Profile Changes in Class III Malocclusion using Protraction Facemask in Indonesian Young Patients (Cephalometric Study)
Abstract
Background:
The prevalence of Class III malocclusion is highest in Southeast Asia. In countries such as Malaysia and Indonesia, the prevalence is as high as 15.80%. Treatment timing and options are very important in treating Class III malocclusion. A protraction facemask or also known as reverse headgear is one of the most used appliances as an interceptive tool for Class III malocclusion in young patients.
Objectives:
This study aims to evaluate the profile changes in treating Indonesian young patients using a protraction facemask.
Methods:
The sample consisted of 63 subjects, 25 males and 38 females. Lateral cephalograms were traced and analyzed using CephaloMetrics AtoZ™ ver. 12 (Yasunaga Computer Systems, Co. Inc., Hanando-Minami, Fukui, Japan). A total of 16 traditional cephalometric measurements (13 skeletal measurements and 3 dental measurements) were used to describe changes between pretreatment and posttreatment cephalograms. All recorded data were analyzed using IBM SPSS version 21 (IBM Corporation, Armonk, New York, USA).
Results:
SNA (p˂0.030), ANB (p=0.000), and Wits appraisal values (p=0.000) showed significant differences out of all measurements. FMA and occlusal plane also showed changes and indicated that a facemask is helpful with treatment.
Conclusion:
Timing, duration, and patient compliance are very important in the management of Class III skeletal malocclusion using a protraction facemask. The use of facemask therapy among Indonesian pediatric patients resulted in an anterior and downward movement of the maxilla, backward rotation of the mandible, and a better orthopedic response.
1. INTRODUCTION
Angle’s Class III malocclusion refers to an anteroposterior dental discrepancy that may or may not be caused by anteroposterior and vertical skeletal changes [1]. Per Angle, Class III malocclusion shows that the position of the mandible is in a more forward position in comparison to the maxilla. Tweed further classified Class III malocclusion into pseudo- Class III malocclusion and skeletal Class III malocclusion, and Moyers added the cause of the problem include osseous, dental, and/or muscular [2, 3]. Several characteristics of Class III malocclusion include concave profile, midface deficiency, protruding lower lip, anterior crossbite, posterior crossbite, mandibular dentoalveolar retrusion, and/or maxillary dentoalveolar protrusion [4, 5].
The prevalence of Class III malocclusion varies depending on ethnic groups, races, and geographic location. The prevalence of Class III malocclusion in North America is around 5%, which is low, while in European countries, it is around 4.9% [6-8]. In Middle Eastern countries, the prevalence is slightly higher at about 10.2%, and in Asian countries, the prevalence is highest, especially in the Southeast Asia region such as Malaysia and Indonesia, at about 15.80% [9-11].
Class III malocclusion has multiple etiologies. One of the main etiologies for Class III malocclusion is familial genetic or hereditary [12]. The Habsburg jaw is one of the most common examples of this where many members of the dynasty have a prognathic mandible [13, 14]. Environmental factors are not limited to enlarged tonsils, but, habit, chronic mouth breathing, trauma, nasal blockage, and abnormal tongue could also lead to Class III malocclusion [15].
Treatment timing and options are very important in treating Class III malocclusion. When dental malocclusion is associated with skeletal discrepancies (maxillary deficiency, mandibular excess, or combination), the treatment complexity increases [16]. Many Class III malocclusion patients seek early treatment due to their prominent facial appearance, which tends to appear as early as three years of age [17]. Treatment options for Class III malocclusion depend on the age of the patient, yet the older the patient, the more limited the treatment options are. Adult patient with Class III malocclusion most likely needs to have orthognathic surgery in addition to using an orthodontic fixed appliance. In contrast, in young patients, there are way more treatment options such as bite plane, removable appliances (with or without expander), proclination of upper teeth, Frankel appliance type III (FR-III), chin cup appliance, and protraction facemask (with or without expander) [1, 4, 18]. Each of these treatment options has its own indications and contraindication.
