All published articles of this journal are available on ScienceDirect.
Trans-Sinus Implant using TTPHIL-ALL-TILT ®Technique as an alternative to Sinus lifts: A Technical Description and Case Series
Abstract
Background:
Severe atrophy of the maxillary ridge and extended maxillary sinus pneumatisation limits the treatment options available for rehabilitating patients with teeth missing in the posterior maxilla. Sinus lifts followed by bone grafting have become the norm for rehabilitating such patients. Nonetheless, sinus lift procedures can be cumbersome, time-consuming, and uneconomical, especially if patients are in need of immediate function.
Objective:
This case series describes a unique combination of placing trans-sinus implants using the TTPHIL-ALL-TILT ® technique for treating patients with the atrophied posterior maxilla.
Methods:
Three different clinical situations have been described where the trans-sinus placement of implants using the TTPHIL-ALL-TILT ® technique was done for managing atrophied posterior maxilla. The first case was that of a single tooth missing in the posterior maxilla, the second of multiple posterior tooth missing (distal extension, partially edentulous condition) and the third being that of a completely edentulous maxilla. The implants were placed in a flapless tilted manner along with double bi-cortical engagement through the maxillary sinus.
Results and Discussion:
Following prosthetic rehabilitation, clinical reviews were performed after 6 months. In all cases, implant stability was manually checked and no pathological symptoms or signs were recovered at any follow-up visit.
Conclusion:
Trans-sinus implants using the TTPHIL-ALL-TILT ® technique prove to be a good choice to rehabilitate these three clinical scenarios. All three patients were extremely satisfied with the treatment outcome. This could very well become a convenient treatment alternative to sinus lift procedures.
1. INTRODUCTION
The rehabilitation of the atrophic maxilla in the posterior region poses a challenge due to anatomical limitations associated with sinus pneumatisation and bone atrophy. The absence of adequate bone volume causes a major limitation for implant insertion, especially when an immediate function is implemented [ 1]. To overcome such a limitation, there are several alternatives ranging from bone augmentations, tilted implants, the use of short implants, and pterygoid or zygomatic implants that can be chosen [ 2, 3].
Recently, a technique wherein trans-sinus placement of implants to fixate in nasal cortical bone in cases where maxillary atrophy may compromise conventional tilted implant insertion was documented [ 4].Malo P et al reported trans-sinus tilted implants gave a cumulative survival rate of 95.7% and 96.4% at patient and implant levels, respectively [ 5]. Another technique placed trans-sinus dental implant by use of bone morphogenetic protein 2 (BMP-2) grafting and immediate functional loading using the all-on-4 treatment method [ 6]. Grandi et al. concluded that there were no statistically significant differences observed between subjects treated with tilted trans-sinus implants without simultaneous bone-grafting or with sinus elevation procedures supporting cross-arch immediately loaded fixed prostheses in atrophic maxillae [ 7].
The aim of the present article is to describe a series of cases where in transsinus placement of implants was done using TTPHIL-ALL-TILT ® in patients with extended anterior and posterior pneumatisation as an alternative to cumbersome sinus lifts. The combined advantages could potentially become a game-changer in rehabilitating atrophied posterior maxilla (Table 1).
| Key Features |
|---|
| Mucointegration—one-time abutment concept |
| Single-drill under preparation |
| Self-drilling active threaded implant for bicortical basal bone engagement |
| Longer implants to engage bi/ multi-cortical plates (16–57 mm) |
| Tilted implants (15–65°) to have more bone-implant contact |
| Rigid splinting with the screw-retained solution for retrievability |
| Platform switching abutment with no micromovement at implant abutment junction |
| Flapless subcrestal placement (pinhole procedure) |
| Immediate prosthesis within 3 days to a week's time |
| Increased primary and secondary stability |
| 20% to 50% greater stress reduction under various loading conditions |
| Economical, safe, and less time-consuming compared to sinus lift procedures |
Ethical principles together with the Declaration of Helsinki were followed while conducting this case series. Written consent from each participant was taken.
2. MATERIALS AND METHODS
Case presentation.
