Evaluation of Oral Dryness and the Salivary-flow Rate in Patients with Oral Lichen Planus
Abstract
Background and Objectives:
Oral lichen planus (OLP) is a common T-cell-mediated inflammatory oral mucosal disease. One of the complaints among OLP patients is xerostomia. However, the relationship between oral dryness and a decreased salivary-flow rate in these patients is not yet conclusive. So, we investigated oral dryness and the salivary-flow rate in OLP patients using various measurements.
Material and Methods:
Thirty OLP patients and 30 controls were included. The oral-dryness symptoms were collected using the Xerostomia Inventory (XI) and Bother Index (BI). The salivary-flow rate was measured using a Modified Schirmer Test (MST) and the spitting method. The clinical signs of dry mouth were determined by the clinical oral-dryness score (CODS). The Thongprasom score was used to evaluate the severity of OLP. The data were analyzed using the Mann-Whitney U test and Spearman’s rank correlation coefficient.
Results:
The XI score and BI score in the OLP group were significantly higher than in the control group. However, CODS, MST, the unstimulated salivary-flow rate, and the stimulated salivary-flow rate were not significantly different between the two groups. There was no correlation between oral dryness and the salivary-flow rate in OLP patients. The severity of OLP was also not correlated to oral dryness and the salivary-flow rate.
Conclusion:
OLP patients had more complaints about mouth dryness than the controls. However, the salivary-flow rates between the two groups were not different. Additionally, the severity of OLP was not related to dry mouth or the salivary-flow rate. The possible reasons for oral dryness among people with OLP require further investigation.
1. INTRODUCTION
Oral lichen planus (OLP) is a common chronic inflammatory disease. It affects 0.5-2% of the population. The disease is found to be more prevalent in women than men, at a ratio of 4:1. The T-cell-mediated immune system is believed to be involved in the pathogenesis of OLP [1, 2]. The three major clinical presentations of OLP consist of the reticular, atrophic, and erosive forms. Patients with the reticular form are frequently asymptomatic. However, patients with the atrophic
or erosive forms usually report roughness in their mouth, a burning sensation, and painful oral mucosa [1-3]. In symptomatic OLP patients, their quality of life is usually affected.
Xerostomia is one of the complaints reported by OLP patients [3, 4]. The relationship between OLP and persistent dry mouth has been reported. Using a modified Xerostomia Inventory, Colquhoun and Ferguson showed that OLP patients had more severe oral dryness than the control group [5]. Other studies have also reported that OLP patients had a higher Xerostomia Inventory (XI) score than the controls [6, 7].
Salivary gland hypofunction is often the cause of xerostomia [8]. Previous studies have shown that OLP patients with more oral-dryness symptoms had a lower salivary-flow rate than the controls. They reported that the unstimulated and stimulated salivary-flow rates among OLP patients were statistically significantly lower than among the controls [6, 7]. Another study reported that 34 (87%) of 39 OLP patients exhibited a low or very low unstimulated salivary-flow rate. Labial salivary gland biopsies also revealed acinar atrophy and chronic inflammatory cell infiltration in 14 (93%) and 12 (80%) of the 15 OLP patients [9]. These results suggest that dry mouth among OLP patients is related to hyposalivation.
In contrast, Artico et al. revealed that the prevalence of oral dryness and hyposalivation in the OLP group, non-OLP group (patients with leukoplakia, traumatic keratosis, and discoid lupus erythematosus), and the control group were not statistically significantly different [10]. Larsen et al. also found that the salivary-flow rate of OLP patients with the dry mouth was not different from that among the controls [11]. Therefore, whether there is an association between oral dryness and hyposalivation among OLP patients remains inconclusive.
In this study, we aimed to investigate oral-dryness conditions and the salivary-flow rates in patients with OLP compared to those in the control group using various measurements in dentistry. Additionally, we studied the correlations among oral dryness, the salivary-flow rate, and the OLP-severity score in the OLP group. The results of our study can help dental professionals be more aware of xerostomia in OLP patients and lead to better management of the disease.
