All published articles of this journal are available on ScienceDirect.
The Influence of Occlusal Adjustment on Long-term Post-treatment Stability of Orthodontic Treatment
Abstract
Objective:
This study aimed to compare the long-term occlusal stability in patients treated orthodontically with and without occlusal adjustment.
Material and Methods:
This observational study followed the STROBE guidelines. The sample comprised 77 patients with class I malocclusion treated without dental extractions and without signs and symptoms of temporomandibular joint dysfunction (TMD), divided into two groups. Group 1 with occlusal adjustment comprised 37 patients, 16 males and 21 females, with mean initial, final, and post-retention ages of 18.33 (s.d.=3.96), 20.99 (s.d.=3.33), and 25.79 years (s.d.=3.34), respectively. The treatment time was 2.66 years (s.d.=1.57), and the time of post-retention evaluation was 4.80 years (s.d.=1.10). Group 2, without occlusal adjustment involved 40 patients, 21 males and 19 females, with mean initial, final, and post-retention ages of 18.07 (s.d.=3.03), 20.75 (s.d.=3.54), and 25.89 (s.d.=3.73) years, respectively. The treatment time was 2.68 years (s.d.=1.09) and the time of post-retention evaluation was 5.14 years (s.d.=1.36). The PAR and Little irregularity indices were measured in the initial, final, and post-retention dental casts. Intergroup comparison was performed using the independent t-test.
Results:
There was no statistically significant difference observed in the intergroup comparison of the PAR and Little irregularity indexes in all phases and periods evaluated.
Conclusion:
There was no significant difference found in the long-term post-treatment crowding and occlusal relapse between class I patients treated with orthodontic non-extraction with and without occlusal adjustment. The occlusal adjustment did not influence the alignment and occlusal post-retention stability.
1. INTRODUCTION
Dental occlusion is a complex and dynamic system. The orthodontist's role is vital in the ongoing care of orthodontic treatment due to its impact on occlusal balance. Orthodontists bear significant responsibility, as consistent attention and monitoring are required throughout the treatment process [1].
Orthodontic treatment aims at harmonious occlusion involving the neuromuscular system, temporomandibular joint, and teeth. The occlusal balance, considered by several authors as simultaneous and stable bilateral contact in a position of centric occlusion, adequate anterior incisor contact, and right and left canine-guided lateral disocclusion, is fundamental for the masticatory system [2].
Occlusal stability is one of the main goals of orthodontic treatment. In addition, a functional occlusion can be obtained when stable centric stops on all teeth in maximal intercuspation are reached [3]. This way, the occlusal adjustment can refine the dental relationship obtained after orthodontic treatment. It is speculated that orthodontic patients who undergo occlusal adjustment may experience increased stability and a shorter retention period [4]. Occlusal adjustment is the systematic remodeling of the occlusal anatomy of the teeth to minimize all occlusal disharmonies in the reflex mandibular occlusal positions [5, 6]. This procedure aims to achieve a stable, nontraumatic occlusal contact relationship between the maxillary and mandibular teeth in maximum intercuspation and all functional excursive contact positions [7]. Occlusal adjustment therapy has some clear indications, which are described as follows: to treat the relapse of anterior open bite [8, 9], and to correct interocclusal relationships and distribute forces in the posterior teeth, in surgical cases of adult or mutilated patients with asymmetric extractions, Bolton discrepancy, and irregular restorations or exceptional extraction protocol.
It was previously suggested that a great finishing of orthodontic treatment would minimize the relapse [2, 10, 11]. However, more recent studies have shown that better occlusal results do not guarantee nor increase the stability [12-15]. Some studies have even indicated that poorly finished occlusions tend to improve in the post-retention phase [12, 13]. The relationship between occlusal contacts and long-term stability after orthodontic treatment has also been discussed. Occlusal adjustment is believed to aid and potentially enhance the outcomes of orthodontic treatment by reducing relapse and promoting the stability of corrections after removing fixed appliances [4, 5, 16, 17]. Conversely, no evidence exists that occlusal adjustment enhances stability after orthodontic treatment. Therefore, this study aimed to compare the post-retention occlusal stability in patients treated orthodontically with and without occlusal adjustment.
2. MATERIALS AND METHODS
This observational study followed the STROBE guidelines. The sample was retrospectively obtained from the records of a pool of orthodontic patients from a private orthodontic clinic of the first author. All patients have signed an informed consent. This study has been approved by the Ethics Research Committee of Ingá University Center, with number 1.957.938.