2.1. Case 1: Partially Edentulous (Single Tooth Implant)
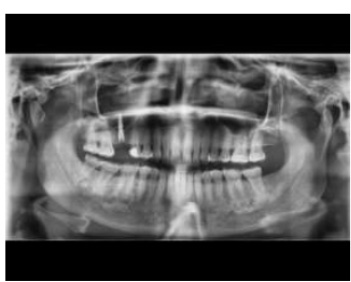
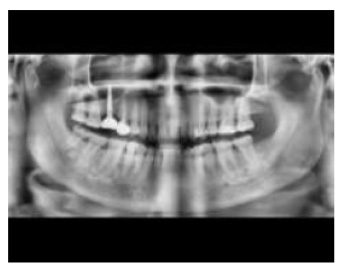
A 52-year-old female patient visited the clinic with the chief complaint of pain and swelling in the upper right back tooth region. Upon clinical examination, it was found that tooth #15 had deep dentinal caries and was tender on percussion and tooth #16 was missing. Her OPG demonstrated pneumatised sinus extending into the missing tooth #16 region such that residual bone height(<8mm) was not adequate for implant placement.
As the patient could not come for multiple visits, it was prudent to provide fixed implant treatment and immediate function without any sinus augmentations to avoid any delay in the completion of treatment. RCT of tooth #15 and trans sinus placement of palato-nasally angulated implant using the TTPHIL ALL TILT ® technique was recommended. After obtaining signed consent for the proposed treatment plan, oral prophylaxis and single sitting RCT were done on tooth #15 followed by an implant placement procedure in the #16 missing tooth region.
2.1.1. Surgical Procedure
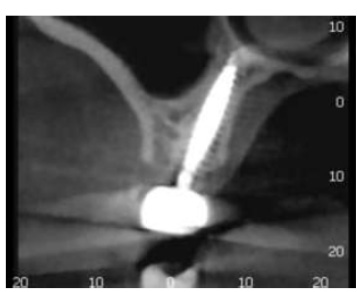
2% lignocaine hydrochloride with adrenaline 1:200000 (Lignox 2%) was administered after obtaining written informed consent. A 1.4mm diameter single drill was used to drill in a flapless manner at the centre of the Bucco-palatal dimension of the implant site at missing tooth #16 region which is the entry point (Fig. 1). The drill was used further along the floor of the maxillary sinus and engaged the cortical bone of the inferior aspect of medial wall of the maxillary sinus. Perforation of Schneider's membrane on the medial-inferior aspect occurred. OPG was taken to confirm the implant position (Fig. 2). The drill was used at a low speed of 400-600rpm for proprioception of cortex engagement. Cone-beam computerized tomography scan was done to confirm the implant angulation in the palato-nasal direction (Fig. 3). Long implants (Bioline I, Bioline Dental GmbH&Co.KG, Berlin, Germany) mounted on implant driverwere driven intothe drilled course until a subcrestal placement of about 3mm was achieved. The apical one-third engaged the medial-inferior maxillary cortical bone and lateral nasal cortical bone (double bi-cortical anchorage) travelling through the medial aspect of the maxillary sinus, thereby the trans-sinus placement of the implant was achieved. Torque and reverse torquing forces of 40Ncm were obtained.

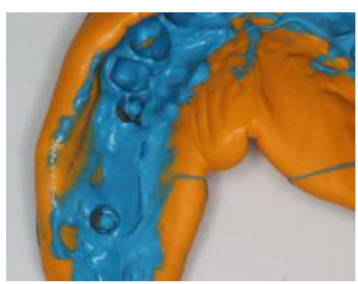
2.1.2. Prosthetic Phase
Implant-level single-stage putty and light body impression (GC Flexseed, GC dental, India) were made using open tray transfer copings. Platform switched 45° angulated abutment was placed on implant analog in the cast to compensate for the implant tilt. The final monolithic zirconia crown was fabricated and cemented on the same day (Fig. 4) and OPG was taken post-placement (Fig. 5). A follow-up of 6 months was uneventful.