2. MATERIALS AND METHODS
2.1. Study Participants
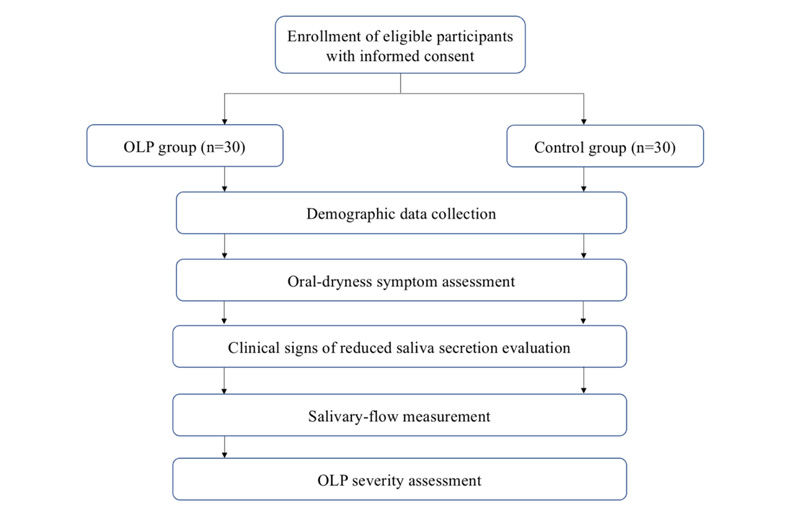
Data were collected from 30 OLP patients and 30 controls who visited the Faculty of Dentistry at Srinakharinwirot University in Bangkok from 2020-2021. The study was approved by the Srinakharinwirot University Ethics Committee (no. SWUEC/E-464/2563). All the participants were informed and gave written consent prior to the beginning of the study. Fig. (1) shows the flow chart of the study protocol. In the OLP group, the inclusion criteria were: being 20 years or older; having a confirmed diagnosis of OLP by clinical and histopathologic presentations according to the World Health Organization (WHO) criteria [12]; had not used corticosteroids or stopped using topical corticosteroids and systemic corticosteroids for at least two weeks and four weeks prior to data collection, respectively. The controls included patients who had no oral lesions and were 20 years or older. The exclusion criteria for both groups were people who had diabetes mellitus, autoimmune diseases, graft-versus-host disease, chronic kidney disease, and/or had used medication-induced hyposalivation such as hypertensive drugs, antidepressants, anxiolytics, bronchodilators, and decongestants. People who had oral candidiasis, a history of head and neck radiation and smoking were also excluded.
The demographic and clinical data consisting of age, sex, systemic diseases, and current medications were collected from all participants.
2.2. Oral-dryness Symptom Assessment
Subjective feelings of oral dryness were evaluated by using the Xerostomia Inventory (XI). This questionnaire consisted of 11 items. Each participant was asked to rate each item from 0-5 (score 1 = never; 2 = hardly; 3 = occasionally; 4 = fairly often; and 5 = very often) [13]. The scores on the 11 items were added to create a total XI score ranging from 11 (no xerostomia) to 55 (extreme xerostomia). The Bother Index (BI) was also used to determine the severity of oral dryness. A self-rated score ranged from 0-10, with 0 representing no burden and 10 representing the most trouble [14].
2.3. Salivary-flow Measurement
One examiner conducted the collection of saliva (VA). The assessment was made between 9:00 a.m. and 12:00 p.m. to minimize the effects of the circadian rhythm. The participants were instructed to refrain from eating, drinking, brushing their teeth, and using mouthwash for 60 minutes prior to the salivary measurement. They were asked to sit upright, swallow once to clear the residual saliva in their mouth, and not to swallow during the test [15, 16].
