All published articles of this journal are available on ScienceDirect.
Knowledge and Clinical Practice of Restoration Repair among Dental Undergraduate Students in the Kingdom of Saudi Arabia
Abstract
Background:
The expeditious advances in minimally invasive dental techniques have led to more conservative treatment options for the repair and refurbishment of defective restorations.
Objectives:
This cross-sectional study aimed to evaluate the knowledge and clinical practices of restoration repair in undergraduate courses in the central region of Saudi Arabia.
Methods:
Data was collected using a survey questionnaire that was distributed using Google forms through social media platforms among undergraduate dental students from different universities in the central region of Saudi.
Results:
A total number of 316 undergraduate students responded, with 77.8% reported having been taught about restoration repair in their undergraduate preclinical courses and 77.2% having practiced restoration repair in their clinical courses. The dominant collective response of the students was that they would opt for repair over replacement to preserve tooth structure and protect the pulp. The most chosen indications for such were the correction of form and partial fractures. Composite was the material of choice for repair, and the students considered the size of the defect to be the most decisive factor in their clinical decision of whether to repair or replace defective restorations.
Conclusion:
The results of this study indicated that restoration repair is taught in preclinical courses and is practiced in the clinic. Students at higher levels are more aware of the procedure and its indications. Based on available evidence, periodic evaluation of clinical teaching strategies, standardization of criteria, and terms are recommended to enhance teaching practice.
1. INTRODUCTION
The constantly improving developments in dental biomaterials and minimally invasive techniques have led to the reconsideration of the total replacement of partially defective restorations [1]. With the advent of newer dental materials and continuous adhesion research evolution, restoration repair and refurbishment are now valid treatment options when the defects are localized [1-3]. When restoration is repaired, a conservative removal of the defective part is indicated, while refurbishment entails the mere refinishing of the restoration for smaller defects and stains [2]. These procedures result in clinically acceptable restorations and increased longevity [4], with little need for local anesthetic use and lesser aggressive tooth structure removal and time consumption [1-4].
Many studies have evaluated the decisive criteria for dental restoration repair and refurbishment and their effect on the expected longevity of the restoration. The most common indications reported for repair are marginal defects or staining, superficial color correction, bulk fracture, and wear of the restoration [1, 2, 4]. Furthermore, researchers in different universities attempted to evaluate whether dental students received classroom teaching on dental restoration repair and if they have practiced it clinically [5-12].
Blum et al. [9] reported that the majority of dental schools in the UK, Germany, and Scandinavia instructed on the repair of direct composite restorations. However, marked variations were observed with respect to this teaching practice and the expected longevity of the repaired restorations. Reportedly, in the US and Canada, although teaching repair of defective resin-based composite restorations was included in the didactic curricula of most schools, the students’ clinical experience was insufficient [11].
In the Kingdom of Saudi Arabia, however, a limited number of studies were conducted relative to the subject. A survey at King Abdulaziz University in Jeddah [6] reported that 70% of the dental students were taught the indications for the repair of dental restorations, but only (42.7%) have performed it. In another study conducted in three other universities in the southern region of the Kingdom of Saudi Arabia, a total of 61.5% of the surveyed students reported not being taught about composite repair for their bachelor’s of dental surgery [5]. No published studies were found about the teaching and practice of dental restoration repair in the central region of Saudi Arabia or the city of Riyadh.
Dental undergraduate programs in Riyadh are taught by many universities using different teaching approaches and some of these programs are fairly new [13]. An evaluation of the teaching methodologies of new techniques and minimally invasive dental procedures could provide valuable insight [14].
Our study aimed to provide insight into the knowledge and clinical practices of dental restorations, repair, and refurbishment among undergraduate dental students from different universities in the central region of Saudi Arabia.
2. MATERIALS AND METHODS
This cross-sectional descriptive study was conducted using a Google forms survey questionnaire distributed through the social media platforms such as WhatsApp, Telegram, and Twitter among undergraduate dental students from different universities in the central region of Saudi Arabia. The study protocol and questionnaire were reviewed and approved by the Institutional Review Board at King Saud University (IRB Project # E-21-6259). The questionnaire was anonymously structured comprising fifteen closed-ended and a single open-ended question. The sample size was 369, which was calculated by assuming a knowledge of 60% with a precision of ±5% for a 95% confidence interval.
