All published articles of this journal are available on ScienceDirect.
Characterization of Dentures for a Natural Esthetic Result: A Case Report
Abstract
Background:
Dental implants offer many viable clinical solutions, but there are patients when they cannot be chosen as the optimal plan. Conventional removable prostheses still come up as a functional option, and several techniques have been developed so that their appearance can be esthetically enhanced and, in certain circumstances, even customized.
Case report:
This paper presents a clinical case where new conventional dentures were manufactured for both jaws. The patient was complaining about the “artificial” appearance of the pre-existing restorations and was also diagnosed with depression, which was an extra challenge to be dealt with. Attention was also given to individualizing the esthetic performance utilizing materials and techniques for the characterization and customization of the dentures for a natural-like result, in accordance with all the clinical factors that influence the restoration in edentulous patients.
Conclusion:
As shown in the presented case, complete dentures remain a viable treatment plan. Especially via the process of characterization and customization, higher patient satisfaction and easier acceptance can be achieved.
1. INTRODUCTION
Dental implants constitute a viable and, for many patients, a desired treatment plan. Yet, there are situations when they cannot be suggested or performed for medical records, economic reasons, or even due to lack of dental care [1]. Conventional removable dentures remain a vital option, and the need as a treatment solution will continue to exist either as an interim prosthesis before the sequence of implant-supported restorations or as the final treatment [1]. Nowadays, esthetic demands and patient awareness of dental esthetics have increased, including edentulous patients [2]. A patient’s acceptance of the removable prosthesis is highly dependent on the restoration's appearance, which is a common reason for their discontent over the lack of natural-looking teeth [2]. For these reasons, adequate time should be dedicated to understanding the patient’s perception of appearance and scrutinizing any available data regarding their natural teeth, such as photographs or even mold casts [3].
Studies deriving from different populations suggest that many existing dentures are not in appropriate conditions and therefore require replacement [4]. Literature includes several reports and methods that could achieve a natural-looking restoration. The clinician and the dental technician are responsible for combining the individualized esthetic appearance and the aging process while considering basic biological principles and established guidelines [3]. Flanges play a significant role in the esthetic outcome via their morphology, color appearance, and texture; therefore, different characterization techniques can serve in this direction.
1.1. Aim
This case report aims to present the clinical and laboratory process steps that took place in order to characterize the teeth and bases in complete dentures for a better esthetic result. The workflow followed was conventional, and the materials included high-impact polymer for the denture bases, PMMA artificial teeth, and light-curing resins to characterize the restorations.
2. CASE REPORT
A 54-year-old Caucasian female patient was referred to the Graduate Prosthodontics Clinic, Department of Prosthodontics, University of Athens. Her chief complaint was the appearance of her existing restorations, mentioning that she feels embarrassed to smile or speak even in front of her closest family members. Due to improper palatal seal, the existing maxillary denture had underextented flanges, insufficient border molding, and reduced retention and stability (Fig. 1). The mandible was restored with a removable partial denture without a metal framework and clasps. As the patient reported, the clinical and laboratory processes were accomplished by a dental technician without the involvement of a dentist.

A detailed clinical examination of the dentures related to the patient’s main esthetic concerns revealed the following:
- The existing denture teeth were esthetically compromised in both shape and arrangement.
- The teeth lacked any lifelike appearance since their color was uniform, “dull,” and opaque.
- The cervical part of the artificial teeth did not have any translucency.
- The morphology, texture, and color appearance of the denture flanges enhanced the esthetic failure.
- The lips and soft tissues were not adequately supported.
For the abovementioned reasons and following a proper radiographic examination, a new denture was fabricated for the maxilla. The mandible's two remaining premolars had a poor prognosis due to minimal remaining osseous support and root caries. They were decided to be extracted, and a new complete denture would follow.
As the patient herself revealed, she was diagnosed with depression, and one of the reasons aggravating her condition was the esthetic appearance of her mouth. To improve the elements, a characterization technique was decided for the laboratory steps and the so-called “pink esthetics.”