Unstimulated whole saliva (UWS) and paraffin-chewing-stimulated whole saliva (SWS) were collected via spitting. The participants were instructed to collect saliva in their mouths and spit it into the pre-weighed container. For SWS, the participants were asked to chew a paraffin-size 5x5 cm2 and expectorate into the pre-weighed container. After the collection, both the UWS and SWS containers were reweighed. The collected volume was deducted from the weight of the container prior to collection. The salivary-flow rates were calculated by dividing the collected volume (assuming 1 g. of saliva equals 1 ml.) by the collection time (min), and the results were presented in ml/min. Hyposalivation was defined when the UWS was valued at < 0.1 ml and SWS was valued at < 0.5 ml/min [8].
The Modified Schirmer test (MST) was also used to determine the unstimulated salivary-flow rate. The test strip was a 4-cm-long filter paper strip with a 1-mm scale interval from 5-35 mm along its length. The participants were asked to lean backward, swallow once to clear the residual saliva in their mouth, and not to swallow during the test. Moreover, they were asked to rest their tongue on their palate so the test strip would not touch their tongue. The test strip was held vertically with a cotton plier and the end of the strip was placed on the floor of the mouth on the right or left of the lingual frenum. When the strip contacted the moisture, the strip was wet and was recorded at 1, 2, and 3 minutes. The strip was removed for 2-3 seconds for reading [17]. The measurements ranged from 5-35 mm. When the measurement was less than 5 mm, 5 mm was recorded, and when it was higher than 35 mm, 35 mm was recorded [18]. Hyposalivation was assessed if the distance was < 25 mm at 3 min [17].
2.4. Oral Examination
One examiner did the oral examination for all the participants (VA). Clinical signs of reduced saliva secretion were evaluated using the clinical oral-dryness score (CODS). CODS is a 10-point scale in which each point represents a clinical feature of oral dryness [14, 19]. The total CODS was calculated by adding the scores from these features. A high total score specified more severe dryness.
Regarding OLP, the location, size, and duration of the oral lesions were recorded. The OLP severity was evaluated according to the Thongprasom score as follows: 0 = normal mucosa; 1 = lesions with only white striae; 2 = mixed keratotic and atrophic or erythematous lesions smaller than 1 cm2; 3 = mixed keratotic and atrophic or erythematous lesions larger than 1 cm2; 4 = erosive/ulcerative lesions smaller than 1 cm2; and 5 = erosive/ulcerative lesions larger than 1 cm2 [20].
2.5. Statistical Analysis
The statistical analysis was done using SPSS software, Version 25 (SPSS Inc, Chicago, IL, USA) for Windows. The difference in mean age between the two groups was compared by using the independent t-test. Sex and systemic diseases were compared using the Chi-square. The XI score, BI score, CODS, and salivary-flow rates were not normally distributed. Thus, the Mann-Whitney U test was used for the comparisons. The correlation between the variables was calculated by using Spearman’s rank coefficient correlation. The statistical significance was defined as a p-value of < 0.05.
3. RESULTS
3.1. Demographic Data and Clinical Presentation of the Study Populations
The participants in each group consisted of 25 women (83.3%) and 5 men (16.7%). The mean age of the OLP group and control group were 54.37 ± 13.05 years old and 54.77 ± 13.73 years old, respectively. There was no statistically significant difference in age and sex between the two groups (p > 0.05) (Table 1). Eight (26.7%) of the 30 OLP patients had systemic diseases, including thyroid disease (6.67%), followed by allergic rhinitis (3.33%), migraines (3.33%), seizures (3.33%), gastroesophageal reflux disease (3.33%), thalassemia (3.33%), and benign prostatic hyperplasia (3.33%). Four patients were taking medications that consisted of propylthiouracil (n=2), lamotrigine (n=1), and folic acid (n=1). In the control group, four patients (13.33%) had systemic diseases, including dyslipidemia (6.67%), thyroid disease (3.33%), and arrhythmia (3.33%). Two patients were taking simvastatin and one person was taking propylthiouracil.