The first section of the questionnaire was designed to collect demographic data such as information about dental students’ current undergraduate program and education level. The second section was structured to cover two categories of knowledge and practice of dental restoration repair and refurbishment, indications, and frequency of use.
The collected data was categorized using Microsoft Excel and analyzed using SPSS 26.0 statistical software (IBM Inc., Chicago, USA).
Descriptive statistics (frequencies and percentages) were used to describe the categorical variables (demographic data, undergraduate program, and items of knowledge and practice). Pearson’s chi-square test was used to observe the statistical significance of categorical responses to items of knowledge and practice and to compare the distribution of these responses in relation to university type and student level of study. A p-value of ≤ 0.05 was used to report the statistical significance of the results.
3. RESULTS
A total of 316 (85.6%) out of 369 participants had completed the study questionnaire. The respondents were almost evenly distributed among third-, fourth- and fifth-year levels. However, the majority of the participants were females (67.1%) and studied at government-funded dental colleges (87%).
A highly significant percentage of students involved in the study (77.8%) reported being taught about restoration repair. More than half of the surveyed students confirmed that their knowledge acquired about restoration repair/replacement was prior to clinical operative courses during their second (25.6%) and third year (32%) levels of the undergraduate program. However, a highly statistically significant (p < 0.0001) percentage (78.5%) responded negatively when asked whether they were familiar with the term “restoration refurbishment.” Furthermore, only 42.6% of the students that claimed familiarity with the term “refurbishment” were able to define it correctly.
Knowledge about restoration repair was assessed with multiple response questions. Each response percentage under these items was compared with a hypothetical percentage of equal distribution, which is 50%.
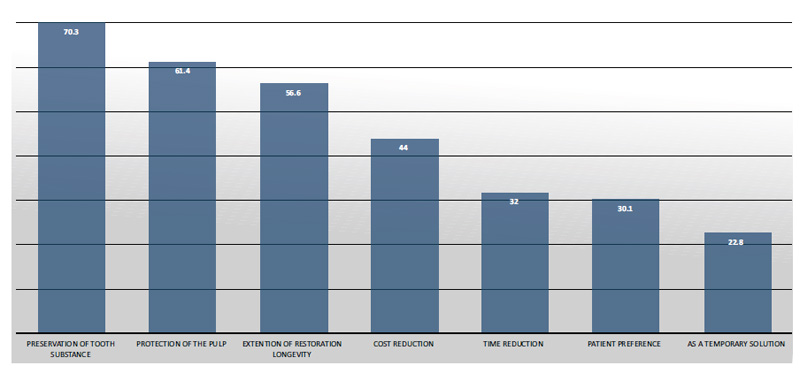
When asked about the main reasons why they would opt for restoration repair over replacement, the reason of majority of the participants was the preservation of tooth substance and pulp protection. The percentages of these two responses were highly significant. Furthermore, 56% of respondents chose to extend the longevity of restorations, while all other responses of patient-related factors such as reduction of treatment cost and time, patient’s preference, and using repair as a temporary solution were chosen by less than 50% (Fig. 1).
The comparison of study subjects’ responses to this specific item of knowledge among the three levels of students showed significantly higher response percentages for the students from the fourth-year and fifth-year compared to the third-year students.