The sample size was calculated based on an alpha significance level of 5% (0.05) and a beta value of 20% (0.2) to achieve 80% power to detect a difference of 0.9mm with a standard deviation of 1.38 in the mandibular Little irregularity index change between the post-treatment and long-term post-treatment stages [18]. The sample size calculation showed that 36 patients per group were needed.
Inclusion criteria were as follows: no signs and symptoms of temporomandibular joint dysfunction (TMD); class I malocclusion; orthodontic treatment with full maxillary and mandibular fixed appliances (slot 0.022” x 0.028”), with Edgewise mechanics and without extractions; permanent dentition, with all teeth irrupted up to the permanent first molars before the beginning of treatment; no anomalies of dental shape or size; absence of open bite and anterior and posterior crossbite; good quality of the orthodontic finished occlusion; no fixed retention at the follow-up stage; the follow-up stage being conducted at least 3 years after the end of the active treatment; and good clinical records from pre-treatment, post-treatment, and post-retention stages, including radiographs, photographs, and dental casts. The patients should have received or not occlusal adjustment during orthodontic finishing and after the removal of the fixed appliances.
This way, the sample comprised 77 patients, who were divided into two groups according to the accomplishment or not of occlusal adjustment for orthodontic finishing. Cases that presented a discrepancy of more than 2mm from centric relation to usual maximum intercuspation were qualified to undergo occlusal adjustment. The last 40 treated patients, who met the inclusion criteria and did not undergo occlusal adjustment, served as a control group.
The patients were treated at the private clinic of the first author from 2010 to 2018. All patients underwent the same orthodontic mechanics: preadjusted fixed appliance with Roth prescription (Morelli, Sorocaba, Brazil). The archwire sequence was as follows: 0.014”and 0.016 round NiTi; 0.018” and 0.020” round stainless steel; and 0.019 x 0.025” rectangular stainless steel, followed by rectangular multi-stranded wire (braided). No interproximal reduction was performed in patients from both the groups.
2.1. Group 1: Patients Treated with Occlusal Adjustment
This group consisted of 37 patients (21 females, 16 males) with class I malocclusion who underwent non-extraction orthodontic treatment with occlusal adjustment at a mean initial age of 18.33 years (s.d.=3.96), mean post-treatment age of 20.99 years (s.d.=3.33), and mean post-retention age of 25.79 years (s.d.=3.34); the mean treatment time was 2.66 years (s.d.=1.57) and mean time for post-retention evaluation was 4.80 years (s.d.=1.10).
2.2. Group 2: Patients Treated without Occlusal Adjustment
This group comprised 40 class I malocclusion patients (19 females, 21 males) who underwent non-extraction orthodontic treatment without occlusal adjustment at a mean initial age of 18.07 years (s.d.=3.03), mean post-treatment age of 20.75 years (s.d.=3.54), and mean post-retention age of 25.89 years (s.d.=3.73). The mean treatment time and mean time of post-retention evaluation were 2.68 (s.d.=1.09) and 5.14 years (s.d.=1.36), respectively.
At the end of active orthodontic treatment, the same retention protocol was used for patients of both the groups: a removable Hawley plate in the maxillary arch and a lingual mandibular canine-to-canine bonded retainer used for 1 year on average.
Dental casts of the patients were obtained at three different time points: pre-treatment (T1), post-treatment (T2), and post-retention (T3). The occlusal adjustment procedure was performed at the finalization stage of active orthodontic treatment with rectangular intercuspation wires (multi-stranded wire, braided, Dentaurum, Ispringen, Germany), and approximately 30 days after the removal of the orthodontic fixed appliance, with the patient in centric relation (CR), according to basic occlusion criteria [8, 19].
The occlusal adjustment was performed in group 1 by the same operator using low and high-rotation handpieces, appropriate diamond burs, articulating paper miller tweezers (Bausch, Koln, Germany), and articulating paper (Art-Fol® 12μ metallic black/red, Germany) (Fig. 1A-B) to remove deflective contacts and premature contacts.



