Imaging Techniques for Assessment of Cranio-maxillofacial Complications of Covid-19, A Systematic Review
Abstract
Objectives:
The aim of this review was to summarize and describe the reported imaging techniques used for COVID-19 patients who have developed cranio-maxillofacial complications.
Methods:
A systematic review of the literature was conducted using MEDLINE/PubMed, Google Scholar, and Scopus databases. Included articles were case reports/series, clinical trials and cross-sectional studies on adult COVID-19 patients that were written in English. Excluded articles were those discussing the radiological assessment of COVID-19 complications manifested in the oral mucosa or the extra-maxillofacial areas. Combinations of the following keywords were used: “COVID-19”, “Maxillofacial,” “complications,” “imaging,” “radiological,” “Mandible,” “Jaw,” “Osteonecrosis,” “cavernous sinus thrombosis,” and “mucormycosis.”
Results:
A total of 13 articles were included. Imaging techniques used were: magnetic resonance imaging (MRI), computerized tomography (CT), multislice CT (MSCT), contrast-enhanced MRI, contrast-enhanced CT, and cone beam CT. These imaging techniques were used in the diagnosis of craniomaxillofacial complications of COVID-19, including sinusitis, cavernous sinus thrombosis, jaw osteomyelitis, cellulitis, vision loss, and mucormycosis. CT and its variants were the most commonly used techniques.
Conclusion:
Within the limitations of the included studies, which were mainly case reports, it can be concluded that imaging techniques that were employed in the diagnosis of craniomaxillofacial complications of COVID-19 were limited to MRI, CT and their variants. Despite the efficiency of the utilized imaging techniques, clinicians worldwide should be aware of the most effective and least risk-associated methods used in such circumstances.
1. INTRODUCTION
Among viral respiratory tract infections, coronavirus disease-2019 (COVID-19) represents the most recently emerging type of non-localized respiratory infection that may present with severe disease outcomes. The disease caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is characterized by a wide range of extrapulmonary manifestations whereby several vital organs may sustain chronic or permanent injury. Despite a small minority of patients who develop an asymptomatic illness, a substantial proportion develop acute and chronic complications that affect almost all tissues. Vital organs affected include, among others, the heart, blood vessels, liver, kidneys and craniomaxillofacial structures [1]. Surgeons may encounter patients who have recovered from COVID-19 but are still lying under the burden of long-term morbidities, which scientists have warned against in anticipation of a multiorgan injury burden following COVID-19 infections [2]. Within the context of cranio-maxillofacial region, numerous complications have been described, including cavernous sinus thrombosis (CST), sinusitis, osteomyelitis, osteonecrosis, vision loss, and cellulitis of the face [3]. These complications are quite diverse and present in various forms according to the type of blood vessels affected by thrombosis/occlusion, location and severity of the inflammatory process, disease duration, history of comorbidities, immune response, and age of the patient, among other factors [4]. The severe morbidity associated with these complications necessitates early diagnosis to initiate timely management and prevention of irreversible outcomes of chronic tissue injury. Therefore, it is necessary to accurately differentiate and promptly diagnose disorders of the regional blood supply to the jaw and face when examining patients who develop these interrelated complications. It is also necessary to consider the diverse nature of involved structures, including bone and associated soft tissues, in the evaluation of inflammatory and necrotic changes associated with disease outcomes. On the other hand, it is important to appreciate the necessary indications and balance them with the possible disadvantages of performing such diagnostic techniques, which can entail increasing costs and adverse health risks of radiation. A wide variety of medical imaging tests are available for diagnosing bone disorders, such as radiography, ultrasound, magnetic resonance imaging (MRI), single-photon emission computed tomography (SPECT) and positron emission tomography (PET) [5, 6]. Other imaging tests are effective for identifying problems in blood flow and the condition of hard and soft tissues, such as multislice computed tomography (MSCT), computed tomography (CT) and magnetic resonance angiography (MR angiography).
Taking into consideration the wide variety of imaging techniques available and the urgency required for diagnosis and prompt management of COVID-19-associated craniomaxil lofacial complications, indications and guidelines for the use of proper diagnostic imaging techniques should be highlighted. Due to the increasing number of reported cases of craniomaxillofacial complications of COVID-19 [7], diagnostic methods that help identify and determine the severity of pathologies in the craniomaxillofacial region are warranted. Therefore, this systematic review aims at examining the relevant studies conducted among COVID-19 patients who developed craniomaxillofacial complications to describe and highlight the most commonly used imaging techniques in the diagnosis of these complications.