The two-phase treatment by doing early intervention (prepubertal growth peak) for treating young patients with Class III malocclusion show benefit by improving and creating a more favorable growth and occlusal relationship of the patient [19]. The first-phase treatment uses orthopedic devices such as a protraction facemask to correct the skeletal problem and yield favorable growth corrections in both the upper and lower jaw [20]. The second-phase treatment involves the use of fixed orthodontic appliances, continued growth monitoring, and establishing proper tooth position and interdigitation. The appropriate time to start this two-phase treatment on a very young patient depends on the patient’s chronological age and phases of dentition [21, 22]. In adolescents, cervical vertebral maturation and/or hand-wrist maturation will help [23].
A protraction facemask or also known as reverse headgear is one of the most used appliances as an interceptive tool for Class III malocclusion in young patients [24]. A protraction facemask was designed in the late 1960s by Delaire. It has two components: (1) an extraoral component which is the framework that fits on the forehead and chin (2) an intraoral component which includes an attachment to the maxillary dentition, and bilateral hooks to attach elastic [10]. The effect of the facemask can be achieved in all three dental planes, especially when combined with a rapid maxillary expander [18, 25]. Success rates depend on multiple factors such as patients’ compliance and time of treatment relative to patients’ growth [26]. Early start to treatment, especially when patients’ age is around 8-9 will lead to more skeletal effects than dental effects [20, 27, 28].
The protraction facemask is recommended to be worn at least 12-14 hours a day for about 7 to 9 months. Longer wear will also lead to faster correction. For severe cases, the patient can be asked to wear the facemask on a full-time basis (about 20 hours a day) except when the patient is eating and brushing [18]. The elastic force being used on each side is typically around 400-600 g. Evening and nighttime wear have been observed to show an increase in growth hormone factor [17, 18].
Studies have been published about the success rate and effect of protraction a facemask on Class III malocclusion therapy. However, no study has been done specifically on the Indonesian population, where the prevalence is one of the highest among all races and geographic locations [29]. The purpose of this study is to examine the effect of protraction facemask therapy on Indonesian young patients by analyzing cephalometric analysis and to compare it to studies that have been done on other patient based.
2. MATERIALS AND METHODS
2.1. Subjects
The sample consisted of 63 subjects, 25 males and 38 females, and was collected based on these inclusion criteria: (1) a developing Class III malocclusion identified by a combination of an ANB measurement of less than 1°, anterior crossbite or an edge-to-edge incisor relation; (2) pretreatment (mean 8.0 years) and posttreatment (mean 8.8 years) lateral cephalograms made on the same cephalostat and of good quality; (3) all subjects of Indonesian descent; (4) subjects treated with a banded jackscrew maxillary expansion appliance, and a protraction facemask (400 to 600 gm on both sides); (5) uses the same type of protraction facemask (Great Lakes, Tonawanda, NY – Reverse-Pull Face Crib) (6) no craniofacial anomalies. Exclusion criteria include (1) having craniofacial anomalies; (2) having syndromic or non-syndromic cleft lip and/or palate; (3) No previous treatment. All subjects were treated and monitored by the same orthodontist (HH) and were seen every four weeks. All patients were asked to wear the facemask 14 hours a day. On average, the patient uses the facemask for 8 months.
2.2. Lateral Cephalogram Analysis
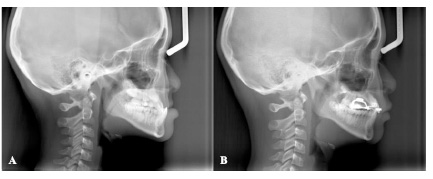
Pretreatment and posttreatment lateral cephalograms were traced side by side to provide consistent identification and location of landmarks between them (Fig. 1). Lateral cephalograms were traced and analyzed by the same investigator using CephaloMetrics AtoZ™ ver. 12 (Yasunaga Computer Systems, Co. Inc., Hanando-Minami, Fukui, Japan). A total of 16 traditional cephalometric measurements (13 skeletal measurements and 3 dental measurements) were used to describe changes between pretreatment and posttreatment cephalograms (Tables 1 and 2). Changes were measured according to differences in landmark position from T1 (pre-protraction facemask therapy) to T2 (post-protraction facemask therapy).
