All published articles of this journal are available on ScienceDirect.
Clinical Evaluation of Reasons for Immediate Composite Restoration Failure Placed by Dental Students: A Cross-sectional Study in Jordan
Abstract
Objective:
The present study aims to investigate the reasons for the immediate failure of direct anterior and posterior resin composite restorations placed by dental students.
Methods:
A cross-sectional study on resin composite restorations placed by fourth- and fifth-year dental students (n=436). Variables included in the study were; the operative field isolation method, the time needed to complete the restoration after cavity preparation to polishing and finishing, and the plaque index of the patient. Restoration class distribution according to the type of tooth and cavity classification was examined and recorded. Restorations were clinically evaluated immediately after placement. It involved the assessment of the restoration’s mobility, marginal discoloration, and lack of anatomy.
Results:
A total of 233 direct anterior and posterior resin composite restorations which were placed by 127 students were diagnosed as failed restorations. The mode of failure was distributed as mobility/debonding (61.80%), marginal discoloration (29.18%), and lack of anatomy (9.02%). Cl III restorations demonstrated the highest failure on tooth type and cavity classification (30%), followed by Cl II restorations in molars (18.45%). Failure-associated factors were proper restoration manipulation, field isolation, and patients’ plaque index.
Conclusion:
In the current study, the most frequent reason for the immediate failure of resin composite restorations was the quick application of the restoration either as the only associated factor or coupled with other failure-associated factors. Failure to maintain proper field isolation and the poor oral hygiene of the patient were the other two failure-associated factors.
1. INTRODUCTION
For centuries dental amalgam was considered the material of choice for restoring carious cavities in posterior teeth [1]. However, Buonocore's improvement of adhesive dental materials since 1955 has led to a giant leap in restorative dentistry [2]. Thus, minimal invasive philosophy was adopted in dentistry in the early 1970s [3]. Thus, dental amalgam restoration lost its glory and popularity in favor of more aesthetic and conservative resin composite restoration [4]. Nevertheless, this new material has disadvantages including; greater technique sensitivity, time consumption during placement, polymerization shrinkage with less wear resistance, and higher cost than dental amalgam [5, 6].
On the other hand, when placed correctly, posterior resin composite restorations may be as serviceable as amalgams, with the privilege of being more esthetic and more conservative and reinforcing the remaining tooth structure through adhesive properties [1]. Accordingly, patients, dental students, and dental curricula in dental education shifted toward tooth-colored dental materials for both anterior and posterior dentitions [7].
Dental amalgam and composites are taught as restorative materials in the undergraduate curriculum at the School of Dentistry, Jordan University. BDS is a 5-year program followed by a one-year internship wherein students learn about the restoration of teeth from their 3rd academic year, where they start practicing manual skills on simulation units. In the 4th and 5th academic years, they move to the clinical courses where they treat patients under supervision. Even though our dental curriculum emphasizes teaching both amalgam and composite in pre-clinical and clinics which means that our students’ clinical training and knowledge about both restorative materials are the same, students and patients prefer to utilize tooth-colored restorative materials for restoring teeth.
However, as aforementioned, resin composites are technique-sensitive materials and adequate operating field isolation is critical for the success and longevity of the restorations [8]. Moreover, the patient’s oral hygiene is an important determining factor associated with the success and longevity of such restorations anteriorly and posteriorly [9]. Students feel more comfortable when handling composites in terms of cavity preparation and material manipulation. Albeit their enthusiasm, immediate failure of those direct composite restorations is not uncommon among undergraduate dental students.
The current study aimed to evaluate clinically the reasons for immediate direct composite restoration failure placed by undergraduate dental students among the patients presenting at students’ dental clinics of the School of Dentistry at Jordan University Hospital for dental caries treatment.
2. MATERIALS AND METHODS
According to the ethics policy of the University of Jordan, the ethical approval form and permission to collect the needed data were signed and approved by the Faculty of Dentistry Research and Ethics Committee (FDREC) and the Academic Research Committee (ARC) at the University of Jordan (No. 75/2022/870).