Most OLP patients presented with the atrophic form (80%), followed by the erosive form (20%). The OLP severity scores were 2 (26.7%), followed by 3 (53.3%), 4 (10%), and 5 (10%). Sixteen patients (53.3%) had oral lesions at multiple sites. The most common site was the buccal mucosa (93.3%), followed by the gingiva (60%), tongue (26.7%), lip (10%), soft palate (3.3%), and the floor of the mouth (3.3%). About 53.3% had oral lesions for 1-5 years, 40% for more than 5 years, and 6.7% for less than 1 year (Table 1).
3.2. Oral Dryness and Salivary Flow-rate Assessment
The mean XI score of the OLP and controls were 21.33 ± 6.69 and 17.70 ± 6.40, respectively. The mean BI score was 2.35 ± 2.25 in the OLP group and 1.18 ± 1.50 in the control group. Both the XI and BI scores among the OLP patients were statistically significantly higher than among the controls (p < 0.05) (Table 2).
| Variables | OLP group (n=30) |
Control group (n=30) |
P-value |
|---|---|---|---|
| Sex (no., %) · Male · Female |
5 (16.7%) 25 (83.3%) |
5 (16.7%) 25 (83.3%) |
1.000 |
| Age (years) · Mean ± S.D. · Range |
54.37 ± 13.05 22-76 |
54.77 ± 13.73 21-77 |
0.908 |
| Systemic diseases (no., %) · No · Yes |
22 (73.3%) 8 (26.7%) |
26 (86.7%) 4 (13.3%) |
0.197 |
| Thongprasom score (no., %) · Score 1 · Score 2 · Score 3 · Score 4 · Score 5 |
0 (0%) 8 (26.7%) 16 (53.3%) 3 (10%) 3 (10%) |
- - - - - |
|
| Location of oral lesions* (no., %) · Buccal mucosa · Gingiva · Tongue · Lip · Soft palate · Floor of the mouth |
28 (93.3%) 18 (60%) 8 (26.7%) 3 (10%) 1 (3.3%) 1 (3.3%) |
- - - - - - |
|
| Duration of oral lesion (no., %) · < 1 year · 1-5 years · > 5 years |
2 (6.7%) 16 (53.3%) 12 (40.0%) |
- - - |
| Variables | OLP group | Control Group | P-value |
|---|---|---|---|
| XI score | 21.33 ± 6.69 | 17.70 ± 6.40 | 0.018* |
| BI score | 2.35 ± 2.25 | 1.18 ± 1.50 | 0.023* |
| Spitting method · UWS (ml/min) · SWS (ml/min) |
0.58 ± 0.45 1.21 ± 0.63 |
0.78 ± 0.53 1.43 ± 1.04 |
0.086 0.333 |
| MST · at 1 min. (mm) · at 2 min. (mm) · at 3 min. (mm) |
10.73 ± 6.19 17.80 ± 8.98 24.47 ± 8.76 |
13.20 ± 5.70 20.83 ± 8.23 26.83 ± 8.38 |
0.121 0.193 0.328 |
The UWS was 0.58 ± 0.45 and 0.78 ± 0.53 ml/min in the OLP and controls, respectively. The SWS was 1.21 ± 0.63 ml/min in the OLP and 1.43 ± 1.04 ml/min in the controls. Using MST, the UWS in the OLP group was lower than among the controls at all time points. However, the two groups had no statistically significant differences in the UWS, SWS, and MST (p > 0.05) (Table 2).
Clinical signs of dry mouth based on CODS were found in 14 OLP patients (46.67%) and 9 controls (30%). The CODS ranged from 0-2 in both groups. The mean CODS in the OLP group and control group were 0.57 ± 0.68 and 0.37 ± 0.61, respectively. When compared to the controls, the OLP group had higher CODS, although this was not at a statistically significant rate (p > 0.05) (Table 3).