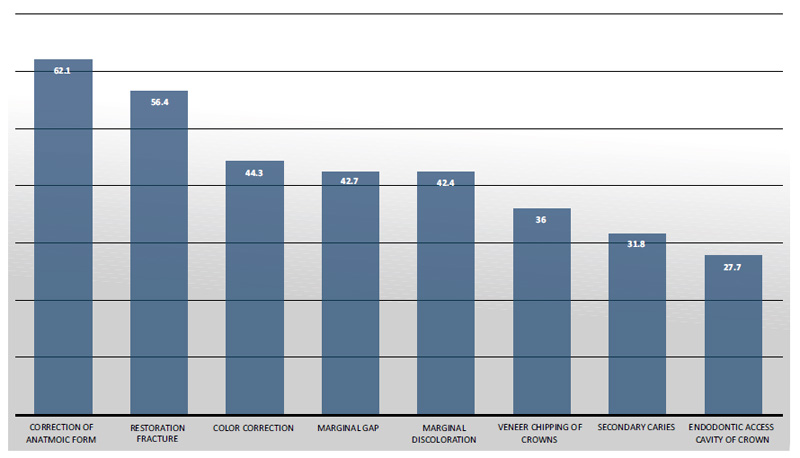
As for indications of repair, the percentages of the two responses, partial restoration fracture and correction of anatomic form, were statistically significant, while the students’ choice of the remaining responses—secondary caries, correction of color, marginal gap, marginal discoloration, veneer chipping of crowns and endodontic access cavity of the crown—were less than 50% (Fig. 2).
The comparison of the study subjects’ responses towards the abovementioned items of knowledge about the possible reasons and indications for restoration repair between the type of university (government and private) showed a statistically significant higher choice of multiple responses of the students from government universities compared to those from private universities.
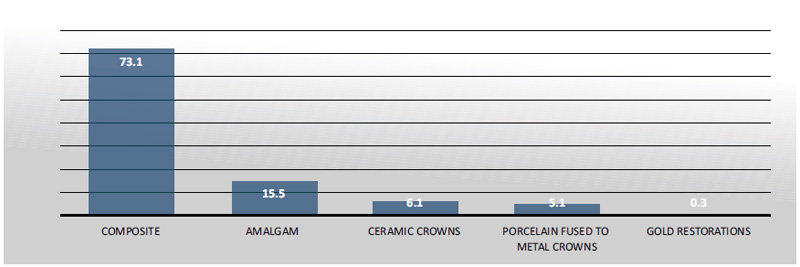
Regarding the clinical practice of restoration repair, only 22.8% of the students reported having never practiced repair. A total of 73.1% of students reported practicing restoration repair on composite restorations and only 15.5% on amalgam (Fig. 3).
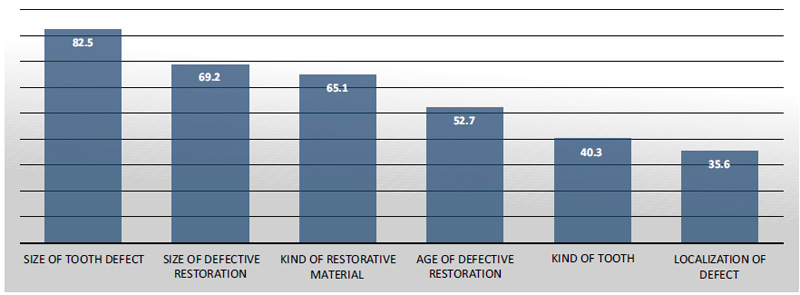
In the clinical practice item, when deciding to repair or replace a restoration, which clinical factors play a role? The different percentages are shown in Fig. (4). The responses to the size of the defect, the kind of restorative materials, and the size of overall defective restoration were found to have percentages of more than 50%, which is statistically significant. Other responses included the age of defective restoration (52.7%), localization of the defect, and tooth kind (less than 50%).
The students who thought that the kind of tooth plays a role in the decision-making of restoration repair responded that they were more likely to choose repair in molars (49.4%) and anterior (40.3%) rather than premolars (10.3%). These differences in percentages are statistically significant (p < 0.0001).
Upon the comparison of the study subjects’ responses when asked about performing repairs in the dental clinic, it was found that students from the fourth- and fifth-year levels had significantly higher responses than those from the third year (p = 0.006). Furthermore, when comparing their responses to clinically deciding factors about restoration repair, the percentage of responses for the size of the defect, kind of restorative material, size of the defective restoration, localization of defect, and age of defective restoration were statistically significantly higher in students from the fourth- and fifth-year levels when compared to the third-year students. Finally, the differences in the frequency of clinical practice of restoration repair between government- and private university students were statistically insignificant.