This cross-sectional study was carried out on 436 4th and 5th-year students (343 female and 93 male) practicing in their restorative dentistry sessions in the dental clinics of the School of Dentistry of Jordan University Hospital (for the academic year 2021-2022). Inclusion criteria for the study include; anterior and posterior direct composite restorations for permanent anterior and posterior teeth. Exclusion criteria include; amalgam and glass ionomer restorations, old composite resin restorations to be replaced or repaired, and endodontic-treated teeth that need restoration. The demographic information like the gender of the student and his or her academic year were recorded. Restoration class (according to GV Black classification) distribution according to the type of tooth (anterior, premolar, or molar) and cavity classification (Cl I, Cl II, Cl III, Cl IV, Cl V) was examined and recorded on a case sheet form specially designed for this study. The authors noted several student and patient characteristics to investigate their relationship with failure further. These characteristics included the operative field isolation method utilized by the student (rubber dam or cotton rolls, with suction), the time needed to complete the restoration after cavity preparation to polishing and finishing (˂ half an hour, half an hour to one hour, ˃ one hour), and the plaque index of the patient (good, fair, poor).
Oral hygiene was evaluated by examining the dental plaque present on the inner and outer aspects of the six index teeth (upper right first molar, upper right lateral incisor, upper left first premolar, the lower right first premolar, the lower left lateral incisor and first molar), using the criteria of the plaque index of Silness and Löe [ 10 ]. Evaluating the state of the patient’s oral hygiene during the examination was as follows: good (plaque index 0.0 absence of plaque), fair (plaque index 0.1–1.9 presence of plaque), poor (plaque index 2.0–3.0 plaque seen by the naked eye).
All restorations were placed by dental students under the supervision of a staff member according to a fixed yet flexible protocol. The protocol theoretically included the following steps in sequence: local anesthesia (when needed) and rubber dam isolation (if applicable); cavity preparation following a conservative design; sectional matrix (posteriorly) or cellulose strip (anteriorly) and a wooden wedge application; acid etching with 37% phosphoric acid for fifteen seconds, rinsing and drying while leaving the dentin moist; application of dentin bonding agent and light curing for twenty seconds; incrementally restoring the cavity with resin composite and light curing each increment for forty seconds; finishing and polishing of the restoration; finally, checking the occlusion and proximal contacts (Ventura Nanolux kit, Madespa, Spain).
Restorations were examined immediately by the supervisor (staff member from the restorative dentistry department). The clinical evaluation was performed on a dental chair under dental operating light using a front-surfaced mouth mirror and dental explorer. Immediate examination of the restoration involved the assessment of the restoration’s mobility, marginal discoloration, or lack of anatomy.
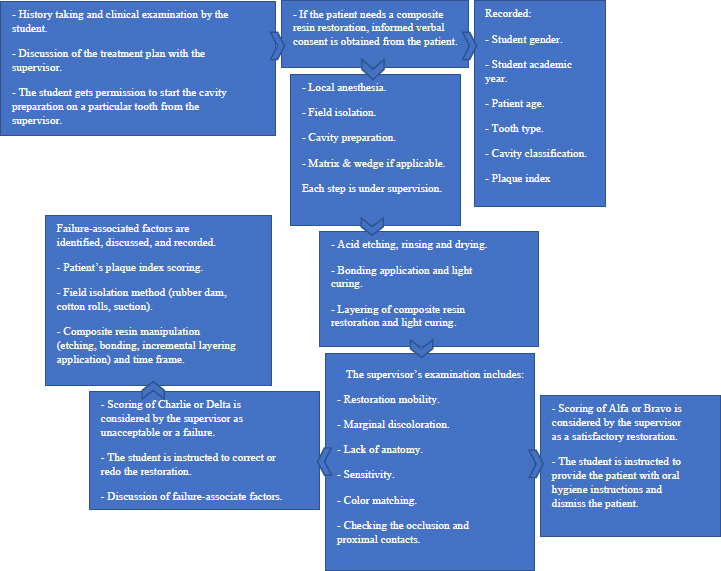
According to The United States Public Health Service (USPHS) criteria: Alfa: restorations of satisfactory quality and meeting all clinical standards with a range of excellence; Bravo: satisfactory restorations though not ideal, with a range of acceptability; Charlie: restorations of unacceptable quality having to be replaced or corrected for preventive reasons; Delta score: was assigned when the restoration was found to be mobile, fractured or missing. Restorations with a Charlie or Delta evaluation were considered failures and the associated factor/s for the failure was/were documented. Furthermore, the supervisor instructs the student to replace the failed restoration and redo it after identifying the failure-associated factors and discussing them with the student. The experimental design is demonstrated in Fig. (1).
