All published articles of this journal are available on ScienceDirect.
Prevalence of Peri-implant Diseases in Patients Attending a Colombian University Dental Clinic: A Retrospective Study
Abstract
Introduction:
Due to the growing demand for dental implants to treat edentulism, the presence of peri-implant diseases (PD) is also increasing. Estimates of the prevalence of PD in the world continue to be heterogeneous. According to the new classification of periodontal and peri-implant diseases in the Colombian population, its frequency was unknown.
Objective:
To evaluate the prevalence of PD in patient assistants in a dental clinic of a Colombian university in Bogotá between 2015-2020.
Methodology:
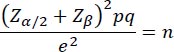
Cross-sectional observational study based on dental records. From a sample frame of 370 dental records of patients treated with dental implants, a sample size of 156 was established and chosen randomly. An analysis was performed through descriptive and inferential statistics. Statistical significance was considered p < 0.05. The open statistical package R was used.
Results:
The final sample was 216 implants. The prevalence of peri-implant health was 50.93%, peri-implant mucositis 31.48%, and peri-implantitis 17.59%. There was a significant relationship between elevated Silness and Löe index and female gender with the development of PD ( p=0.000). Systemic conditions other than diabetes, implant placement time, simultaneous regeneration, surgical and post-surgical complications, placement site, and adherence to maintenance therapies did not have statistical significance.
Conclusion:
The prevalence of PD was 49.07% in these implants. This indicates the need for a follow-up program and supportive peri-implant therapy.
1. INTRODUCTION
According to the National Study of Oral Health IV in 2014 (ENSAB IV) in Colombia, the prevalence of partial edentulism in patients older than 20 years was 19.7%. 50% of people over 65 have lost more than eight teeth, and 32.9% are edentulous [ 1]. There are different therapeutic options for replacing teeth, such as removable or fixed prostheses and dental implants. Implant therapy has advanced considerably in recent decades, becoming a widely expanded alternative in dental practice, with a predictability of over 95% in 10 years of follow-up [ 2]. Although dental implants provide a solution for the rehabilitation of edentulous ridges, inflammatory peri-implant diseases around them have been reported, which can compromise their stability and permanence in the oral cavity [ 3 ].
These conditions were first described in 1993 at the First European Workshop on Periodontics, had numerous case definitions, and different clinical parameters were considered for their diagnosis. Hence, the prevalence was diverse, given the lack of consensus regarding the signs of health or disease in dental implants [ 4]. For example, considering different ranges of bone loss, a wide prevalence of peri-implantitis has been reported from 1%, with a bone loss more significant than 5 mm as a reference. In comparison, other studies considered that bone loss of 0.4 mm increased its prevalence by 47% [ 5]. Sanz et al. (2012) considered other variables, such as those implants with initial radiographs where periimplantitis was defined as a marginal bone loss between 1- and 1.5-mm. Cases without initial radiography were marginal bone loss of 2 mm after the initial remodeling phase counted as a definition of periimplantitis [ 6]. In other cases, it was impossible to determine a statistically significant relationship between the prevalence of periimplantitis in implants placed in native bone vs. regenerated sites in a 10-year follow-up [ 7]. The difference in concepts for a case definition varied substantially. For example, Rocuzzo et al. (2014) defined peri-implantitis as a bone loss greater or equal to 2 mm [ 8]. While Tenenbaum et al. (2017) define peri-implantitis as bone loss greater than or equal to 4.5 mm [ 9].
Therefore, global epidemiological reports showed a significant variation in the prevalence of peri-implant diseases according to the population and the established case definitions. Therefore, comparisons between studies proved to be challenging [ 10]. A consensus was made by the American Society of Periodontology and the European Federation of Periodontology, published in 2018, where the signs of each peri-implant condition were defined. According to this publication, peri-implant conditions can be diagnosed as health, peri-implant mucositis, and periimplantitis [ 11]. Peri-implant health is defined as the absence of clinical signs of inflammation and bleeding, accompanied by bone loss that does not exceed 2 mm concerning the initial position of the implant [ 11]. Peri-implant mucositis is characterized by inflammation of the peri-implant mucosa and bleeding without bone loss [ 12]. Periimplantitis presents inflammation of the peri-implant mucosa, bleeding, and progressive bone loss, with possible suppuration [ 11].