Therefore, 6 weeks after the extraction of the remaining teeth, a maxillary and mandibular impression was taken, utilizing a two-step technique with zinc-oxide and eugenol paste as well as border molding using custom trays. The impressions were then sent to the dental laboratory to fabricate working casts.
The interarch relationship was recorded with bimanual manipulation using base plates and polyvinylsiloxane. This is a significant clinical step for the orientation and accuracy of the prosthetic space.
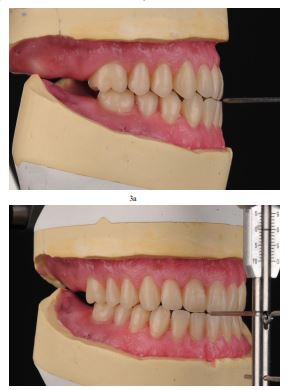
Due to skeletal Class III relation (Fig. 2), it was preferred to set up the teeth in an edge-to-edge position with no horizontal or vertical overlap (Fig. 3a and b). By the intraoral try-in, the patient was satisfied with the planned result and reported that they were identical to her previously existing natural teeth.

The prefabricated denture teeth were chosen to be out of PMMA, with a diagonal grid structure, to enhance the density and hardness of the surface (Tribos 501, Gebdi DENTAL-PRODUCTS GmbH, Germany). They were slightly reshaped by grinding the incisal edges and proximal points to match the patient sex and age. The occlusal scheme was decided to be lingualized occlusion. The modified artificial teeth were arranged in the desired occlusal plane and evaluated intraorally. One of the main concerns at this stage was to achieve an esthetically pleasing composition per the formation of proper buccal corridors for a more natural smile line. The process of mimicking the natural color of the gingival tissues was supported by transferring a detailed color prescription of the natural intraoral tissues to the laboratory utilizing pink shade tabs and standardized photographic documentation.
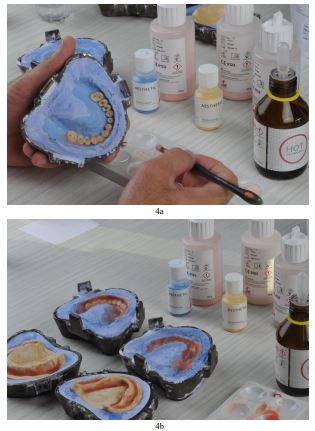
The laboratory processing of the prostheses followed in the conventional manner (Xplex high-impact polymer, Candulor Dental GmbH, Germany). After deflasking, a surface layer of the labial flanges was grinded and then sandblasted in order to enhance the adhesion of the new composite layers and extrinsic color agents. An additional primer was used to coat the modified surface of the restorations, and light-cured composite resins were distributed utilizing the incremental layering technique. To mimic the area of the “attached tissue,” a light pink shade without fibers was selected, combined with a fibered, slightly reddish pink color layer at the “mucosal part.” The surface texture is also important for esthetic improvement. Thus, color variations were chosen for the cervical areas of the artificial teeth with smooth transitions reproduced in the flanges of both dentures in order to improve appearance by simulating root eminences, small blood vessels, and soft-tissue topography (Aesthetic Color Set Easy, Candulor Dental GmbH, Germany). A visible light-curing device was used afterward to photopolymerize the prostheses per the manufacturer’s instructions (Fig. 4a and b).
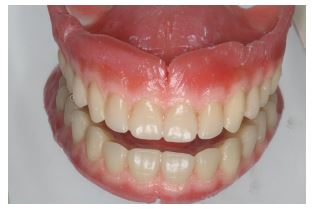
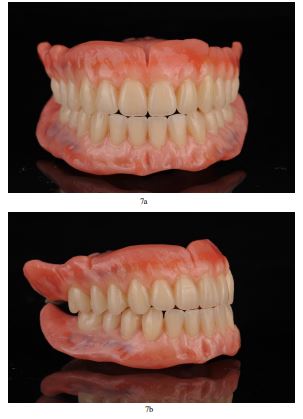
The newly fabricated restorations were coated with high-gloss polishing varnish and subjected to a final photopolymerization stage in the curing unit (Figs. 5 and 6) The comparison between pre-existing and new dentures clearly indicates the esthetic differences. After a final intraoral evaluation and some minor adjustments, the prostheses were delivered to the patient, who was satisfied both with function and esthetics (Figs. 7a and b, 8a and b). The 2-year follow-up also enhances these encouraging results, and the patient herself mentions the psychological improvement thanks to the prosthodontic rehabilitation.