2.2. Case 2: Partially Edentulous Maxillary Arch (Implant Supported 3- Unit Bridge)
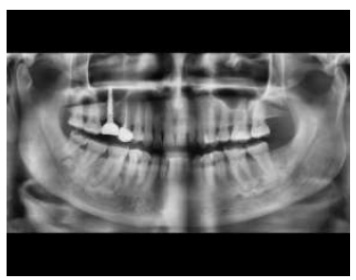
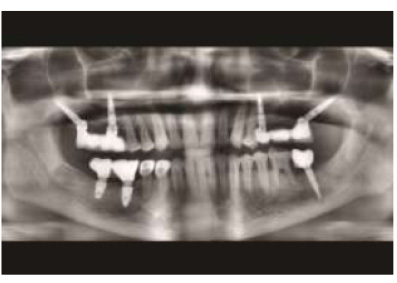
A 59-year-old male patient reported a chief complaint of loose teeth in the upper and lower back region of the jaw. Clinical examination revealed Grade III mobility about tooth 17, 27, and 48, Grade II mobility about tooth 25, gingival recession, missing 16, 26, 37, 46,47, and poor oral hygiene status. The patient was willing to go ahead with a fixed prosthesis for the same region. TTPHIL- ALL TILT ® technique was planned for the same. Radiographic picture and computed tomography suggested moderate bone loss present in the right maxillary sinus region and moderate to severe bone loss in the left maxillary region (Fig. 6).

Considering the amount of bone, for the right maxillary posterior region, atraumatic extraction of 17 followed by the placement of two implants i.e. 16, 17 (pterygoid implant) for implant-supported bridge was planned. Whereas, for the left maxillary posterior region, fixed prosthesis wrt. 25,26,27 removal, atraumatic extraction of 25, 27 followed by the placement of two implants i.e. 25, 27(trans-sinus) for implant-supported bridge were planned. As for the mandible, extraction of 48 followed by placement of two short implants 46, 47 for implant-supported bridge and one single tooth implant corresponding to 37 edentulous region.
Surgery was completed quadrant-wise.
2.2.1. Surgical Procedure for the Trans-sinus Implant
Under aseptic precautions (flapless approach), crestal anesthesia is given at the planned surgical sites. The first anterior implant is placed 3mm behind tooth #24 (entry point at the bone inferior to the antero-medial wall of the maxillary sinus). The drill is used at a low speed of 400-600rpm for proprioception of cortex engagement. The bone available just posterior to the anterior sinus wall and inferior to the sinus floor was used to anchor the implant's head. The antero-inferior maxillary cortical and nasal cortical were used to achieve double bi-cortical anchorage (Fig. 7). Torque and reverse torquing forces of 35Ncm were obtained.
Atraumatic extraction of 27 was performed. Using a physio dispenser speed at 400 rpm, the pilot drill is used next, and after palpation of the hamular process, it is directed 5 mm laterally in the extraction socket at approximately 45° to the occlusal plane (Fig. 8). The single stepped drill first encountered the posterior aspect of cortical bone of the posterior wall of the sinus, passes through the sinus and then engages the cortical bone of the posterior wall of the maxillary sinus and finally upto the pterygomaxillary junction (Fig. 9). The implant is now driven slowly using the implant mount with a long handle until the subcrestal placement is achieved (Fig. 10). Torque and reverse torquing forces of 35Ncm were obtained.


2.2.2. Prosthetic phase
Multiunit abutments (30° and 45°) are then placed at the correct angulations to compensate for the tilt of the implants (Fig. 11). The surgical phase is followed by the prosthetic phase- Impression making (Fig. 12), metal framework trial, Bisque trial followed by placement of final prosthesis which was made using computer aided design and computer aided manufacturing (CAD CAM) technology for designwithin 2–5 days (Fig. 13). Post-placement orthopantomogram is taken (Fig. 14). The patient was followed up at 6 months.