Implantology therapy has been used in dentistry as an alternative to restore function and aesthetics to partially or totally edentulous patients. However, dental implants are not exempt from biological complications or diseases [ 11]. These inflammatory diseases have generated significant interest today due to their limitations in treatment. Although with the new classification criteria, the cases have been redefined, reporting a reduction in the prevalence of periimplantitis to the previous criteria, the figures continue to be inconclusive. In a 10-year follow-up with 220 implants, it was reported that 35.3% of implants had a diagnosis of mucositis and 8.7% of implants with a diagnosis of peri-implantitis [ 13].
No prevalence studies have been published in Colombia based on the 2018 classification of peri-implant conditions. Studies such as the one by Duque et al. (2016), with a case definition of probing depths greater than or equal to 5 mm, with bleeding and bone loss greater than or equal to 2 mm, reported a prevalence of 81.2% of mucositis and 15.6% of peri-implantitis [ 14]. However, as already mentioned, the limitations lie in the diversity of concepts for a peri-implant diagnosis.
Due to the above, it is worth conducting a study based on the new classification of periodontal and peri-implant diseases of 2018 [ 11] that allows knowing national figures with defined and unified criteria defining preventive or therapeutic measures. The objective of the present study was to evaluate the prevalence of peri-implant diseases in patients at the dental clinic of UNICOC Bogotá between 2015-2020.
2. METHODOLOGY
A cross-sectional retrospective study was conducted with clinical records of patients over 18 who received dental implants and a definitive crown between 2015 and 2020. According to the American Association of Periodontology and the European Federation of Periodontology [ 11], the classification criteria were used to determine the cases of peri-implant health, peri-implant mucositis, and periimplantitis. From a total population of 370 medical records of patients treated with dental implants at the UNICOC School of Dentistry, a sample size of 156 was established and randomly chosen using the Microsoft Excel program. The sample size was established using the following:
 |
Within the inclusion criteria, clinical records of patients over 18 who attended the UNICOC postgraduate clinic between 2015-2020 with implant therapy and who have received rehabilitation on these implants were evaluated. Dental records that did not present a periapical radiographic record or presented a prosthetic load were excluded. The data were taken from the dental records, and a periapical radiographic analysis was performed in a 1:1 ratio. Bone loss from the implant platform to the apical portion of the implant was considered for bone loss records. All the records were accounted for to determine the diagnosis according to the 2018 classification: clinical analysis records such as probing depth, bleeding, suppuration, and radiographic analysis. According to article 11 of Resolution 008430 of 1993 in Colombia, it is considered an investigation without risk. No biological, physiological, psychological, or social intervention was performed on the subjects involved. The institutional ethics committee of Institución Universitaria Colegios de Colombia (UNICOC) evaluated and approved the study with approval number 23-04-2021-06. Written informed consent has been taken from the patients for this study.
The data was recorded in a database in the Microsoft Excel program. The kappa index was calculated with ten dental records reviewed by the three examiners and the expert researcher, obtaining a kappa index of 0.89.
The data obtained were analyzed using the chi-square test (χ 2), the Microsoft Excel program, and R software, and a statistical significance value of p < 0.05.
3. RESULTS
A total of 156 medical records from the UNICOC Bogotá School of Dentistry were reviewed. Of these, 19 medical records were excluded because they did not meet the inclusion criteria (19 without implant rehabilitation). In the 137 histories evaluated, a total of 369 implants were found. The socio-demographic profile is defined in Table 1.
Of the total number of implants registered in the dental records (369), there was no peri-implant chart for re-evaluating 153 implants (41.46%), so it was impossible to reach a diagnosis. Therefore, a sample of 216 implants was taken for the present study.
The peri-implant diagnosis was distributed as follows: Peri-implant health 110 implants (50.93%), peri-implant mucositis 68 implants (31.48%), and peri-implantitis 38 implants (17.59%) (Fig. 1).
After the statistical analysis (chi-square), the results are summarized in Table 2.