The collected information and responses were coded and statistical analysis was performed using the software SPSS Statistics for Windows, Version 16.0 (SPSS Inc., Chicago, IL, USA). All data were tested for normality using the Shapiro-Wilk test. Descriptive statistics was generated and the Chi-square test was used to examine associations between the different variables. The significance level was set at P < 0.05.
3. RESULTS
The total sample comprised 233 failed restorations done by 127 students (68 female students and 59 male students). The sample distribution according to patients’ age group is shown in Table 1, in which the majority of the sample population fell in the age group 30-50 years old. The distribution of failed restorations on tooth type and cavity classification was demonstrated in Table 2. 52.36% of the failed restorations are located in anterior teeth. 56.56% and 28.69% of anterior failed restorations are of Cl III and Cl V, respectively. The mode of failure is shown in Table 3, and failure-associated factors are demonstrated in Table 4. The distribution of failed restorations in students’ academic year is shown in Table 5. The most frequent reason for failure was due to the quick application of the restoration representing 76.4% of the failed restorations either as the only associated factor or coupled with other failure-associated factors, followed by failure to maintain field isolation (66.1%) either alone or associated with the other two failure associated factors. Poor oral hygiene represented 40% of all failed restorations. Poor oral hygiene was the only failure-associated factor in 48.4% of those failed restorations, while 51.6% of the failed restorations were associated with poor oral hygiene and other failure-associated factors. Among the failed restorations, mobile restorations represented 61.8%, while marginal discoloration represented 28.8% of the failed restorations.
| Patients’ Age | 16-30 | 31-50 | 51-70 |
|---|---|---|---|
| N=112 | 22 | 71 | 19 |
Table 2.
| N=233 | Cl I | Cl II | Cl III | Cl IV | Cl V |
|---|---|---|---|---|---|
| Anterior | - | - | 69 | 18 | 35 |
| Premolar | 2 | 30 | - | - | - |
| Molar | 22 | 43 | - | - | 14 |
Mobile restorations were evident in class III restorations (36.1%), while marginal discoloration and lack of anatomy were the highest in class II restorations (38.8%) and (50%), respectively, as shown in Table 6. The Chi-square tests results and the independent samples t-test demonstrated a statistically significant relationship between mobile restoration (debonding) and failure-associated factors (P < 0.001) as shown in Tables 7 and 8.
| Mode of Failure | Mobile Restoration | Marginal Discoloration | Lack of Anatomy |
|---|---|---|---|
| N=233 | n=144 (61.80%) | n=68 (29.18%) |
n=21 (9.02%) |
| Cl I premolars | - | - | 2 |
| Cl I molars | 5 | 14 | 3 |
| Cl II premolars | 21 | 7 | 2 |
| Cl II molars | 17 | 19 | 7 |
| Cl III anterior | 52 | 14 | 3 |
| Cl IV anterior | 11 | 5 | 2 |
| Cl V anterior | 29 | 5 | 1 |
| Cl V molars | 9 | 4 | 1 |
| N=233 | Mobile Restoration n=144 (%) |
Marginal Discoloration n=68 (%) |
Lack of Anatomy n=21 (%) |
|---|---|---|---|
| Field isolation/rubber dam + suction | n=48 33.33% |
n=26 38.24% |
n=4 33.33% |
| Field isolation/cotton rolls + suction | n=96 66.67% |
n=42 61.76% |
n=8 66.67% |
| Time to restore tooth/ < half an hour | n=89 61.81% |
n=34 50.00% |
n=5 41.67% |
| Time to restore tooth/ ½ - 1 hour | n=36 25.00% |
n=25 36.76% |
n=4 33.33% |
| Time to restore tooth/ > 1 hour | n=19 13.19% |