With the patient seated, whether there was a deviation between centric occlusion and maximum habitual intercuspation was observed. Once a deviation greater than 3 mm was detected between these two bites (Fig. 2), the patient was selected for occlusal adjustment. Each patient was instructed to stay reclined in the dental chair, and then the operator located the centric relationship position (CR) bimanually. Once this position was achieved, the patient was instructed to occlude the teeth to feel the first dental contact slowly. After identifying this first dental contact, the patient was to reopen the mouth. The occlusal surface of the teeth was dried, and with forceps holding the articulating paper (Art-Fol® 12μ metallic black/red, Germany) between the teeth, the patient was instructed to slowly close the mouth again, with the mandible being guided to the RC position until premature contact occurs (Fig. 3). The contact areas were located for both maxillary and mandibular posterior teeth. If a CR slide was detected (i.e., one or both contacts situated on an incline, either mesial or distal, or buccal and lingual), the inclines were reshaped into cusp tips or flat surfaces (Fig. 4) [8, 19]. According to Janson et al. [8], contacts between cusp tips and flat surfaces direct the occlusal forces through the long axes of the teeth. After eliminating the premature contacts on both the right and left sides and when the maximum posterior contact between the maxillary and mandibular posterior teeth was reached, the excursive movements of the mandible were checked. Premature contacts in the lateral and protrusive excursions were adjusted. If there was a slide during the protrusive movement, tooth wear was always done on the palatal surface of the maxillary incisors and never on the incisal edge of the mandibular incisors. The bur used to grind was an inverted-cone diamond slow-speed (#38, KG Sorensen, São Paulo, Brazil). After the procedure, the area was polished with pumice and water, and a fluoride solution was applied to the ground tooth surface for 5 minutes [8].
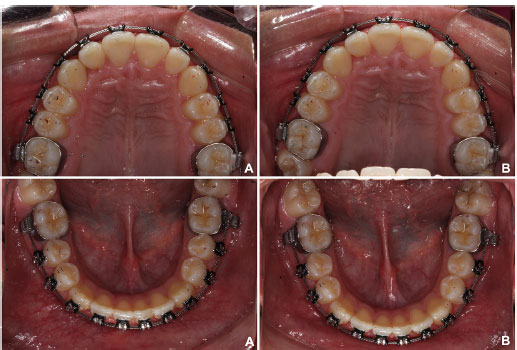
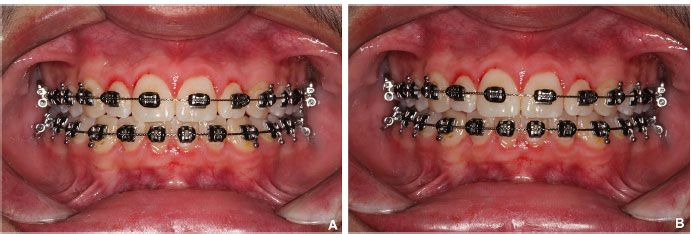
At the end of treatment, in both the groups, none of the subjects presented premature contacts or occlusal interferences during mandibular movements. All patients showed centric relation occlusion or a centric relation discrepancy to the usual maximum intercuspation of no more than 2 mm (Fig. 5).
2.3. Peer Assessment Rating (PAR) Index
The PAR index was used, as described by Richmond et al. [20], and scored with the American weight [21].
The PAR index is an occlusal index already validated to measure malocclusion, such as how much a patient deviates from the normal occlusion [20]. The index allows the evaluation of treatment outcomes, long-term stability, and relapse by comparing the severity of the initial malocclusion with the result of the post-treatment and post-retention dental casts.
The PAR index is calculated from 11 components: maxillary right and left segments, maxillary anterior segment, mandibular right and left segments, mandibular anterior segment, right and left posterior occlusion, overjet, overbite, and midline [20]. It measures teeth alignment (crowding, spacing, and impacted tooth), and sagittal, transverse, and vertical relationships (including open bite, crossbites, etc.) [22].
2.4. Little Irregularity Index
Little proposed a quantitative method to evaluate the irregularities of the mandibular anterior teeth, i.e., the linear distance of the anatomical interproximal contact of the mandibular incisors, and the sum of these five irregularities represents the distance to which the interproximal contact must be moved to achieve alignment [23].
This index was chosen to evaluate mandibular anterior crowding since it is highly reproducible and reliable, and is the most used index in the orthodontic literature to assess stability and mandibular anterior crowding relapse [18, 24].
These indexes were measured in dental casts of the initial (T1), final (T2), and post-retention (T3) stages by a single-blinded calibrated operator (MFB) with a digital caliper (ZAAS precision: 150 mm).