Regarding the gender variable, we found that, of the 216 implants, 143 were found in women and 73 in men. The sex difference was statistically significant for health, mucositis, and periimplantitis ( p =0.000). However, it is noteworthy that the number of implants found in women was more significant than in men (Table 2).
| Sociodemographic Profile | |||
|---|---|---|---|
| Variable | n | Percentage (%) | |
| Sex | Female | 93 | 67.88 |
| Male | 44 | 32.12 | |
| Age | 20-34 | 4 | 2.92 |
| 35-44 | 10 | 7.30 | |
| 45-64 | 84 | 61.31 | |
| 65-79 | 39 | 28.47 | |
| Social stratum | Stratum 1 | 1 | 0.73 |
| Stratum 2 | 9 | 6.57 | |
| Stratum 3 | 16 | 11.68 | |
| Stratum 4 | 3 | 2.19 | |
| Stratum 5 | 1 | 0.73 | |
| Stratum 6 | 0 | 0.00 | |
| Not registered | 107 | 78.10 | |
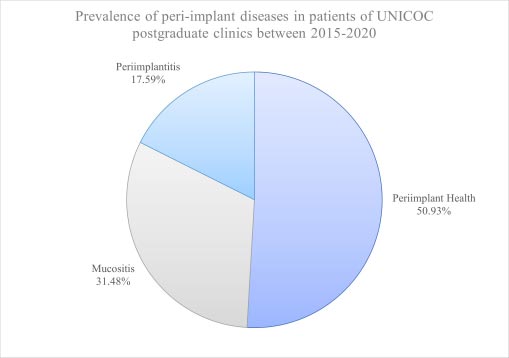
Table 2.
| Variable | Peri-implant health (n) | Mucositis (n) | Periimplantitis (n) | Total (n) | p-value | |
|---|---|---|---|---|---|---|
| Sex | Female | 76* | 36* | 31* | 143 | 0.000 |
| Male | 34 | 32 | 7 | 73 | >0.05 | |
| Age | 20-34 | 0 | 2 | 0 | 2 | >0.05 |
| 35-44 | 7 | 1 | 0 | 8 | >0.05 | |
| 45-64 | 64* | 30 | 22* | 116 | 0.042 | |
| 65-79 | 39 | 35* | 16 | 90 | 0.042 | |
| Systemic disease | Present | 58 | 38 | 19 | 115 | 0.834 |
| Not present | 52 | 30 | 19 | 101 | 0.834 | |
| Diabetes | Present | 5 | 11* | 3 | 19 | 0.028 |
| Not present | 105 | 57 | 35 | 197 | >0.05 | |
| Silness y Löe index | 0-15% | 10 | 3 | 0 | 13 | >0.05 |
| 16-30% | 28* | 26* | 13* | 67 | 0.009 | |
| 31-100% | 12 | 15 | 14* | 41 | 0.009 | |
| Implant placement time | Immediate | 2 | 0 | 0 | 2 | 0.645 |
| Early | 1 | 1 | 1 | 3 | 0.645 | |
| Late | 107 | 64 | 36 | 207 | 0.645 | |
| Simultaneous regeneration | Present | 31 | 20 | 7 | 58 | 0.454 |
| Not present | 76 | 43 | 28 | 147 | 0.454 | |
| Loading time | 0-1 year | 74* | 33* | 18 | 125 | 0.002 |
| 1-3 years | 17 | 18 | 12 | 47 | >0.05 | |
| >3 years | 12 | 15 | 4 | 31 | >0.05 | |
| Type of prosthetic restoration | Screwed | 70* | 46* | 24* | 140 | 0.001 |
| Cemented | 3 | 9 | 11 | 23 | >0.05 | |
| Hybrid | 16 | 4 | 0 | 20 | >0.05 | |
| Overdenture | 0 | 7 | 1 | 8 | >0.05 | |
| Submerged | 4 | 0 | 0 | 4 | >0.05 | |
| Surgical complications | Present | 3 | 0 | 0 | 3 | 0.247 |
| Not present | 107 | 66 | 35 | 208 | 0.247 | |
| Post-surgical complications | Present | 1 | 0 | 2 | 3 | 0.056 |
| Not present | 109 | 66 | 33 | 208 | 0.056 | |
| Implant placement site | Anterosuperior | 25 | 7 | 6 | 38 | 0.906 |
| Anteroinferior | 10 | 5 | 3 | 18 | 0.906 | |
| Posterosuperior | 41 | 26 | 13 | 80 | 0.906 | |
| Posteroinferior | 34 | 31 | 15 | 80 | 0.906 | |
| Treatment for peri-implant disease | No treatment | 86 | 8 | 0 | 94 | >0.05 |
| Local decontamination | 0 | 55* | 22* | 77 | 0.000 | |
| Explant | 0 | 0 | 10 | 10 | >0.05 | |
| Adherence to peri-implant supportive therapy | Present | 34 | 20 | 9 | 63 | 0.699 |
| Absent | 76 | 48 | 29 | 153 | 0.699 | |
In the age analysis, it was found that the age group of 46-64 years was statistically significant for health (64 implants) and periimplantitis (22 implants) ( p=0.042). On the other hand, for the group 65-79 years old, 35 implants with mucositis were found, which was statistically significant ( p =0.04). Within the systemic condition, it was found that when they presented a systemic condition other than diabetes, no statistically significant differences were found for the peri-implant condition. When the analysis for diabetes was performed, it was found to be statistically significant for mucositis, found in 11 implants ( p=0.028).