2.3. Case 3: Completely Edentulous Maxillary Arch (Implant Supported)
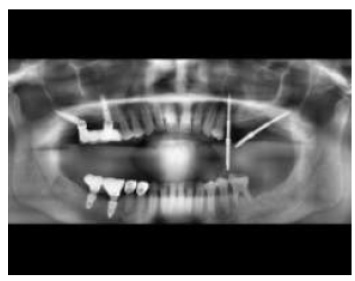
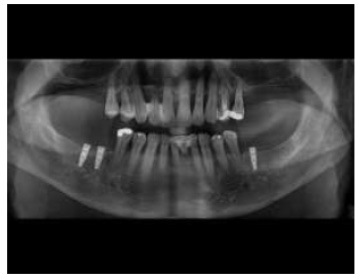
A 61-year-old male patient complained of missing upper back teeth and lower back teeth. Intraoral examination revealed Miller's class IV recession and grade 3 mobility in all the remaining maxillary teeth and grade 1 mobility in the remaining mandibular tooth (Fig. 15). Medical history revealed diabetes and insulin-dependent. On detailed radiographic examination, there appeared severe bone loss and inadequate bone in the maxillary sinus region (Fig. 16). Treatment plan for the maxilla was immediate implant placement in 13, 15(Trans-sinus), 17 (Pterygoid implant/ Trans-sinus), 23, 25, 27 (Pterygoidimplant/Trans-sinus) tooth region and for mandible implant placement in 36,37, 46, 47 tooth region followed by implant retained prosthesis. Routine blood investigations were performed and the physician’s fitness for the surgical procedure was acquired.


2.3.1. Surgical Procedure for the Trans-sinus Implants
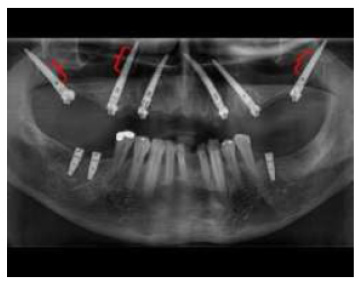
Atraumatic extraction of 13,14,15 was performed under local anaesthesia. An anterior fixture was placed to the anterior wall of the maxillary sinus from distal to a mesial direction towards the nasal cortex in the first quadrant. Using a surgical guide, a pilot drill of 1.2 mm was positioned through the mucosa into the alveolar bone up to 6 mm depth. Radiovisiographic Image (RVG) (Carestream, Kodak, India) was taken to confirm 300 tilt to the occlusal plane. Then, a 1.4 mm diameter single drill was used to drill through the template at a low speed of 400-600 rpm for proprioception of nasal cortex engagement. A 3.5×18 mm tapered implant mounted on an implant driver was driven into the drilled course. A 40Ncm torque and reverse torquing forces were obtained using a torque rachet. A confirmative RVG was taken. The second implant (3.5×18 mm) was placed using the same protocol at 15 extraction site parallel to the first implant in distal to a mesial direction at 45 0 to occlusal plane (Fig. 17). Perforation of Schneider's membrane on the medial-inferior aspect occurred. The drill is used at a low speed of 400-600rpm for proprioception of cortex engagement. The bone available posterior to the anterior sinus wall and inferior to the sinus floor was used for anchoring the implant's head. The apical two-thirds engaged the anterio-inferior maxillary cortical bone and anterio-superior maxillary cortical bone travelling through the anterior aspect of the maxillary sinus. The antero-inferior and superior maxillary cortical was used to achieve double bi-cortical anchorage. Torque and reverse torquing forces of 35Ncm were obtained.

Under aseptic precautions (flapless approach), crestal anesthesia is given at the surgical site. A pterygoid instrument is inserted and a check RVG is taken to confirm the point of entry (junction of the floor and posterior wall of maxillary sinus) and the initial path. Using a physio dispenser speed at 400 rpm, the pilot drill is used next, and after palpation of the hamular process, it is directed 5 mm laterally at approximately 45° to the occlusal plane. This process is a guide to identify the thickest part of the pterygoid pillar of the bone. The single-stepped drill first encountered the posterior aspect of cortical bone of the posterio-inferior wall of the sinus, passes through the sinus, and then engages the cortical bone of the posterior wall of the maxillary sinus and finally up to the pterygomaxillary junction. Just after crossing the maxillary sinus posteriorly, the drill is stopped. A depth gauge is again used and a check X-ray is taken to finalize the length of the implant and to ensure its path. The implant is now driven slowly using the implant mount with a long handle until the subcrestal placement is achieved. The pterygoid implant was diagonally inserted superiorly, posteriorly, and distally, towards the pterygopalatine fossa of the sphenoid bone. Torque and reverse torquing forces of 35Ncm were obtained.