2. METHODS
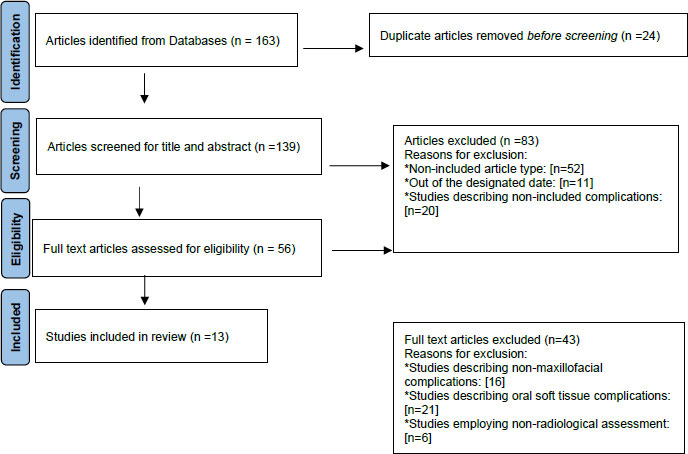
The review was conducted in accordance with PRISMA 2020 (Preferred Reporting Items for Systematic Review and Meta-analysis) guidelines [8]. The primary outcome was identifying types of imaging techniques used, and the secondary outcome was describing types of craniomaxillofacial complications diagnosed by these imaging techniques in COVID-19 patients.
2.1. Information Sources and Search Strategy
MEDLINE/PubMed, Google Scholar, and Scopus databases were systematically and thoroughly searched to identify published data on craniomaxillofacial complications of COVID-19 using the following combinations of keywords and Boolean Operators ‘AND’ and ‘OR’ as follows: “COVID-19” AND “Imaging” OR “Radiological” ‘AND’ “Maxillofacial” OR “Mandible” OR “Jaw” AND “Complications” OR “Osteomyelitis” OR “Osteonecrosis” OR “Cavernous Sinus Thrombosis” OR “Mucormycosis.” References of retrieved articles were manually searched for the same keywords.
2.2. Selection Process
The Mendeley Reference Manager was used to select articles. Two reviewers (N.D-O and E.Z-A.) independently selected the eligible studies. Any disagreement between reviewers was resolved by consensus or by a third reviewer (O.A-H.). Articles included in the review were assessed for quality by two researchers ((N.D-O and E.Z-A.) who worked independently. The Joanna Briggs Institute (JBI) critical appraisal tool was used to assess the quality of articles for this review [9]. According to this appraisal tool, methodological quality (risk of bias) for case series employed ten criteria, while that for case reports and cross-sectional studies employed eight criteria that were evaluated as a “yes,” “no,” “unclear,” and “not applicable.”
3. RESULTS
3.1. Study Selection
A total of 13 articles were determined to be appropriate for inclusion in this review. The flowchart that describes the selection process is presented in Fig. (1).
3.2. Study Characteristics
A total of 13 studies (two cross-sectional and 11 case reports/series were included Table 1).
3.3. Methodological Quality (risk of bias)
All case reports have satisfactorily addressed the JBI Critical Appraisal Checklist for case reports. In all case series, it was not possible to determine whether they had consecutive inclusion of participants. There were two cross-sectional studies included. In Rao et al., strategies to deal with confounding factors were not stated [13], and in Moorthy et al. [15], it was unclear if the study has addressed this item. Therefore all case series and cross-sectional studies were assessed to have a low risk of bias taking into consideration that one item (out of 10 in the case of series and out of eight in cross-sectional studies) was either missing or unclear (Table 2).