Regarding the Silness and Löe index, a record was found for 121 implants, where statistically significant differences were found in the group of 16-30% in health, mucositis, and peri-implantitis ( p =0.009) and the group of 31-100% it was statistically significant for peri-implantitis ( p =0.009).
Within the time of implant placement, no statistically significant difference was found in the prevalence of peri-implant conditions ( p=0.645). No statistically significant differences were found in the implants with simultaneous bone regeneration ( p=0.454). When the implant loading time was analyzed, it was found that there was a statistically significant difference when the loading time was 0-1 year for both the health condition and peri-implant mucositis ( p=0.002). However, 61.6% of the evaluated implants belonged to the 0–1-year load group, so this variable’s sample number would explain this association and the follow-up times reviewed in the records; long-term follow-up terms are few, with the maximum follow-up time being eight years.
Regarding the type of prosthetic restoration, a statistically significant difference was found for health, mucositis, and periimplantitis when screw-retained restorations were performed ( p=0.001). However, 71.79% of the implants were found with a screw-retained restoration.
Regarding complications, no statistically significant differences were found for surgical ( p =0.247) and post-surgical ( p=0.056) complications. No statistically significant differences were found for the implant placement area ( p=0.906).
For treating peri-implant conditions, statistically, significant differences were found concerning treating some peri-implant diseases; non-surgical peri-implant therapy is typical for both periimplantitis and mucositis groups (p=0.000). No statistically significant differences were found regarding adherence to peri-implant supportive therapy ( p=0.699).
4. DISCUSSION
This study is the first published research in Bogotá, Colombia, based on the American Academy of Periodontology diagnostic criteria and the European Federation of Periodontology for periodontal and peri-implant diseases [ 11] to know the prevalence of peri-implant disease in UNICOC. In this study, a prevalence of peri-implant health of 50.93%, peri-implant mucositis of 31.48%, and periimplantitis of 17.59% were evidenced, showing that approximately half of the implants experience some peri-implant disease.
These data show a high prevalence of periimplantitis compared to the retrospective cohort study conducted by David French et al. (2018), where 2060 patients with an initial total of 4591 implants placed in Calgary (Canada) showed a prevalence of periimplantitis of 0.4% during the first 2 and 3 years of loading, and a prevalence of 7.7% at 8 and 10 years [ 15]. The general behavior of the patients is to return to the service when the patient has referred any symptom of illness. This may explain the high figures for peri-implant disease because, considering the findings of Weinstein et al. (2020) through a multicenter study of a total of 248 patients, only 10 of these presented at least one implant with periimplantitis (4.03%), with a total of 1162 implants, only 14 were affected (1.20%). However, they were patients whose follow-up was strict in a peri-implant supportive therapy [ 16 ], determining that non-attendance to these therapies is a risk factor for developing a peri-implant disease, with a medium-high level of evidence [ 17].
Regarding gender, the evidence has not established it as a risk factor for the development of peri-implant disease, nor has age, with a medium-high level of evidence [ 17]. However, in the present study, it must be kept in mind that most of the sample were women. However, it is impossible to establish a direct relationship with peri-implant disease nor with the age group to which the patient belonged since most patients who received dental implants at UNICOC clinics were older than 46 years.
