both the “surgery-first orthognathic approach” and conventional orthognathic surgery can trigger degeneration of the alveolar bone around the mandibular incisors after treatment in patients with mandibular prognathism [57].
Furthermore, it has recently been shown that in patients with mandibular prognathism, horizontal skeletal stability following orthognathic surgery is superior if an intraoral vertical ramus osteotomy is performed compared with a sagittal split ramus osteotomy [37]. This possible benefit may be an important key factor when deciding which osteotomy technique to use in these patients.
There are two different types of orthognathic surgical sequences: the maxilla-first approach, the standard orthognathic sequence, and the mandible-first approach devised through the evolution of rigid internal fixation to eliminate errors that might be encountered during preoperative bite registration [67].
Analyzing hard and soft tissue landmarks to evaluate maxillary stability in patients with skeletal class III malocclusion, no significant differences were found between the two types of surgical approaches, and, as a result, it can be stated that the mandible-first approach can be a reliable method to achieve high maxillary stability [38].
However, it has recently been shown that the mandible-first approach was found to be more accurate in the vertical dimension and the thickness of the splints has no effect on the overall accuracy if an appropriate selection of intermediate splints is made to maintain the intermediate condylar position [58].
Advances in three-dimensional (3D) virtual surgery programs have allowed their comparison with conventional two-dimensional (2D) planning techniques, showing statistically significant differences between 2D and 3D soft tissue planning i.e., the 3D planning approach appears to be more accurate than 2D planning, for soft tissue [54]. In contrast, comparable results were shown between the two planning techniques for hard tissues [39], although the use of Computer-Aided Design and Manufacturing (CAD/CAM) has proven effective and accurate in transferring virtually planned mandibular anatomy to the patient in orthognathic mandible-first surgery [40, 41, 55,68-70].
Moreover, it has recently been shown that the use of CAD/CAM printed guide masks shows better accuracy in jaw repositioning than CAD/CAM printed occlusal splints and a significant reduction in the duration of the intervention [42, 59]. In addition, CAD/CAM surgical guides can also be used to implant intermaxillary fixation screws more accurately, reducing the incidence of root and periodontal ligament damage [43].
CAD/CAM technology has also been used recently for the fabrication of a patient-specific osteotomy guide for performing Le Fort 1 osteotomy, showing that it is more precise than using the traditional osteotomy guide or CAD/CAM surgical splints, resulting in better manipulation of the direction and depth of osteotomy on the inner and posterior maxillary walls and providing greater surgical safety [41, 44].
In addition, CAD/CAM has also been tested during surgery through computer-aided intraoperative navigation (Ci-Navi), performing a Le Fort I osteotomy and repositioning the upper jaw in the designated position by taking advantage of Ci-Navi assistance in real-time, highlighting its superiority over conventional methods in facilitating accurate repositioning of bone segments in bimaxillary orthognathic surgery [45].
Through the administration of quality-of-life questionnaires such as the Oral Health Impact Profile (OHIP) and the Orthognathic Quality of Life Questionnaire-22 (OQLQ-22), surgery-first has been shown to immediately improve quality of life and avoid the psychological discomfort caused by lengthy pre-surgical orthodontic treatment [46]. However, CAD/CAM surgery showed no significant psychological improvement compared with the use of classic occlusal wafers in patients with dentofacial deformities [47, 48].
Finally, diode Laser and photobiomodulation therapy (PBMT) has also been applied in patients undergoing orthognathic surgery: diode Laser was shown to be more effective and safer during circumvestibular incisions for Le Fort I osteotomy than conventional devices [49], and PBMT with an energy density of 68.33 J/cm2 was the most effective adjuvant to oral nonsteroidal anti-inflammatory drugs (NSAIDs) in reducing postsurgical edema [50] and could improve mouth opening in men undergoing bimaxillary orthognathic surgery [51].
4.2. Oral Microbiota Changes by Intermaxillary Fixation
Negligence in orthopaedic preliminaries can invalidate the occlusion inconsistencies that are routinely present when osteosynthesis does not include intermaxillary fixation: comparison of bone stumps fatally maintains congruence defects, the dimensions of which are amplified at the level of the occlusion, which, in contrast, does not tolerate even slight discrepancies [71].
However, as in other surgical procedures [72], intermaxillary fixation leads to impaired oral hygiene and, consequently, orthognathic surgery may lead to increased plaque accumulation and microbiological changes, encouraging the proliferation of periodontopathogenic bacteria, and leading to the formation of periodontal pockets [43].
The studies observed a temporary impairment of oral hygiene linked to minimal changes in the periodontal microflora, but no long-term increase in the concentration of periodontal bacteria. In particular, the concentration of the bacillus Eikenella corrodens (Gram-negative, period- ontopathogenic, responsible for the onset of infective endocarditis) tends to increase temporarily in a statistically significant manner (P=0.037) during the period of fixation; however, there is a statistically significant decrease (P=0.017) in this concentration by the end of the period of intermaxillary fixation [60].
The postoperative healing period following orthognathic surgery is generally associated with reduced oral hygiene resulting from a lack of mechanical plaque control (first postoperative week), the application of fixation in combination with elastics (first to sixth postoperative week), fixed orthodontic appliances and postoperative symptoms (pain, swelling, reduced mouth opening). It has been shown that an uncontrolled accumulation of bacterial deposits over a period promotes a shift toward periodontal-pathogenic bacterial species [61].