| S.No | Author (year)/Refs | Study Type | Country | Patient (s) Age (years), Gender |
Imaging Technique/s | CMF Complications |
|---|---|---|---|---|---|---|
| 1 | Eswaran et al (2021) [10] | Case report | India | 31, M | CE MRI CE CT |
Fungal sinusitis (maxillary, ethmoid, sphenoid sinus) Thickening of recti muscles Retrobulbar fat stranding CST Diffuse thrombosis with complete obstruction of the Right internal carotid artery, Diffuse erosion of the frontal bone Underlying meningeal thickening. |
| 2 | Boymuradov et al-1 (2021) [11] | Case report | Uzbekistan | 58, M | MSCT | Maxillary osteomyelitis Total shadowing of the right maxillary sinus |
| 3 | Boymuradov et al-2 (2021) [12] | Case series | Uzbekistan | Two M (65 and 68 years) Two F (62 and 67 years) |
MSCT MR angiography |
Maxillary osteomyelitis Cellulitis of the face Vision loss |
| 4 | Rao et al. (2021) [13] | Cross-sectional | India | 28 patients Mean age (49.1±10.8) M=78.6% |
MRI CT |
Mucormycotic pansinusitis Maxillary osteomyelitis |
| 5 | Shires et al. (2021) [14] | Case report | USA | 76 M | CT MRI |
Sinusitis, left orbital and periorbital abscess cellulitis, Maxillary osteomyelitis |
| 6 | Moorthy et al. (2021) [15] | Cross-sectional | India | 18 patients (15 M, 3 F) mean age= 54.6 (35-73) |
CT MRI |
Rhino-cerebro-orbital IFI Maxillary sinusitis/necrosis Cellulitis of the face |
| 7 | Chouhan et al. (2021) [16] | Case series | India | 41 patients 28 M and 13 F with a mean age of 48.2 (range, 21-68) |
CE MRI CE CT |
Rhino-orbital-cerebral mucormycosis Sinusitis CST |
| 8 | Arewar et al. (2021) [17] | Case report | India | 60 M | CT | Mandibular osteomyelitis |
| 9 | Dave et al. (2021) [18] | Case series | India | 58 patients 44 M (76%), mean age (55 ± 11, median= 56). |
CT CE MRI |
Rhino-orbital-cerebral mucormycosis Orbital cellulitis Cavernous sinus involvement Orbital apex involvement Sinus involvement |
| 10 | Ambereen et al. (2021) [19] | Case report | India | 39 M | CE CT | Mandibular mucormycosis |
| 11 | Arafat et al (2021) [20] | Case report | India | 57 F | CT | Mucormycotic Osteomyelitis of the Maxilla |
| 12 | Sai Krishna et al. (2021) [21] | Case report | India | 34 M 50 M |
CBCT CT |
Mucormycotic osteomyelitis of the maxilla and zygoma |
| 13 | Desai et al. (2021) [22] | Case series | India | 50 patients Age range (23-73) Males, n=29, 58% |
MRI CT |
Mucormycosis of the maxillary and ethmoid sinuses. Extension of disease to the orbit, cavernous sinus, hard palate, skull base, and intracranial involvement |
| Author (year)/Refs | Study Type | Level of Risk | Item | Assessment |
|---|---|---|---|---|
| Boymuradov et al. 2 (2021) [12] | Case series | Low | Did the case series have consecutive inclusion of participants? | Unclear |
| Rao et al. (2021) [13] | Cross-sectional | Low | Were strategies to deal with confounding factors stated? | No |
| Moorthy et al. (2021) [15] | Cross-sectional | Low | Were strategies to deal with confounding factors stated? | Unclear |
| Chouhan et al. (2021) [16] | Case series | Low | Did the case series have consecutive inclusion of participants? | Unclear |
| Dave et al. (2021) [18] | Case series | Low | Did the case series have consecutive inclusion of participants? | Unclear |
| Desai et al. (2021) [22] | Case series | Low | Did the case series have consecutive inclusion of participants? | Unclear |
4. DISCUSSION
This review summarized and highlighted the imaging methods used to diagnose craniomaxillofacial diseases that arise in association with COVID-19 as a complication of the disease itself or its treatment modalities. It reported studies that were mostly case reports and series originating mainly from India. This was expected considering the notable 2- fold increase in rhino-orbital mucormycosis in India during the COVID-19 era [23]. From a global perspective, literature published on mucormycosis has exponentially increased, with more than one thousand articles published since the emergence of the pandemic, which reflects the great interest in understanding and reporting this opportunistic invasive infection. Therefore, it is important, before discussing the utilized imaging techniques, to highlight the close pathogenic relationship of mucormycosis, jaw osteomyelitis and CST. In susceptible COVID-19 patients, rhino-orbital-cerebral mucormycosis is reportedly the most common type of mucormycosis [24]. It is initiated by inhalation of the fungal spores, and owing to the angioinvasive and thrombotic characteristics of these micro-organisms spread to neighboring structures ensues. This spread involves the paranasal sinuses, the nasal mucosa, turbinates, and palate, and eventually, it progresses to maxillary osteomyelitis, orbital involvement and vascular involvement of the carotid artery and cavernous sinus [24, 25].