Regarding the presence of diabetes and the development of peri-implant disease, it was shown that there was statistical significance ( p=0.028). However, the evidence remains controversial. Studies such as the one by Alberti et al. (2020) show that there is no relationship between diabetes and peri-implant disease [ 18], findings corroborated by Astolfi et al. (2022) where, in a retrospective study with 555 implants in 132 patients the diabetes was not established as a risk factor for the development of peri-implant disease, nor were systemic diseases such as arterial hypertension, osteoporosis, or cardiovascular disease; being concordant with the present study ( p=0.834). These same authors report something different for the variables: smoking and history of periodontitis, obtaining a statistically significant relationship, and the accumulation of bacterial plaque [ 19]. The last one is related to this research since Silness and Löe index values greater than 31% were related to the presence of peri-implant disease. The variables of smoking and history of periodontitis could not be considered for the present investigation due to the lack of information in dental records.
Parvini et al. (2020) studied the prevalence of peri-implant disease after immediate implant placement and loading in 47 patients with 64 implants; all patients were treated at the Department of Oral Surgery and Implantology at Goethe University., Frankfurt. A prevalence of peri-implant mucositis of 57.5% and peri-implantitis of 4.2% was observed. There is evidence of a higher prevalence of mucositis and a lower prevalence of periimplantitis compared to the data in the present study. In both studies, more women received implant therapy than men [ 20].
In Brazil, a study was conducted by Matarazzo et al. (2018) on 211 people, 135 women and 76 men, with a total of 748 implants. A higher prevalence was observed compared to the present study: 69.2% peri-implant mucositis and 29.5% peri-implantitis. Peri-implantitis was significantly associated with the male gender, contrary to what was found in this study [ 21].
In Colombia, Barrientos et al. (2018) conducted a study on radiographs at the Pontificia Universidad Javeriana of Bogotá, where they studied implants placed in patients between 18 and 92 years of age, where no statistically significant differences were found regarding sex and peri-implant disease [ 22], in the same way as reported at the CES University in Medellin by Duque et al. [ 14]. These authors found no statistically significant differences between the type of implant restoration and the development of peri-implant diseases. The prevalence of mucositis was 72.7%, and periimplantitis was 24.3%. The present study showed a statistically significant difference in health, mucositis, and peri-implantitis when screw-retained restorations were performed ( p=0.001). However, 71.79% of the implants were found with screw-retained restorations. Considering that no direct relationship is reported in the scientific literature between screw-retained restorations and the development of peri-implantitis, these data may be associated with the size of the implanted sample with screw-retained restorations.
Regarding the implant placement area, the findings go against what was reported by Song et al. (2020), who reported that both the maxillary and mandibular anterior areas had a higher prevalence of periimplantitis [ 23]. These findings may be related to the bone quality of the area and the predominant bone type, in addition to the low bone volume that generally corresponds to these anatomical areas.
Although adherence to peri-implant supportive therapy did not yield statistically significant data, a low percentage of patients who were attending frequently was observed in the study. The review by Monje et al. (2015) shows that the lack of adherence to peri-implant therapy is related to the incidence of peri-implant pathologies, for which it is essential to personalize peri-implant maintenance times and explain to the patient the importance of adhering to it [ 23-25].
Within the limitations of this study, it is found that the relationship between peri-implant disease and smoking could not be established because this condition was not wholly reported in the dental records. It was also not possible to obtain data on the history of periodontitis. These two variables have already been described as risk factors for developing the peri-implant disease. Also, the sample size can be expanded.
CONCLUSION
The prevalence of 49.07% of peri-implant diseases may be due to genetic, social, and demographic variations that may directly affect them, even with standardized diagnostic parameters. It is becoming increasingly clear that the most critical risk factors for developing the peri-implant disease are smoking, a history of periodontitis, and poor oral hygiene. This shows the need to schedule regular visits for peri-implant supportive therapy.
LIST OF ABBREVIATIONS
| PD | = Peri-implant Diseases |
| UNICOC | = Institución Universitaria Colegios de Colombia |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The institutional ethics committee of Institución Universitaria Colegios de Colombia (UNICOC) evaluated and approved the study with approval number 23-04-2021-06.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were per the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent has been taken from the patients for this study.
STANDARDS OF REPORTING
STROBE guideline has been followed.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the article’s findings are available in Zenodo at https://zenodo.org/badge/DOI/10.5281/zenodo. 7824134.svg reference number 10.5281/zenodo.7824134.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