3. DISCUSSION
In contemporary Prosthodontics, complete edentulism remains a challenge, especially in esthetically compromised cases where the patient might have lost self-confidence and trust in the clinician. Complete dentures as a rehabilitation solution are known to improve health-related and oral health-related quality of life and are, thus, a significant part of offering to our patients [5]. It is interesting that of all the factors studied, patient satisfaction was found to be the strongest predictor of oral health-related quality of life and is consequently useful in assessing it [6].
When complete dentures are the selected treatment plan, there is always the probability that after delivering them, the patient might encounter difficulties adapting to them. One of the main reasons is psychological factors. More specifically, fear, anxiety, and, most importantly, depression, along with the recommendation that the last remaining teeth should better be extracted, can lead to emotional turmoil and absence of adaptation [7]. Patients who have lost all or most of their natural dentition -due to poor dental treatment- often feel guilty, as if it was “their fault,” which may not always be the case [8]. Furthermore, there is a correlation between chewing problems and impairments in oral-health-related quality of life. More specifically, chewing difficulties have been associated as a causal factor for depression [9].
Therefore, it is of utmost importance to follow all the rules concerning achieving sufficient stability and retention so that the patient can benefit from the clinical application of the prosthesis without having to deal with drawbacks in function or social activities. After all, despite the progress in Implantology, there are still cases when conventional dentures offer the optimal solution [3]. Apart from these, esthetic appearance always plays a vital role in the better acceptance of the restoration by the patient. There are cases where the prosthesis's artificial and esthetically compromised outcome was the main reason for complaint. From a psychological aspect, the patient may feel overwhelmed and fear possibly being recognized as edentulous or socially embarrassed; they may reject it and become isolated [7]. It is, thus, a sound practice not to continue with the processing and finishing of the removable prosthesis until the patient, unpressured and after enough time, mentions absolute satisfaction with the esthetics [8].

Natural-looking restorations are more easily acceptable, and individualized appearance seems to be appreciated by the patient since it blends harmonically with the other facial characteristics [10]. Therefore, this constitutes one of the main strong points of the selected treatment plan. In addition to that, it is an affordable solution, especially in comparison to implant-assisted prostheses. Unfortunately, these techniques are not often included in daily-routine practices, which is one of the main limitations of this case report, probably due to a lack of relative awareness or because special techniques, materials, and, thus, money and extra time may be needed [11]. Nonetheless, in more complex cases like the present one, mainly due to the medical record, it is a very helpful instrument for better adaption and psychological enhancement.
Other authors have reported different characterization methods, including customized elements on the teeth like amalgam fillings, cervical erosions, or artificial smoking stains to enhance the smile's natural appearance [3, 12]. New techniques and materials are expected to further improve the esthetic result of complete dentures.
CONCLUSION
Even in esthetically compromised cases where the patient might have lost their self-confidence and trust towards the clinician, conventional dentures are a reliable rehabilitation solution and improve health-related and oral health-related quality of life. The “mucosal part” of the prosthesis is as important as the teeth in mimicking natural appearance, while its customization can enhance patient satisfaction and acceptance.
ABBREVIATION
| PMMA | = Poly(methyl methacrylate) |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The patient’s consent form is attached in an extra file in the Greek language.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
Informed consent was obtained from the patient for treatment and publication (attached file in Greek).
ACKNOWLEDGEMENTS
The authors want to thank K. Iliopoulos (CDT) for his precious help in the laboratory stages of denture fabrication.