4. DISCUSSION
In the last couple of decades, new dental colleges have been established in Saudi Arabia. Some have a well-established basis while others are still building their academic strength. It has been suggested that more research is needed to evaluate the effectiveness of the taught curricula and to address important questions about the currently offered dental programs [13, 14].
This cross-sectional study aimed to provide insight into the teaching practices and clinical implementation of restoration repair in operative courses of dental undergraduate programs in the central region of the country.
Longitudinal clinical studies have established restoration repairs in permanent teeth to be a valid treatment with many advantages of extending restoration longevity, and preservation of tooth substance along with cost and time reduction [1-5]. The specific criteria of when and how restorations are to be replaced should be clearly outlined and taught to students to prevent high numbers of unnecessary aggressive replacements for restorations with localized defects. It has been reported that dental restoration replacement constituted 40.9% of activities performed in general dental practice in Saudi Arabia [15].
To evaluate their knowledge about dental restoration repair, the undergraduate students who participated were interrogated about the classroom teachings of the subject. The majority of our undergraduate students responded positively. This is in line with a previously reported percentage (70.7%) of students reporting being taught about the indications of restoration repair in a study conducted in the city of Jeddah, Saudi Arabia [6]. On the other hand, when a similar question was asked in universities in the southern region of Saudi Arabia, only 38.5% reported being taught about resin composite repair [5]. In 2021, a comprehensive study of the teaching status of defective resin-based composite restoration repair in dental schools in Middle Eastern and North African (MENA) countries reported that 69% of schools taught repair as an alternative to the replacement of restorations. Of the schools that are not teaching repair, 80% indicated that they plan to include this topic in the curriculum within the next five years. Most schools taught theoretical and practical aspects of repair only at a clinical level [16].
Most of the undergraduate dental programs in the Kingdom of Saudi Arabia last for five years, and the students start their operative courses in their first year. However, the clinical component of the operative courses does not begin until the third-year level. This explains why the teaching of restoration repair in the dental curriculum began to be offered before the fourth-year level when students begin to gain their clinical expertise and implement what they learned during their classroom teaching.
In the current study, the respondents were instructed to choose from several preset responses when asked why they would opt for restoration repair rather than replacement, the probable indications for initiation of restoration repair, and the preferred dental materials for repair. Furthermore, the students were asked whether they had practiced restoration repair during their undergraduate courses, which restorations were repaired, and what clinical factors affected their decisions. The responses listed in the questionnaire were adapted after an extensive review of similar questionnaires and the available literature on the different tooth- and patient-related factors pertaining to restoration repair and replacement [1-11].
The decisive criteria and reasons why a clinician may choose to repair a partially defective restoration are ambiguous in the literature. Studies have categorized these indications into tooth/restoration-related and patient-related factors [1-3, 16]. Restoration repair is generally associated with a more conservative approach, delaying the so-called “restoration death spiral” [1].
When asked about why they would opt for restoration repair rather than replacement, preservation of tooth substance and protection of the pulp were the two most chosen responses. The choices of students were clearly in line with the current research, stating that teeth with repaired restorations are less likely to require further aggressive interventions such as endodontic or surgical treatment compared to the replaced restorations [17]. Research has also proven that repairs extend the longevity of the existing restorations [4], and that replacement should be considered as the last resort when there are no other viable alternatives [17]. Nonetheless, it should be noted that the restorative material, number of surfaces involved, tooth type, and the primary reason for treatment can influence the longevity of repaired restorations [18].
Regarding the indications of restoration repair, partial fractures and correction of anatomic form were the most chosen answers. Our findings are in line with previously reported answers from students in the Middle East, Africa [16], the United Kingdom, and Ireland [7], where students thought that partial material loss and marginal defects were the most common indications. On the other hand, secondary caries was reported to be the main indication for intervention in other studies in Saudi Arabia [5, 6].
Although a high percentage of respondents chose correction of anatomic form as one of the clinical indications of restoration repair, most of the study’s participants reported not being familiar with the meaning of the term “refurbishment.” These findings are similar to a previously published percentage of only 18% of surveyed students in Jeddah being aware of the term [6]. Refurbishment is comprised of procedures that include resurfacing, reshaping the anatomic form, and removal of any excess material by contouring and finishing the surfaces of defective restorations. It can be done if the defects are adjustable without damaging the tooth [19]. This implies that operative course lectures need to be updated periodically to keep up with the swift advancements in materials and clinical terms.