Craniomaxillofacial inflammatory and necrotic diseases such as fungal osteomyelitis of the jaw predominantly involve the maxilla more often than the mandible due to the high susceptibility of the maxillary sinus to mucormycosis [24]. There is obviously a higher male gender prevalence in the studies reported in this review, probably because of the associated comorbidities such as diabetes mellitus [26]. Except for two studies that report mandibular involvement [17, 19], all studies included in this review reported lesions involving the maxilla in the form of sinusitis, osteomyelitis and mucormycosis. Therefore, it is necessary to utilize imaging techniques that identify diseases in hard and soft tissues as well as vascular involvement.
Seven types of imaging techniques were used in the included studies: MRI, contrast-enhanced MRI, MR angiography, CT, contrast-enhanced CT, MSCT and CBCT. Medical imaging tests, such as radiography, ultrasound, magnetic resonance imaging (MRI), single-photon emission computed tomography (SPECT) and positron emission tomography (PET), are often used to diagnose severe bone disorders such as osteomyelitis [6]. On the other hand, imaging methods such as multislice computed tomography (MSCT), computed tomography (CT) and magnetic resonance angiography (MR angiography) are effective diagnostic methods in determining the viability of blood supply and condition of hard and soft tissues.
MRI assumes an important role in the craniomaxillofacial region since it inherently has a better contrast resolution as compared to CT [27]. CT is the preferred diagnostic imaging technique used to evaluate sinuses, whereas the degree of extra-sinus involvement is best assessed by MRI [28]. MRI is based on the application of field gradients, strong magnetic fields, and radio waves [29, 30]. Hence, in contrast to CT which may be associated with exposure to high radiation [31], MRI substantially reduces the ionizing radiation-associated risks [32]. However, there remain a few disadvantages of the technique attributed to the time-consuming, claustrophobia-worsening, and expensive nature [33]. A recent systematic review concluded that osteomyelitis is reliably diagnosed by MRI, PET and SPECT, and in terms of diagnostic accuracy, they seem to be similar [6]. On the other hand, scintigraphy, CT and plain radiography showed inferior diagnostic accuracy when compared to the above three techniques [6]. Further, PET is recommended in situations where avoiding false-positive diagnoses is important, for example, when the test would be followed by surgery or other invasive procedures [6].
It was noticed that all studies reported in this review had utilized CT and/or MSCT, the latter type is usually used in disease screening and preventive medicine by utilizing a combination of X-rays and medical ultrasonography [34]. The frequent use of CT and MSCT is a cause of concern since CT has been described as one of the largest contributors to man-made radiation sources in healthcare as it currently accounts for a growing number of examinations worldwide with a possible increased tendency to develop malignancies [32]. The same can be said for MSCT, whereby there is a carcinogenic potential of radiation due to the destruction of cells and DNA [35, 36]. Only one study utilized CBCT [21], although this method has been recommended in the maxillofacial region for its accuracy and applicability in many clinical situations [37].
The benefits of using digital panoramic radiography in the diagnosis of osteomyelitis are questionable. This technique has been effectively used to confirm the structure and condition of the maxilla and mandible at the same time; however, radiographic signs of osteomyelitis may not be found in diagnostic radiographs as early as 4-8 days after onset [38]. Despite its high costs, MRI is probably the most widely recommended and used technique, being more accurate than radiography and able to detect osteomyelitis in its early stages [29]. On the other hand, PET and bone scintigraphy are more expensive and less widely available than MRI.
Ultrasound, on the other hand, avoids radiation exposure and is readily available, but its diagnostic accuracy is currently uncertain [39]. There is also a distinction between methods that provide two-dimensional images (radiography, scintigraphy) and those producing three-dimensional images (PET, MRI, CT, SPECT).