| Variables | Study Populations | P-value | |
|---|---|---|---|
| OLP Group (n=30) |
Control Group (n=30) |
||
| CODS | 0.57 ± 0.68 | 0.37 ± 0.61 | 0.200 |
| Clinical signs based on CODS* (no., %) · Yes · The mouth mirror sticks to the buccal mucosa · The mouth mirror sticks to the tongue · Frothy saliva · Absence of salivary pooling in the floor of the mouth · Lobulated/fissured tongue · No (no., %) |
14/30 (46.67%) 4/14 (28.57%) 0/14 (0%) 12/14 (85.71%) 1/14 (7.14%) 0/14 (0%) 16/30 (53.33%) |
9/30 (30%) 2/9 (22.22%) 1/9 (11.11%) 7/9 (77.78%) 0/9 (0%) 1/9 (11.11%) 21/30 (70%) |
0.184 |
3.3. The Correlations among Oral dryness, the Salivary-flow Rate, and the OLP-severity Score in the OLP Group
There was no correlation between the salivary-flow rates (UWS and SWS) and the subjective patients’-reported oral-dryness scores (XI and BI) among the OLP patients. The MST at three minutes, which was found to have high sensitivity and high positive predictive value (17), also showed no association between the XI and BI scores. There was no correlation between the OLP severity score, subjective oral-dryness symptoms, and salivary-flow rates (Table 4). Interestingly, the XI and BI scores were significantly correlated with each other (rs = 0.687, p < 0.001). The association between the UWS and SWS also showed a high positive correlation coefficient (rs = 0.610, p < 0.001). Additionally, MST was associated with UWS (rs = 0.647, p < 0.001) and SWS (rs = 0.655, p < 0.001), respectively (Table 4).
4. DISCUSSION
OLP is a common chronic T-cell-mediated autoimmune disease. Previous studies have reported that OLP patients complain of dry mouth [3, 4]. However, the association between subjective oral dryness and a decreased salivary-flow rate in these patients is still unclear. Thus, we investigated the oral-dryness conditions and salivary-flow rates in the OLP patients by using various measurements. We found that OLP patients had significantly higher XI and BI scores than the controls. In agreement with our findings, Agha-Hosseini et al. showed that OLP patients suffered more dry mouth than their control group [6, 7]. Using a modified XI and Beck’s inventory scale for xerostomia evaluation, similar results have been reported [5, 11]. These data indicate that OLP patients experience oral-dryness symptoms more than non-OLP people do.
| BI Score | MST at 3 minutes | UWS | SWS | Thongprasom Score | |
|---|---|---|---|---|---|
| XI score | rs = 0.687 p < 0.001* |
rs = -0.274 p = 0.142 |
rs = -0.185 p = 0.329 |
rs = -0.077 p = 0.686 |
rs = -0.126 p = 0.507 |
| BI score | - | rs = -0.318 p = 0.087 |
rs = -0.195 p = 0.301 |
rs = -0.095 p = 0.619 |
rs = -0.174 p = 0.357 |
| MST at 3 minutes | - | - | rs = 0.647 p < 0.001* |
rs = 0.655 p < 0.001* |
rs = -0.065 p = 0.731 |
| UWS | - | - | - | rs = 0.610 p < 0.001* |
rs = -0.048 p = 0.801 |
| SWS | - | - | - | - | rs = 0.030 p = 0.877 |
A previous study reported that OLP patients had normal UWS and SWS [11]. Another study showed that the salivary-flow rate was not statistically significantly different among OLP, non-OLP, and the controls [10]. We also found no statistically significant differences in the UWS, SWS, and MST between the OLP and control groups. In our study, CODS in the OLP group indicated that these patients had none to mild xerostomia. The CODS results were also in accord with the results of the salivary-flow rate, which revealed no hyposalivation among the OLP, suggesting that CODS is another useful tool for xerostomia evaluation.
By contrast, previous studies have shown that OLP patients had statistically significantly lower UWS and SWS than controls [6, 7]. However, in these studies, the researchers did not give information about the patients’ mean age and the differences in mean age between the OLP and the control group. It is known that age is one factor that can affect the salivary-flow rate [8]. Therefore, the differences involving people’s ages in the study population may affect the salivary-flow rate results. Lundstrom et al. found that 87% of 39 OLP patients had low or very low UWS [9]. Nevertheless, most of the OLP patients in their study had rheumatoid arthritis and Sjogren’s syndrome, which could have been the reason for their salivary gland hypofunction [8].