| Skeletal Measurements | |
|---|---|
| Measurements | Definition |
| SNA (o) | The angle measuring the relationship of the maxilla in relation to the anterior cranial base |
| SNB (o) | The angle measuring the relationship of the mandible in relation to the anterior cranial base |
| ANB (o) | The relative position between the maxilla and mandible |
| FMA (o) | The angle of inclination of lower border of the mandible to the Frankfort plane |
| IMPA (o) | The angle of the lower incisor to the mandibular plane |
| FMIA (o) | The angle of the lower incisor to the Frankfort plane |
| Wits appraisal (mm) | The appraisal of jaw disharmony |
| Gonion angle (o) | Most posteroinferior point on the angle of the mandible |
| Y-axis (mm) | A measure of the direction of facial growth and is formed by the angle between a line extending from S-Gn to the Frankfort plane |
| Facial angle (o) | The angle of recession or protrusion of the chin and the inferior internal angle between the facial plane and Frankfort plane |
| SArGo (o) | Representing the intersection of three radiographic images: (1) the inferior surface of the cranial base (2) the posterior outlines of the ascending rami (3) dorsal contour of the mandibular condyle bilaterally |
| Occlusal plane (o) | The angle between occlusal plane to Frankfort horizontal plane |
| Dental Measurements | |
|---|---|
| Measurements | Definition |
| U1 to FH (o) | Angle from upper central incisor to Frankfort Horizontal plane |
| L1 to MP (o) | Angle from lower central incisor to mandibular plane |
| U1 to L1 (o) | Angle between upper central incisor to lower central incisor |
3. RESULTS
Cephalometric mean measurements pre and post-treatment for the total samples are shown in Table 3. Table 4 showed the statistical paired t-test comparing the means and standard deviations of the related group to determine if there are significant differences. SNA (p˂0.030), ANB (p=0.000), and Witts (p=0.000) values showed significant differences between pre-treatment and post-treatment for the group that wore their facemask. FMA (p<0.070) and occlusal plane (p<0.092) also showed changes and indicated that a facemask helps with treatment and skeletal changes. There were no significant differences between males and females in the treatment results and duration of treatment.
| S. No. | Measurements | Pre | SD | Post | SD |
|---|---|---|---|---|---|
| 1 | SNA | 82.7633 | 4.7362 | 86.0847 | 8.8261 |
| 2 | SNB | 84.2560 | 5.3547 | 84.7903 | 6.9169 |
| 3 | ANB | -1.1810 | 2.2795 | 1.2670 | 3.9392 |
| 4 | FMA | 33.9780 | 5.5668 | 35.4600 | 6.9627 |
| 5 | IMPA | 88.8303 | 8.9099 | 88.5873 | 9.4547 |
| 6 | FMIA | 57.1907 | 7.9541 | 55.9803 | 9.9976 |
| 7 | NSAr | 120.9503 | 6.3033 | 119.6677 | 8.1810 |
| 8 | Witts | -8.8080 | 3.1407 | -5.1023 | 3.3930 |
| 9 | Go angle | 135.8290 | 7.7685 | 136.3917 | 8.4348 |
| 10 | Y Axis | 64.1353 | 3.8015 | 65.1477 | 4.9857 |
| 11 | Facial angle | 85.3453 | 3.7620 | 85.6437 | 5.2333 |
| 12 | SArGo | 138.4720 | 9.2941 | 139.9067 | 9.3175 |
| 13 | Occlusal Plane | 13.5207 | 4.3559 | 12.0040 | 4.7945 |
| 14 | U1 to FH | 119.8203 | 8.2421 | 121.5397 | 8.0248 |
| 15 | L1 to MP | 88.8303 | 8.9099 | 88.5607 | 9.4081 |
| 16 | U1 to L1 | 117.4693 | 11.6385 | 114.4393 | 11.8443 |
| S. No | Measurement | Mean Diff. | t | sig | p sig |
|---|---|---|---|---|---|
| 1 | SNA | 3.32133 | 2.284 | 0.030 | * |
| 2 | SNB | 0.53433 | 0.441 | 0.663 | - |
| 3 | ANB | 2.44580 | 4.893 | 0.000 | * |
| 4 | FMA | 1.48200 | 1.879 | 0.070 | ** |
| 5 | IMPA | -0.24300 | -0.129 | 0.898 | - |
| 6 | FMIA | -1.21033 | -0.600 | 0.553 | - |
| 7 | NSAr | -1.28267 | -0.989 | 0.331 | - |
| 8 | Witts | 3.70567 | 5.451 | 0.000 | * |