Contrast-enhanced MRI was used in three of the reported studies. Chouhan et al. (2021) found this technique helpful in identifying the extent of the disease in the postoperative period [16]. Further, they used it to determine the response of mucormycotic lesions to antifungal therapy and to detect residual disease [16]. On the other hand, Rao et al. (2021) used CT, and they recommended its use to evaluate maxillary bone involvement in mucormycosis complicating COVID-19 at an early stage to limit tissue necrosis [13]. However, Desai et al. (2021) considered that MRI is the technique of choice for assessing the intracranial and intraorbital extensions of mucormycosis because of its excellent soft-tissue resolution [22]. Therefore, they recommended a combination of contrast-enhanced MRI for its excellent soft-tissue resolution and CT for the bony component, which provides excellent information not only for early accurate diagnosis of infection but also for effective surgical management [22]. Contrast-enhanced MRI can be used to detect pathological lesions throughout the body and to detect peripheral arterial occlusive disease or flow-related abnormalities [40]. The use of contrast-enhanced CT/MRI is important because it shows the presence of heterogeneous and asymmetric filling defects, thrombosis in the superior ophthalmic vein, other venous tributaries, dural venous sinuses and cerebral veins when CST is suspected [41]. It is also helpful in the identification of orbital involvement as denoted by abnormal orbital fat density/signal intensity [41].
The findings of this study show that MRI (and its variants) and CT (and its variants) were the only methods used as diagnostic imaging methods for patients developing craniomaxillofacial complications. However, CT and related techniques (MSCT and CBCT) were collectively considered the most popular methods. Therefore, it is expected for healthcare systems, particularly in communities burdened by the craniomaxillofacial complications of COVID-19, to face a rise in risks associated with the use of CT in the future. Avoiding the use of other valid diagnostic methods, such as PET and SPECT, may highlight the unavailability and underuse of these techniques, particularly in countries that showed a high burden of craniomaxillofacial complications of COVID-19.
This review reported important findings with implications on the diagnostic process of COVID-19's immediate and long-term complications; however, it has limitations attributed to the nature of included studies. Included studies were in the main case reports/ series due to the characteristic geographic distribution of COVID-19 cranio-maxillofacial complications, particularly CST, mucormycosis and osteomyelitis. This necessitated the use of the JBI critical appraisal tool. This tool has been described by Ma et al. (2020) to be the only tool for the assessment of methodological quality or risk of bias for case reports and series [42]. On the other hand, this tool is also recommended by the same researchers for the assessment of cross-sectional studies. Therefore, all studies included were assessed by this tool, and it was shown that items of assessment were satisfactorily addressed. It is recommended that future studies on this topic to employ analytic methods to compare the effectiveness of various imaging techniques in diagnostic accuracy for cranio-maxillofacial morbidities such as osteomyelitis, mucormycosis, cellulitis of the face and CST.
CONCLUSION
Healthcare personnel directly responsible for the treatment of patients with CMF complications of COVID-19 have to take into consideration the urgent nature of these complications as well as the possible risks posed by ionizing radiation exposure. The selected imaging modalities have to ensure accurate diagnostic imaging examination and design the ideal management plan with the lowest possible radiation exposure.
LIST OF ABBREVIATIONS
| COVID-19 | = Coronavirus disease-2019 |
| SARS-CoV-2 | = Severe Acute Respiratory Syndrome Corona Virus-2 |
| CST | = Cavernous Sinus Thrombosis |
| IFI | = Invasive Fungal Infection |
| CMF | = Craniomaxillofacial |
| MRI | = Magnetic Resonance Imaging |
| CT | = Computerized Tomography |
| MSCT | = Multi-slice Computerized Tomography |
| CBCT | = Cone Beam Computerized Tomography |
| SPECT | = Single-Photon Emission Computed Tomography |
| PET | = Positron Emission Tomography |
| PRISMA | = Preferred Reporting Items for Systematic Review and Meta-analysis |
| JBI | = The Joanna Briggs Institute |
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
PRISMA guideline has been followed.
AVAILABILITY OF DATA AND MATERIALS
This was a systematic review, therefore are data is available in the manuscript as written in the proof.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.
SUPPLEMENTARY MATERIAL
PRISMA checklist is available as supplementary material on the publisher’s website along with the published article.
Supplementary material is available on the publisher’s website along with the published article.