In the clinical practice component of the questionnaire, the majority of the students in our study reported practicing some kind of restoration repair. This is an important question as the steps and skills of different restoration repair protocols may be taught in the didactic component but are rarely if at all, implemented in preclinical course exercises.
Dentistry learning has three main domains: cognitive, affective, and psychomotor. Restoration repair is a practice involving cognitive treatment planning, along with the operative skill to perform the required treatment. In 2013, a study conducted in Saudi Arabia showed that students’ acquired didactic knowledge scores were not always positively correlated with their clinical performance of the skills [20]. This supports the need for students to practice restoration repair during their clinical courses in order to be able to adapt these techniques and apply them in their future practice.
In a clinical setting, the decision of restoration repair, or replacement when faced with a defective restoration should be based on a solid evaluation of the location, size, and extent of the defect. The most commonly adopted criteria for restoration evaluation are the modified US Public Health Service (USPHS)/Ryge criteria and FDI (World Dental Federation) criteria. Both criteria rely on certain functional, biological, and esthetic parameters that are used for the assessment of the restorations that result in a decision of a clinically acceptable or unacceptable restoration. The FDI criteria were proposed to be more sensitive, resulting in less invasive treatments when dealing with defective restorations [21-23].
In the current study, students have chosen the size of the defect, the kind of restorative material, and the size of the overall defective restoration to be the most influential clinical evaluation factors when choosing to repair restorations. Furthermore, they have indicated that the highest clinical repairs were performed on composite restorations. Many studies have reported composite to be the material of choice for restoration repairs [6, 18]. This can be explained by the marked enhancement of resin composite materials in recent years, their ability to bond to existing composites and tooth surfaces, and their proven potential to reinforce the existing tooth structure, particularly in large restorations of molar teeth [18, 24]. Since 1998, direct restorations using resin composites have exceeded the use of amalgam by far, due to the enhanced mechanical properties of composites, along with the esthetic and health concerns related to amalgam use [24]. Moreover, Gordan et al.. [18] stated that while the reasons for the replacement of amalgam restorations have remained fairly constant, the reasons for the failure of composite restorations and their longevity have changed markedly during recent years.
Restorations on molar teeth were the most chosen for repair by our respondents, followed by anterior and then premolars. These results were in line with previously published data revealing that practitioners were more likely to repair molar restorations. The possible explanation is that molar teeth received most of the biting forces, and their restorations were likely to involve a higher number of surfaces [18].
When the demographic data of our respondents were reviewed, the majority were noted to be females from government universities. Becker [25] analyzed gender effects on survey participation and reported many theories on why females had higher response rates in surveys, such as susceptibility to communication, helping norms, and interest in sharing opinions with others.
Furthermore, fourth- and fifth-year students had evidently selected an increased number of responses in both knowledge and practice items. This could be due to their broader clinical experience and advanced exposure in their studies. We also found that the knowledge about restoration repair and replacement in government students was higher than that of private students. However, the difference in the frequency of clinical practice of repair between government and private university students was insignificant. This observation could be related to the differences in teaching practices and curricula between universities, proving that continuous evaluation and comparison between teaching strategies and outcomes can provide valuable insight for improvement.
CONCLUSION
The results of this study indicate that restoration repair is taught in preclinical courses and is practiced in the clinic. Students at higher levels are more aware of the procedure and its indications. Based on available evidence, periodic evaluation of clinical teaching strategies, standardization of criteria, and terms are recommended to enhance teaching practice.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study protocol and questionnaire were reviewed and approved by the Institutional Review Board at King Saud University (IRB Project # E-21-6259).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were according to the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT TO PARTICIPATE
The study does not disclose personally identifiable information and poses no risk to the participant’s data.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available at: https://docs.google.com/file/d/17zTpqS vS2IkZfvpNpskTH geu6RIqQ4-W/edit?filetype=msexcel
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
FUNDING
None.
ACKNOWLEDGEMENTS
Declared none.