However, the results of these studies revealed that, apart from the short-term increase in E. corrodens concentrations, there were no statistically significant changes in periodontal microflora; the absence of microbiological changes may be due to the perioperative administration of penicillin G., the postoperative application of a chlorhexidine mouthwash and/or the ability of patients to perform adequate mechanical plaque control after orthognathic surgery [60].
In a subsequent study, intermaxillary fixation in orthodontic patients has been shown to increase plaque index (IP) up to 21.3%, with a prevalence of the coccoid bacterial form. This index decreases to 8% when the patient can independently resume correct oral hygiene at the end of the fixation period. The trend in the total number of cocci and bacilli in the various treatment stages shows a path like that of IP, i.e., a progressive improvement [62].
Assessing the subject's dietary habits and nutritional status before surgery is essential. Normal diets with high protein and vitamin C intake are recommended in normal-weight patients. Underweight patients should follow a high-protein, high-vitamin, and high-calorie diet [73].
Full-mouth disinfection can be used to rapidly reduce bacterial load and hyperemia before surgery: it is also associated with a strict home oral hygiene protocol, i.e., brushing of tooth surfaces, tongue cleansing with 1% chlorhexidine gel for one minute, nebulizer applications and rinses with 0.2% chlorhexidine mouthwash twice a day, and irrigation of periodontal pockets with 1% chlorhexidine gel [52].
One week after surgery, the patient, who has an intermaxillary fixation, must be motivated to resume oral hygiene using a small toothbrush for the buccal surfaces, chlorhexidine-based mouthwash, and a tongue cleaner for the lingual surfaces. Rinses with this type of mouthwash lead to an improvement in the control of the bacterial forms in the plaque and in the amount of plaque itself, as well as making it possible to reach sites that cannot be reached in any other way. After the fixation is removed, it is important to evaluate the oral hygiene techniques learned in the pre-surgical phase, a professional oral hygiene session is carried out, and the resumption of the diet is checked by monitoring the nutritional status of the subject since a correct diet favours the healing, immune and blood coagulation processes [62].
This review has some limitations. No information specialists or academic librarians have been included in the conduction of the electronic search. Moreover, it did not consider all articles in the literature, concerning grey literature and non-indexed research. Furthermore, the results may differ according to the population considered. Finally, because there are few studies in the literature related to a specific topic, conducting a specific review on a single topic was impossible.
Future research prospects could include further randomized controlled clinical trials that should be conducted to evaluate the superiority of external sutures in controlling enlargement of the nasal wing base post-Le Fort 1, as well as the intraoral vertical ramus osteotomy role in horizontal skeletal stability in patients with Class III malocclusion, the usefulness of Laser in orthognathic surgery, and, finally, the possible quantitative and qualitative changes of the many other microorganisms that make up the oral microbiota, for which specific studies have not yet been performed to date.
Recent research showed that paraprobiotics [74], lysates [75], postbiotics [76], and other natural compounds [77] showed promising results in clinical dentistry. Future research is needed to improve current knowledge about all these treatment possibilities in intermaxillary fixation.
CONCLUSION
Current knowledge on orthognathic surgery techniques is based on well-established traditional surgical concepts; However, excellent results have been obtained regarding new suture techniques to reconstitute the nasal wing base, new “surgery-first,” “maxilla-first,” and “mandible-first” surgical approaches in patients with Class III malocclusion, the greater precision and accuracy of patient-specific CAD/CAM osteotomy guidance for Le Fort 1 osteotomy compared with the use of traditional osteotomy guidance or CAD/CAM surgical splints, and, finally, definitive confirmations of the benefits associated with the use of lasers in orthognathic surgery. Regarding the change in oral microbiota following intermaxillary fixation post orthognathic surgery, the only statistically significant temporary bacterial increase recorded was for E. corrodens. No long-term increase in the concentration of periodontal bacteria was recorded and, moreover, good pre-surgical home oral hygiene, adherence to professional oral hygiene sessions during the fixation period and the re-establishment of correct post-surgical home oral hygiene allows a significant reduction in these values.
AUTHOR CONTRIBUTIONS
Conceptualization, F.S., and U.G.; methodology, F.S., and A.S.; software, U.G., and A.S.; validation, U.G., and F.S.; formal analysis, F.S., and A.S.; investigation, U.G., and A.S.; resources, F.S. and A.S.; data curation, U.G., and F.S.; writing – original draft preparation, M.P., M.G.N., and F.P.; writing – review and editing, F.S., A.S. and U.G.; visualization, F.S., M.P. and M.G.N.; supervision, U.G., and F.P.; and project administration, F.S., A.S., and U.G. All authors have read and agreed to the published version of the manuscript.
AVAILABILITY OF DATA AND MATERIAL
The data supporting the findings of the article will be available from the corresponding author [A.S] upon reasonable request.
ACKNOWLEDGEMENTS
Declared none.
SUPPLEMENTARY MATERIAL
Table S1: PRISMA 2020 checklist; Table S2: Search strategies for electronic databases; Table S2: Summary table of studies excluded in this systematic review; Table S3: Criteria for judging the risk of bias in the “Risk of bias” assessment tool; Table S4: Evidence of studies included in this systematic review; Table S5: NHLBI Quality Assessment of Controlled Intervention Studies; Table S6: NHLBI Quality Assessment Tool for Before-After (Pre-Post) Studies With No Control Group; Table S7: NHLBI Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies.