n=9 13.24% |
n=3 25.00% |
| Patient’s plaque index good |
n=48 33.33% |
n=14 20.59% |
n=4 33.33% |
| Patient’s plaque index Fair |
n=67 46.53% |
n=25 36.76% |
n=6 50.00% |
| Patient’s plaque index Poor |
n=29 20.14% |
n=29 42.65% |
n=2 16.67% |
| Student’s Academic Year | N=127 | % |
|---|---|---|
| 4th-year student | n=92 | 72.44% |
| 5th-year student | n=35 | 27.56% |
| - | Cavity Classification | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| Class 1 | Class 2 | Class 3 | Class 4 | Class 5 | - | |||
| Mode of Failure | Mobile restoration | Count | 5 | 38 | 52 | 11 | 38 | 144 |
| % within modeoffailure | 3.5% | 26.4% | 36.1% | 7.6% | 26.4% | 100.0% | ||
| % within cavityclassification | 20.8% | 52.1% | 75.4% | 61.1% | 77.6% | 61.8% | ||
| Marginal discoloration | Count | 16 | 26 | 12 | 5 | 8 | 67 | |
| % Within modeoffailure | 23.9% | 38.8% | 17.9% | 7.5% | 11.9% | 100.0% | ||
| % within cavityclassification | 66.7% | 35.6% | 17.4% | 27.8% | 16.3% | 28.8% | ||
| Lack of anatomy | Count | 1 | 6 | 3 | 1 | 1 | 12 | |
| % within modeoffailure | 8.3% | 50.0% | 25.0% | 8.3% | 8.3% | 100.0% | ||
| % within cavityclassification | 4.2% | 8.2% | 4.3% | 5.6% | 2.0% | 5.2% | ||
| Total | Count | 24 | 73 | 69 | 18 | 49 | 233 | |
| % within modeoffailure | 10.3% | 31.3% | 29.6% | 7.7% | 21.0% | 100.0% | ||
| % within cavityclassification | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | ||
| - | Value | df | Asymptotic Significance (2-sided) |
|---|---|---|---|
| Pearson Chi-Square | 34.284a | 12 | .001 |
| Likelihood Ratio | 33.887 | 12 | .001 |
| Linear-by-Linear Association | 11.496 | 1 | .001 |
| N of Valid Cases | 233 | - | - |
| a. 10 cells (50.0%) have an expected count of less than 5. The minimum expected count is 0.77. | |||
| - | Levene's Test for Equality of Variances | t-test for Equality of Means | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| F | Sig. | t | df | Sig. (2-tailed) | Mean Difference | Std. Error Difference | 95% Confidence Interval of the Difference | |||
| Lower | Upper | |||||||||
| Mode of failure |
Equal variances assumed | .007 | .933 | -.503 | 231 | .615 | -.070 | .139 | -.343 | .203 |
| Equal variances not assumed | - | - | -.519 | 60.328 | .605 | -.070 | .134 | -.338 | .199 | |
4. DISCUSSION
Typically, dental students are required to treat patients’ anterior and posterior carious teeth with restorations during their undergraduate training. Dental schools are responsible for providing undergraduates with adequate, efficient training to ensure the graduation of knowledgeable clinicians equipped sufficiently to practice dentistry independently [11]. Since the late 90s, there is a general trend in dental schools toward adopting composites for both anterior and posterior restorations instead of restoring posterior cavities with amalgam fillings [12]. However, dental students need to possess a clear understanding and knowledge of the standards and the criteria of successful composite fillings to enhance the longevity and quality of their restorations [13]. These guidelines will augment their abilities, given that they lack practical experience and have not yet acquired adequate competent manual skills necessary to assemble a successful restoration [11, 12].
The purpose of the present study was to evaluate clinically the reasons for immediate direct composite restorations failure placed by undergraduate dental students among the patients presenting at students’ dental clinics of the dental school at Jordan University Hospital for dental caries treatment.