The same protocol is followed in the second quadrant after extraction of 11,21, 22, 23, 24, and 25 (Fig. 18), except the implant in the 25 extraction site is not placed in a trans-sinus manner but merely tilted in a palato-nasal direction to engage nasal cortex (Fig. 19).

2.3.2. Prosthetic phase
Multiunit abutments (30°, 40°, and 50°) are then placed at the correct angulations to compensate for the tilt of the implants (Fig. 20). Impression-making with transfer copings, Jig trial (Fig. 21), bite records, metal framework trial, bisque trial followed by placement of final prosthesis made using computer-aided design and computer-aided manufacturing (CAD /CAM) technology for design (Fig. 22), and fabrication within 2–5 days. Post-placement orthopantomogram is taken (Fig. 23). Follow-up of the patient is done at 6 months.




3. RESULTS
Post-surgical instructions were given to all patients. Amoxicillin- 2 g along with clavulanic acid was administered preoperatively, 1 g twice daily for 6 days thereafter. Ibuprofen (600 mg) was prescribed immediately after surgery together with 4 mg of betamethasone. A cold/soft diet and appropriate oral hygiene were recommended for 2 weeks.
In all cases, postoperative recovery was uneventful: soft tissues healed well and no signs of inflammation were present. Implants and implant retained prosthesis remained immobile on monthly follow-up till 6 months inferring that the implants were clinically stable. Implants were also assessed radiographically and none of the patients showed undue marginal bone loss (Figs. 24-26). No pathological symptoms or signs (implant mobility, peri-implant probing depth, or peri-implant bleeding on probing) were recovered at any follow-up visit for each implant.


4. DISCUSSION
A few studies on trans-sinus implant placement in patients with atrophic maxilla exist as well as a few other studies for the use of TTPHIL-ALL-TILT ® treatment protocol for rehabilitating edentulous atrophic maxilla exist. To the authors’ knowledge, this is the first case series for rehabilitating patients with extended anterior and posterior pneumatised or atrophied maxilla; where the concept of trans-sinus implant placement and TTPHIL-ALL-TILT ® treatment protocol has been used simultaneously without the use of other reconstruction techniques (such as bone grafting and/or sinus lift). The current case series describes such cases with three different combinations of edentulous states to suggest the versatility of this procedure.
Because of the presence of extended maxillary sinus pneumatisation and osseous quality in the above case scenarios, a combination of trans-sinus implant placement and TTPHIL technique was used to obtain double bicortical anchorage from nasal fossae, the anterior wall of the maxillary sinus and pterygomaxillary region minimising micro-movements; thereby, helping in better primary stabilisation [ 3, 8]. The cortical engagement was possible due to longer, tilted implants. From a biomechanical perspective, the anterio-posterior spread of implants provided favourable inter-implant distance [ 10], increased bone-implant contact area, eliminated cantilever, and consequently lead to efficient load distribution. Complete cantilever elimination can be attributed to the engagement of the pterygoid cortex which compensated for poor osseous structure [ 11]. From a clinical point of view, the technique fulfilled the requirement for immediate functional loading of implants by achieving high primary stability [ 12]. Moreover, the technique eliminated the use of cumbersome procedures of placing grafts, bypassed vital structures, and reduced overall treatment costs.
A healthy peri-implant mucosal barrier is essential for the stability and function of loaded implants. Reduction in postoperative pain, swelling, intraoperative bleeding, surgical time, soft and hard tissue preservation, and maintenance of blood supply are some advantages of the flapless technique [ 13]. Yamada et al., concluded that flapless guided surgery for immediately loaded fixtures depicted predictable outcomes and a high implant survival rate in the edentulous maxilla [ 14]. Additionally, Martinez et al., demonstrated that combining flapless surgery and subcrestal implant placement aids in the preservation of the crestal bone and increased osseointegration [ 15]. Subcrestal implant placement compensated for the predictable bone loss by allowing bone to regenerate and soft tissue growth of 1mm. Additionally, it facilitated osseointegration to the abutment surface and minimised thread exposure by the formation of marginal tissue architecture enhancing aesthetic outcome [ 16].