| 9 | Gonion angle | 0.56267 | 0.517 | 0.609 | - |
| 10 | Y-axis | 1.01233 | 1.318 | 0.198 | - |
| 11 | Facial angle | 0.29833 | 0.388 | 0.701 | - |
| 12 | SArGo | 1.43467 | 1.036 | 0.309 | - |
| 13 | Occlusal Plane | -1.51667 | -1.744 | 0.092 | ** |
| 14 | U1 to FH | 1.71933 | 1.067 | 0.295 | - |
| 15 | L1 to MP | -0.26967 | -0.144 | 0.887 | - |
| 16 | U1 to L1 | -3.03000 | -1.147 | 0.261 | - |
**: 1<P<.05
4. DISCUSSION
Skeletal Class III malocclusion with either combination of maxillary retrognathism, mandibular prognathism, or both, provide challenges for an orthodontist. It is very difficult to predict the craniofacial growth of every patient. Even though it is very important to be able to predict children’s future growth for many specialties, not only the orthodontist, to this day there is no accurate method to do so [30]. Mandibular growth is even more unpredictable. Orthodontists rely mostly on cervical vertebral analysis and hand-wrist bone analysis to help predict and analyze the growth pattern of patients [31, 32]. The cervical vertebral analysis is very advantageous because the orthodontist does not need to take an additional radiograph to the patient.
The benefits and success of early orthopedic treatment using a protraction facemask with or without maxillary expansion have been well documented [11, 20, 29, 33]. The optimal timing remains unknown, but many studies have suggested early start will result in more orthopedic results. According to McNamara, the optimal timing to achieve orthopedic results should be started at early mixed dentition [34]. Hickham mentioned that prior to age 8 is the best time to achieve the optimal orthopedic result, and Proffit advised prior to age 9 to get more skeletal changes than dental changes [1, 35].
The mean age of all patients used for this study was age 8.0. Significant changes were found on three skeletal measurements (SNA, ANB, and wits appraisal). The increased value on SNA and ANB suggested an anterior movement of point A due to the orthopedic forces of the protraction facemask. Changes to the FMA and occlusal plane showed an anterior and downward growth along with a clockwise rotation to the mandible and/or occlusal plane. The skeletal and dental effects can be seen by using a protraction facemask. Skeletally, the maxilla will move forward and downward. The anterior palatal plane will move slightly upward, while the posterior palatal plane will move slightly downward. The mandible will have a downward and backward rotation, which leads to improvement of the maxillomandibular skeletal relationship in the sagittal plane and an increase in lower anterior facial height. Dentally, the upper anterior teeth will have an increase in labial inclination and the lower inclination decreases (Fig. 1) [28]. Significant improvement could be seen for the soft tissue, as the skeletal relationship improves (Fig. 2). Soft tissue profile became more convex after a few months of treatment.

In comparison to other studies that have been published in the literature for other races, the changes were found to be similar. Shanker et al. [36] suggested that treating patients during the early mixed dentition stage will lead to a more significant movement of point A if compared to the untreated control. Three-quarter of the changes to point A was due to the skeletal maxillary advancement while the other quarter was due to skeletal remodeling that happened during growth and incisor tooth movement. The 12-month and 24-month posttreatment follow-ups indicated very little to no relapse of the achieved maxillary advancement in the treatment group. The estimated maxillary changes also resemble the control group.