It is acknowledged worldwide that esthetic dentistry is receiving increased attention in dental practice, and esthetic concepts and techniques are taught in almost all dental schools [14]. However, the performance of dental restorations is influenced by several factors other than the clinician itself, such as the restorative material’s properties and other patient’s associated factors [15, 16]. The failure of resin composite restorations in particular in the anterior teeth in our study, can be attributed to these several factors collectively.
First, applying composite restorations is a multi-step procedure that requires proper knowledge of the importance of the precise application of each step to avoid the cumulative effect of errors in each step [13, 17]. In this study, the improper manipulation of the restoration (acid etching timing on enamel and dentin, proper washing, drying approach to both enamel and dentin) and the inappropriate placement technique (beveling, incremental layering, light curing) was the most frequent reason for restoration failure, which is attributed possibly to students’ lack of experience, skills, and comprehensive knowledge [18, 19]. This fundamental factor was associated with restoration failure placed by other undergraduates in several dental schools and studies [20-22]. Furthermore, the results of our study, which demonstrated decreased failure rate among fifth-year students in comparison to fourth-year students and decreased failure rate among the second semester in comparison to the first semester for both fourth and fifth-year students are supported by other results that stated the significance of incremental learning [23, 24], in which technical dental procedures are trainable in the course of dental education and that motor skills are teachable and can be acquired during the course of learning to accomplish a successful clinically acceptable composite restoration [23-25].
The authors noticed in the current study that the quality of the restoration placed by the students is related to the time frame. Resin composites are technique-sensitive materials, which means handling them as restorative materials mandate specific requirements [18, 19, 21]. The more time spent by students applying the restoration starting after cavity preparation and ending with polishing and finishing, the less debonding, or/and marginal discoloration of the restoration was identified. In our study, debonding and failure of adhesion was the main cause of failure among other modes of failure for composite restorations (61.80%). This result is in agreement with Reis de Moura et al. study, which might be due to the lack of experience of undergraduates with adhesive technique, although the same aforementioned study demonstrated higher failure rates with Cl II and Cl IV than Cl III restorations in contrast to our results where Cl III (36.1%) restorations showed highest failure percentage among cavity classification [12]. In another study, posterior restorations showed more fractures and loss than anterior restorations, although the annual survival rate for anterior restorations was lower than for posterior ones [26]. Comparing the results is improper since the nature of the two studies is different, in which our study is an immediate clinical evaluation of posterior and anterior composite restorations placed by dental students, while the other study is based on a retrospective longitudinal evaluation of such restorations.
The results of the current study coincide with other findings regarding the influence of proper handling of composite resin restoration on its success [ 27 ]. Another study by Mjor and Toffenetti [ 28 ] reported that inadequate handling of the material can be a reason for marginal discoloration.
Second, one of the essential elements of proper bonding of composite resin restoration to tooth structure is appropriate field isolation and complete avoidance of moisture contamination [17, 18]. The importance of such a factor can’t be underestimated and it was the main reason for failed restorations (Cl II, Cl III, and Cl V) in our study, especially among fourth-year students. Restoration’s mobility (66.67%) and marginal discoloration (61.76%) were highly evident in such failures (95.83%) and highly associated with failure to maintain optimal field isolation. Worth mentioning that the more training the students undertake to apply the rubber dam to achieve optimal isolation effectively, the less moisture contamination and eventually less failure of restoration they have. In other words, it is highly recommended that students appreciate the effect of the proper application of rubber dam to achieve effective isolation rather than the utility of rubber dam per se.
The third factor that can’t be neglected and play a pivotal role here is case selection [29]. One of the major contributing factors to case selection is the patient’s oral hygiene status [19, 29]. Patient oral hygiene is a very important factor in determining the longevity of resin composite restorations [16]. Composite accelerates the growth of Streptococcus mutans, which in combination with poor oral hygiene, will cause marginal discoloration and secondary caries [30].
The low failure rates associated with poor oral hygiene demonstrated in our study are due to the decreased number of cases with poor oral hygiene. Failed restorations in patients with good and fair plaque index were associated with inappropriate placement of restoration and improper field isolation rather than plaque index. On the other hand, half of the poor plaque index cases failed due to this factor alone. Poor oral hygiene is associated with inflammatory response and gingival bleeding [ 31 ], which jeopardizes the etching step and compromises the subsequent bonding due to moisture contamination with blood [ 32 ], which will eventually lead to debonding and restoration failure.