MST has been shown to reveal an excellent correlation with the volumetric method for measuring xerostomia [17]. This method is easy to perform, well tolerated, and inexpensive [17, 18]. We found that measuring the salivary-flow rate using the MST gave a high correlation to UWS and SWS in the OLP group. These findings indicate that MST can be routinely used as a chair-side screening tool to determine hyposalivation for OLP in dental clinics.
It has been suggested that oral mucosal alteration can change people’s oral perceptions [21]. Kaplan et al. reported that patients with oral mucosal alteration had statistically significantly higher dry-mouth perception than those with normal mucosa [22]. We found that OLP patients had higher self-reported oral-dryness symptoms than the controls. One possible explanation is that the inflammatory change from OLP lesions can alter patients’ oral mucosa, which leads to the feeling that they have dry mouth. Another study showed that 79% of OLP patients reported a significant dry mouth reduction after topical corticosteroid treatment [23]. This data also supports the conclusion that oral-lesions improvement can ameliorate the symptoms of xerostomia in OLP individuals.
An earlier study showed that Mucin5B, Mucin7, and Proline-rich proteins in saliva protein profiles of OLP patients were significantly lower than among the controls [24]. Another study showed that the level of Mucin5B in the UWS of OLP patients was significantly lower than in the control group [6]. As salivary mucin plays a role in the protective coating, lubricating, and wetting of the oral mucosa [25], a decrease in these proteins may affect the perception of oral dryness among OLP patients. Thus, these findings may further explain the reason for oral dryness among such patients without hyposalivation in this study.
Ramon et al. investigated how different clinical presentations of OLP and the extent of oral mucosal involvement affect salivary-flow rates. These researchers found that the salivary-flow rate was not statistically significantly different between OLP patients with atrophic/erosive lesions and white lesions. The size of the lesions was also not associated with the salivary-flow rate [26]. In accordance with their study, we found no correlation between OLP severity with oral dryness and a patient’s salivary-flow rate. These results were not surprising because OLP is not a disease that first affects the salivary gland [27].
Nevertheless, the sample size in this study is limited, which may lead to insufficient statistical power to detect a difference between the groups. Moreover, the limitation of sample size may be the cause of the negative findings observed in this study. Therefore, a future study with a larger sample size is required for more accurate results and interpretations.
CONCLUSION
Our findings indicate that oral-dryness symptoms were higher among OLP patients than among the controls. However, there was no difference in the salivary-flow rates between the two groups. The severity of OLP lesions was not related to the oral-dryness symptoms or salivary-flow rates. Thus, the reasons for subjective oral-dryness symptoms among OLP patients require further study. Also, dry-mouth symptoms should be considered during the management of OLP.
AUTHORS' CONTRIBUTIONS
VA: study design, data acquisition, analysis and interpretation of data, writing publication; ST: conception and design; PJ: conception and design; PT: conception and design, analysis and interpretation of data, writing publication, critical revision of publication, supervision. All authors have read and approved the final manuscript.
LIST OF ABBREVIATIONS
| BI | = Bother Index |
| CODS | = Clinical Oral Dryness Score |
| MST | = Modified Schirmer Test |
| OLP | = Oral Lichen Planus |
| SWS | = Stimulated Whole Saliva |
| UWS | = Unstimulated Whole Saliva |
| XI | = Xerostomia Inventory |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Srinakharinwirot University Ethics Committee (no. SWUEC/E-464/2563).
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All the humans were used in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013 (http://ethics.iit.edu/ecodes/node/3931).
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
All data supporting the results of this study are available from the authors [V.A and P.T] upon request.
FUNDING
This work was supported by a grant from the Faculty of Dentistry, Srinakharinwirot University [grant number 292/2564].
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