Baik studied the use of maxillary protraction in 60 Korean children [37]. Out of the 60 patients, 47 were treated using a protraction facemask and palatal expander, while the other 13 were treated only using a protraction facemask and labiolingual appliances. Like the study of Shanker et al. and our study, significant forward changes in point A were found, especially in the group that was treated with the maxillary expander.
The study that was completed on 30 Chinese patients with skeletal Class III and maxillary retrognathism, using a maxillary palatal expander and protraction facemask in the mixed dentition stage showed that four years after removal of appliance, 70% of these patients still showed positive overjet [38]. The follow-up of 8 years old showed that 67% of the patients that came back still show a positive overjet. From the sagittal plane, the changes were similar between the stable group and the relapse group. However, the relapse group has a slightly higher increase in the lower facial height and the mandibular plane has opened more. Dental compensation in both the stable and relapse group are similar, but the mandible had outgrown the maxilla four times in the relapse group, in comparison to two times in the stable group. The authors stated that a third of the Chinese patient had a high potential to be the candidate for orthognathic surgery later in life due to unfavorable growth patterns [39].
Another group of authors did a study on Italian children that have undergone treatment using palatal expansion with a protraction facemask [20]. The treatment was started prepubertal growth spurt (mean age: 8 years, 3 months), while the final observation was completed roughly six years later (mean age: 14 years, 10 months). There was a slightly greater increase in midfacial length (1.6 mm) in the treatment group when compared to the control group. The mandibular length of the group increases by 2.4 mm more in the control group in comparison to the treated group. The untreated control also showed more Class III relationship (-2.7 mm) in comparison to the treated group (3.4 mm) [20].
Merwin et al. [40] showed that older patients (8-12 years old) will result in more dental changes such as maxillary molar extrusion (1.7 mm) versus younger patients (5-8 years old). There is also a greater increase in lower facial height in the 8-12 years old group in comparison to the 5-8 years old group. In general, the protraction facemask with or without the palatal expansion is an effective method to intercept and altered in children with skeletal Class III malocclusion [41].
The benefit of doing this conventional treatment is the ability to modify the intraoral component of the appliance based on each patient’s needs. The attachment to the maxillary dentition could be removable, bonded (using acrylic), and banded. An additional component such as a jackscrew to help expansion could be added. The decision of each depends on the treating clinician. For example, bonded version could help as a temporary bite-plane effect but may be the least comfortable option. Furthermore, compared to bone-anchored maxillary protraction, this treatment option is less invasive and costs less for the patient. On average, many of the studies done on the bone-anchored maxillary protraction technique are used on late mixed dentition, early permanent dentition patients or patients around 11-12 years old [42, 43]. This is why early diagnosis of Class III patients is very important.
Timing, duration, and patient compliance all play an important role in the success of the treatment. Successful early treatment in treating Class III malocclusion led to a reduced chance of the future need for more invasive procedures or even orthognathic surgery. However, it is not a fully guaranteed result. Continuous growth monitoring should be done to prevent significant relapse.
CONCLUSION
The use of protraction facemask therapy among young Indonesian pediatric patients resulted in an anterior and downward movement of the maxilla, backward rotation of the mandible, and a better orthopedic response. Facemask therapy is an appropriate intervention to treat skeletal Class III malocclusion in this Southeast Asian region. Continuous monitoring after completion of phase I treatment is always recommended and phase II should be proceeded based on the clinician’s decision.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The protocol was approved by the ATSU, Arizona IRB Committee (IRB #2015-47, date of approval April 24, 2015).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were according to the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained prior to initiating the study.
AVAILABILITY OF DATA AND MATERIALS
Data supporting the findings are available based on request from the corresponding author [H.H].
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