As is visible from the results, failure modes and factors are intermingled and can’t be separated or segregated. Remarkably, students who tend to fail a restoration have more tendency to fail more restorations and vice versa. This tendency can be attributed to individual variations among the students regarding their manual dexterity and competency [24]. Despite the importance of such factor, which could affect the results, the current study didn’t investigate the correlation of this variable. Furthermore, the ability of students to provide their patients with better resin composite restorations increased as the level of education increased, and this could be explained by the impact of clinical practice and increased knowledge and understanding on refining their capabilities and manual skills [25].
Besides, the teaching method among undergraduate dental students may be crucial in yielding better outcomes regarding composite resin restoration procedures and other dental skills [13,21,33]. The step-by-step strategy proved to facilitate a more efficient teaching process, close and positive interaction between students and teachers; and results in less cumulative effect of errors in each step than the all-in-one teaching method [13,33]. Furthermore, dental schools are reported to be highly demanding and stressful learning environments. Recent studies have shown that studying dentistry can be extremely stressful for clinical-years students who need to acquire diverse proficiencies such as theoretical knowledge, clinical skills, and interpersonal communication skillsleading to diminished efficiency at learning [34]. Students tend to focus on finishing the required procedure on time to gain the mark, rather than on the quality of the procedure itself. This is observed clearly when the student finishes a multi-surface restoration in less time than the supervisor can finish it. Although each step is approved by the supervisor, proper measures throughout the whole procedure cannot be guaranteed from the student side, such as avoidance of moisture contamination, sufficient etching time, proper bonding and curing, and incremental layering application of the restoration. However, similar studies with larger sample sizes, more successive academic years inclusion, more variables, and a larger range of dental skills are required to generalize the results.
To the best of the authors’ knowledge, no studies to date have assessed the ability of dental students to handle dental composites adequately and analyzed failure-associated factors linked with immediate failures.
5. LIMITATIONS OF THE STUDY
The results of this study can’t be generalized or conclusive due to Covid-19 pandemic conditions, increased numbers of students at our school of dentistry, and the short duration of the study, which was one year. More clinical training in restorative dentistry can be provided during the fourth and fifth academic years, which will reduce restorative failure among undergraduate students, and this factor (training sessions) is variable.
Moreover, as the study is not a retrospective study nor a long-term clinical study and it was intentionally aiming to study the immediate failure modes associated factors, only three modes of failures were studied (restoration’s mobility, marginal discoloration, and lack of anatomy). Thus, recurrent caries and restoration fractures were invalid modes of failure.
Color mismatching was also intentionally not evaluated in the current study due to the limitation of shade selection. In addition, neither the quality nor the quantity of the etchant, the bonding agent, and the composite resin material were included in the failure-associated factors assessment evaluation process.
Finally, the authors didn’t count the total number of the restored teeth, though it would have been much better if the percentage of the failed restorations could be calculated, due to the huge number of students and restorations, only the failed restorations were included in the study.
CONCLUSION
In the current study, the most frequent reason for the immediate failure of resin composite restorations was the quick application of the restoration either as the only associated factor or coupled with other failure-associated factors. Failure to maintain proper field isolation and the patient's poor oral hygiene were the other two failure-associated factors. The results of this study indicate the importance of integrally teaching dental students theoretically and practically the success-associated factors of adhesive restorative materials and their technique sensitivity.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
According to the ethics policy of the University of Jordan, the ethical approval form and permission to collect the needed data were signed and approved by the Faculty of Dentistry Research and Ethics Committee (FDREC) and the Academic Research Committee (ARC) at the University of Jordan (No. 75/2022/870).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from the participants prior to participation.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The datasets used and/or analyzed during the current study are available from the corresponding author [A.A.A] upon reasonable request.
FUNDING
None.
CONFLICT OF INTEREST
The authors have no conflict of interest to declare.
ACKNOWLEDGEMENTS
Declared none.