2.5. Error Study
The intra-examiner error was evaluated by taking new measures and calculating a new PAR index for the initial, final, and post-retention dental casts of 10 patients, with a total of 30 pairs of dental casts. The first and second measurements were performed within a month interval. The formula proposed by Dahlberg [25] was applied to estimate the random errors, and dependent t-tests were used to analyze the systematic errors.
2.6. Statistical Analysis
The normality of the data was checked with the Kolmogorov-Smirnov test, which showed normal distribution, so parametric tests were used. The chi-square test was used to evaluate the compatibility of the groups with respect to the distribution between the genders. The independent t-test was used to evaluate the compatibility of the groups regarding the initial age, the final age, the post-retention age, the time of treatment and post-retention evaluation, and initial malocclusion severity measured by PAR and Little indexes. For the inter-group comparison of the variables in the studied phases and their alterations in the treatment and post-treatment evaluation phases, the independent t-test was used. The results of all tests were analyzed with the Statistical Software for Windows, version 7.0 (StatSoft, Tulsa, Okla, USA), adopting a significance level of 5%.
3. RESULTS
There was no significant systematic error obtained; the random errors were 0.43 mm for the Little irregularity index and 0.51 for the PAR index (Table 1).
| Variables |
1st Measurement (N=30) |
2nd Measurement (N=30) |
Dahlberg | P | ||
|---|---|---|---|---|---|---|
| Mean | s.d. | Mean | S.D. | |||
| PAR (score) | 6.32 | 3.87 | 5.99 | 3.21 | 0.51 | 0.720 |
| Little (mm) | 4.95 | 3.62 | 5.07 | 3.59 | 0.43 | 0.897 |
|
Sex Group |
Males | Females | Total |
|---|---|---|---|
| Group 1 With occlusal adjustment |
16 | 21 | 37 |
| Group 2 Without occlusal adjustment |
21 | 19 | 40 |
| Total | 37 | 40 | 77 |
| X2=0.65 DF=1 P=0.416 | |||
| Variables (mm) |
Group 1 With Occlusal Adjustment (N=37) |
Group 2 Without Occlusal Adjustment (N=40) |
P | ||
|---|---|---|---|---|---|
| Mean | s.d. | Mean | s.d. | ||
| Initial age (T1) |
18.33 | 3.96 | 18.07 | 3.03 | 0.373 |
| Final age (T2) |
20.99 | 3.33 | 20.75 | 3.54 | 0.380 |
| Postretention age (T3) | 25.79 | 3.34 | 25.89 | 3.73 | 0.451 |
| Treatment time (T2-T1) |
2.66 | 1.57 | 2.68 | 1.09 | 0.474 |
| Postretention evaluation time (T3-T2) |
4.80 | 1.10 | 5.14 | 1.36 | 0.116 |
| Variables |
Group 1 With Occlusal Adjustment (N=37) |
Group 2 Without Occlusal Adjustment (N=40) |
P | ||
|---|---|---|---|---|---|
| Mean | S.D. | Mean | S.D. | ||
| PAR initial (T1) | 14.13 | 4.25 | 15.16 | 3.44 | 0.244 |
| PAR final (T2) | 1.35 | 2.65 | 1.09 | 1.89 | 0.619 |
| PAR postretention (T3) | 2.10 | 3.66 | 2.42 | 2.45 | 0.651 |
| PAR change with treatment (T2-T1) |
-12.78 | 3.22 | -14.07 | 3.13 | 0.078 |
| Postretention PAR relapse (T3-T2) |
0.75 | 1.68 | 1.33 | 1.36 | 0.099 |
| Little initial (T1) | 5.12 | 2.72 | 6.18 | 3.01 | 0.110 |
| Little final (T2) | 1.22 | 1.15 | 1.29 | 0.93 | 0.769 |
| Little postretention (T3) | 1.79 | 1.13 | 2.25 | 1.43 | 0.123 |
| Little change with treatment (T2-T1) | -3.90 | 2.91 | -4.89 | 3.33 | 0.170 |
| Postretention little relapse (T3-T2) |
0.57 | 1.35 | 0.96 | 1.26 | 0.193 |
Groups were comparable regarding gender distribution (p=0.416), initial (p=0.373), final (p=0.380) and post-retention ages (p=0.451), and treatment (p=0.474) and post-retention evaluation times (p=0.116) (Tables 2 and 3).
There was no statistically significant difference found in the intergroup comparison of PAR and Little irregularity indexes in all stages and periods evaluated (p ranging from 0.078 to 0.769) (Table 4).