Densification of peri-implant bone is crucial for immediate functional loading in type-3 osseous bone quality because it provides improved primary stability, bone-implant contact area, and osseointegration. Drill surface causes peripheral compaction of bone chips and debris through “osseodensification” . The usage of a single osteotomy drill reduced temperature and improved vascularization favouring bone regeneration [ 17]. Implant threads helped engage surrounding bone causing lateral condensation of spongy bone through “corticalisation” [ 18]. One stage, flapless surgery, single drill, subcrestal placement, and double bi-cortical bone fixation and a few other features of this combined technique of trans-sinus implant and TTPHIL-ALL-TILT ® treatment protocol allowed delivery of immediately loaded provisional fixed prosthesis by facilitating and maintaining mucosal integration.
To improve biomechanical efficiency, previous studies have advocated the use of only trans-sinus implants, zygomatic implants, or the TTPHIL technique, all separately. But, these techniques cannot completely eliminate cantilevers. Employing zygomatic implants can be invasive, technique sensitive, and limited by the anatomy of zygomatic bone [ 19].
The authors recommend the use of trans-sinus implants with TTPHIL-ALL-TILT ® treatment protocol as an alternative technique when it is not possible to rehabilitate the completely edentulous posterior maxillae with conventional treatment options like tilted implants and to be considered before choosing more complex options such as zygomatic implants or sinus lift/bone grafting procedures. Some guidelines suggested by the authors through this case series include making sure that the implant apex firmly engages a cortical bone and does not stay protruded in the sinus cavity. This would help in reducing micromovements at the apex and irritation in the sinus lining. The apical third being engaged at two cortical walls will be highly stable and the surface of the implant in between which is exposed to the sinus would just be covered with debris. It was reported in a systematic review conducted by G M Ragucci, et al. that the long-term consequences of debris accumulation over the implants extended inside the maxillary sinus and perforating the Schneiderian membrane have not been systematically evaluated before [ 20]. However, Jung et al. observed in a dog-mongrel study that after 6 months of follow-up, when dental implants were placed with the maxillary sinus perforation, the mucosa in the maxillary sinus cavity showed no inflammatory signs. This study concluded that the extending implants do not make the maxillary sinus vulnerable to complications and do not cause any effect on the sinus physiology resulting in no local or systemic pathology at all [ 21]. Additionally, in one of the latest studies conducted by Malo et. al. with a 3-year follow-up, sinusitis was observed in 2 out of 80 patients with a prevalence rate of 2.9%. It was observed that the prevalence rate was comparatively lower as compared to the prevalence reported in rehabilitation of the atrophic maxilla through zygomatic implants, in which this complication is one of the most prevalent, and yet it's possibly underestimated since most studies do not mention the presence or absence of these complications [ 5].
The outcome of the present case series was similar on 6 months follow-up, as rupturing the sinus membrane in the absence of preoperative sinusitis did not seem to influence significantly the prevalence of sinus infections. Nevertheless, the combined use of these two techniques in more patients and long-term clinical and radiographic follow-up is needed for better validation of the technique. Future randomised controlled trials should focus on the long-term outcome of this rehabilitation technique when compared to alternative techniques.
CONCLUSION
The presented technique eliminated the cantilever and provide improved implant stability for maxillary rehabilitation and was able to improve clinical ease, patient acceptance, and chewing efficiency. The patient was satisfied with the implants and prosthesis and demonstrated good healing leading to the overall success of the implants and prosthesis. By harnessing the benefits of a variety of concepts in implantology, these two techniques combined has been successful in providing these three patients and clinician a more organised and efficient treatment option for rehabilitating severely atrophied maxilla. More thorough, long-term research is required to prove whether this could universally replace the established protocols for rehabilitating atrophied posterior maxilla.
LIST OF ABBREVIATIONS
| OPG | = Orthopantomogram |
| CBCT | = Cone Beam Computed Tomography |
| TTPHIL | = Tall Tilted Pin Hole Immediately Loaded |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Institute for dental Implantology, Hyderabad, India.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available in the Zenodo Repositary at https://zenodo.org/, reference number 8285685.
ACKNOWLEDGEMENTS
Declared none.