Patients with malocclusions of similar type and severity treated with or without occlusal adjustment showed the same change in the post-retention period, i.e., similar post-retention occlusal and anterior alignment stability.
4. DISCUSSION
The underlying principle of occlusal adjustment is to enhance occlusal relationships, thereby improving the long-term stability of orthodontic treatments [26]. This study showed that the occlusal adjustment did not influence the alignment and occlusal post-retention stability, despite all dogma concerned with orthodontic gnathology [27]. This does not mean that this procedure should be banned or forgotten in the routine practice of the orthodontist. The orthodontist must be aware of the current concepts of long-term stability after orthodontic treatment and the factors involved in it [7, 18, 22, 28, 29]. Based on these results, occlusal adjustment is simply part of the means to achieve an ideal occlusion, like interproximal reduction for a Bolton discrepancy [26].
The sample was comparable according to the gender distribution, ages, treatment and post-retention evaluation times, and initial severity of malocclusion evaluated by the PAR and Little indexes (Tables 2-4). The homogeneity of the sample and the comparability of the groups have been considered very important in the present study because they eliminate other factors that can contribute to or influence the stability and relapse of occlusal characteristics, in addition to performing the occlusal adjustment [24, 30]. The sample was retrospectively selected from a pool of patients of the first author, and the cases that presented a discrepancy of more than 2 mm from centric relation to usual maximum intercuspation were qualified to undergo occlusal adjustment. This selection criteria were in accordance with a previous study [7]. This study revealed that most subjects one week post-debonding had a unilateral contact on initial closure in the centric occlusion and a slide between this position and the intercuspal position. The authors pointed out the long-term implications of these findings to be unclear and speculated that it could be associated with post-orthodontic instability. Since both groups of our study were comparable regarding malocclusion severity at pre-treatment and treatment results, the only difference between the two groups was the occlusal adjustment procedure that was performed in group 1. Based on this, we can assume that group 2 (no occlusal adjustment) served as a control group. At the long-term evaluation stage, both groups presented similar occlusal changes, showing that occlusal adjustment did not influence the long-term stability of orthodontic treatments.
The duration of retainer use is crucial as it directly impacts the stability of treatment results [30, 31]. This way, patients of both groups had the same retention protocol for, on average, 1 year. The time of post-treatment evaluation at the post-retention stage was approximately 5 years in both the groups. It is not a long time, but it was previously reported that most relapse occurs in the first two years after removing fixed appliances [30].
There are many ways of evaluating occlusal characteristics [20, 32], but the PAR index is validated and one of the most widely used with great acceptance [14, 18, 33]. In both groups, initial malocclusion was not so severe according to the PAR index (14.13 and 15.16) [20], and the Little irregularity index indicated moderate crowding (5.12 and 6.18mm) (Table 4) [23]. Malocclusion was similarly corrected with treatment in both groups, with an excellent orthodontic finishing (Table 4). The PAR index showed a more than 90% reduction in both groups, indicating a high standard and quality of treatment [20]. In the post-retention evaluation, the PAR index decreased to 85.13% and 84.03% in groups 1 and 2, respectively, concerning the initial malocclusion score, with a loss of less than 10%, indicating acceptable stability [12, 14, 33]. A previous long-term study that included class I and class II malocclusion showed the behavior of the PAR index over the years to be similar in both types of malocclusions [28]. Cotrin et al. showed that the PAR index improved significantly post-treatment and worsened 37 years after the treatment; however, it did not reach the pretreatment values [28]. Besides, no statistically significant difference was observed between the two groups with respect to the stability of occlusal characteristics according to the PAR index (Table 4), showing that the occlusal adjustment procedure did not influence the long-term stability of the treated cases.
The mandibular anterior crowding was similarly corrected with treatment in both groups, indicating perfect alignment or minor irregularity remaining at the end of the treatment [23]. The relapse observed increased the Little irregularity index of less than 1mm in both groups (Table 4). This is considered excellent stability for the mandibular anterior segment, which is characteristic of occlusion most prone to relapse [15, 18, 24, 29, 34-37]. There was no difference observed in the relapse of mandibular anterior crowding between patients who underwent occlusal adjustment and those who did not [15].
The number of occlusal contacts was not evaluated despite several studies determining the count of occlusal contacts as a result of adjustments or treatments [16, 38-41]. However, according to Okeson [19], in theory, an ideal occlusion implies a cusp tip contacting two opposing marginal ridges, resulting in two contacts on the cusp tip. However, the contact can occur in only one opposing ridge, resulting in a single contact in the cusp tip. Therefore, we considered a single contact per tooth acceptable after occlusal adjustment.
One can say that it is unnecessary to perform occlusal adjustment at the end of or after orthodontic treatment. But it is necessary to point out some arguments. Occlusal contacts change during and after orthodontic treatment, and settling occurs for years [28]. According to Sullivan et al. [16], orthodontic treatment may severely alter tooth contacts in the early stages of treatment. It may lead to an appreciable permanent reduction in occlusal contacts, which is not always compensated by a prolonged period of post-treatment settling. In addition, these authors also recommend close attention to finishing and occlusal adjustment to ensure more contact. It is common to observe a slide from the centric occlusion to the maximum intercuspation occlusion after treatment. Therefore, centric relation may not accurately record day-to-day contacts with a discrepancy between centric relation and usual maximum intercuspation. So, the cases that presented a discrepancy of more than 2 mm from centric relation to centric occlusion at the end of orthodontic treatment were qualified for occlusal adjustment. According to Ziebert et al. [38], the type of tooth contacts that are the most stable are those of a cusp against a flat plane (e.g., the bottom of a fossa or marginal ridge) or those of a combination of a cusp against a flat plane and one or more inclined planes. So, it could be speculated that even in those patients who did not undergo occlusal adjustment, these types of occlusal relationships were present, highlighting the same occlusal relapse in the long term for both groups. In a study evaluating the incidence of occlusal contact points, Rinchuse and Sassouni [27] found that the functional bite registrations generated in centric occlusion did not show significant differences in the number, location, or severity of non-working (balancing) or protrusive functional occlusion contacts between orthodontically treated and untreated subjects with ideal static occlusion. Besides, Gazit and Lieberman [39] found that the number of occlusal contacts increased by 56% in the first year following orthodontic treatment. This indicates that orthodontic treatment in the long-term can maintain good occlusal contacts without interference and premature contacts, and that there is not always a need for occlusal adjustment; however, performing it may not add significant advantages, mainly in terms of stability, as results of the present study showed. However, the present study did not evaluate the number of occlusal contacts after treatment since this was retrospective. Selective tooth wear should not be used as a substitute for an orthodontic movement in patients with not well-finished occlusions nor as a solution to the limitations of the orthodontist [5].
A balanced occlusion obtained after orthodontic treatment may not necessarily need an occlusal adjustment. Orthodontists must seek occlusal balance since unbalanced occlusal contacts generate undesirable forces, and consequently undesirable tooth movements, depending on the intensity and duration of the contact, and not as a factor determining dental stability, as indicated by the present study’s results. However, we must remember that the current study evaluated only patients without any sign or symptom of TMD and at the end of orthodontic treatment. In addition, none of the patients presented premature contacts or occlusal interferences during mandibular movements, and all of them were finished in centric relation occlusion or a centric relation discrepancy to the usual maximum intercuspation no more than 2mm.
One could say that the occlusal adjustment could bring some risk to the patient, such as dentin sensitivity, due to excessive enamel wear. Enamel thickness patterns are partly explained as an adaptation to functional demand [42]. The lingual faces of maxillary molars and the buccal faces of the mandibular ones have thicker enamel than the other crown faces [42]. According to Moncada et al., there is no correlation between tooth sensitivities and tooth thickness [43]. Janson et al. [8] evaluated the treatment of anterior open bite performed with occlusal adjustment and stated that it is a viable treatment alternative for this malocclusion, which improves the functional occlusion with only transient sensitivity. Besides that, they evaluated the same sample 3.4 years after the procedure, and the dentinal sensitivity remained within the normal range in the long term [9].
CONCLUSION
In the present study, there was no significant difference obtained in the post-retention crowding and occlusal relapse between class I patients treated with orthodontic non-extraction with and without occlusal adjustment. Also, the occlusal adjustment did not influence the post-retention alignment and occlusal stability.
LIST OF ABBREVIATIONS
| TMD | = Temporomandibular joint dysfunction |
| CR | = Centric relation |
| PAR | = Peer assessment rating |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Ethics Research Committee of Ingá University Center, with number 1.957.938.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee, and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
ACKNOWLEDGEMENTS
Declared none.


