All published articles of this journal are available on ScienceDirect.
Combined Effect of Fluoride Mouthwash and Sub-ablative Er:YAG Laser for Prevention of White Spot Lesions around Orthodontic Brackets
Abstract
Background:
Development of white spot lesions (WSLs) around orthodontic brackets compromises esthetics and necessitates additional dental treatments.
Objectives:
This study aimed to assess the efficacy of fluoride mouthwash combined with Er:YAG laser irradiation for the prevention of WSLs around orthodontic brackets.
Methods:
Orthodontic brackets were bonded to 50 bovine incisors. The entire tooth surface was coated with acid-resistant varnish except for a margin around the brackets. The microhardness of the teeth was measured at the respective area using the Vickers hardness test. The teeth were then randomly divided into five groups (n=10) of control (Gc), Orthokin fluoride mouthwash (Gf), 100 mJ/cm2 Er:YAG laser (Gl), laser + mouthwash (Glf), and mouthwash + laser (Gfl). Then, the teeth underwent pH cycling according to the standard protocol for demineralization. The microhardness of the teeth was measured again, and the percentage of change in microhardness was calculated. The amount of calcium released during pH cycling was quantified using atomic absorption spectroscopy. Data were analyzed using one-way ANOVA and Tukey’s test.
Results:
Calcium release (indicative of demineralization) in the Gf, Gfl, and Glf groups was significantly lower than that in the Gc and Gl groups (P<0.05). The reduction in surface microhardness was also the same in the five groups with no significant difference (P>0.05).
Conclusion:
Fluoride mouthwash combined with Er:YAG laser or Er:YAG laser alone cannot decrease the incidence of WSLs around orthodontic brackets compared to fluoride mouthwash alone.
1. INTRODUCTION
Improvement of dental and facial esthetics is an important goal in orthodontic treatment. However, the development of white spot lesions (WSLs) is a clinical complication of bracket bonding and orthodontic treatment that can comprise the ultimate esthetic goal of orthodontic treatment, and necessitates additional dental treatments [1]. WSLs occur in about 50% of orthodontic patients [2].
Applying orthophosphoric acid for enamel etching prior to orthodontic bracket bonding and increased Streptococcus mutans colony count in the oral cavity after orthodontic treatment raise the risk of enamel demineralization and dental caries [3, 4]. Furthermore, the development of WSLs is closely correlated with oral hygiene status, such that in patients with poor oral hygiene and absence of adequate plaque control, WSLs can develop around fixed orthodontic appliances in less than 4 weeks following their placement [5].
The optimal efficacy of fluoride in the prevention of caries, its prominent role in the enhancement of remineralization and prevention of demineralization, and its optimal efficacy for impairing the metabolism of cariogenic bacteria and their acid production have been well documented [6]. Topical application of fluoride products in the form of gel, foam, varnish, and solution results in deposition of superficial calcium fluoride crystals on the enamel surface, which would serve as a reservoir for fluoride release during the process of demineralization. Small amounts of fluoride are available in the enamel in the form of fluorapatite, which has less solubility than the formed calcium fluoride and higher resistance against caries. Thus, the application of topical fluoride in various forms is imperative to achieve maximum cariostatic activity [7]. Moreover, the application of fluoride along with a modality to maximize its uptake can guarantee caries prevention [6].
Several laser types have been studied for dental applications since the 1960s to modify the tooth surface and increase its resistance to acid dissolution [8]. The ruby laser was first used in 1966 to enhance enamel resistance to acid attacks. Later in 1966, Nd:YAG laser was first used on enamel samples to confer resistance to the enamel against acid demineralization [9]. At present, laser irradiation is suggested for monotherapy or as an adjunct to prevent enamel caries and inhibit the progression of incipient carious lesions [6, 7, 10]. It has been confirmed that a combination of different laser types with topical fluoridation of enamel is more effective than traditional fluoride therapy. It enhances the enamel resistance to caries and decreases its acid solubility. An important issue is that laser irradiation results in the participation of fluoride in the enamel structure in the form of calcium fluoride and within its crystalline structure in the form of fluorapatite [11]. Thus, laser irradiation and fluoride therapy can have synergistic effects.
Er:YAG laser belongs to the erbium family of lasers and is absorbed by water, hydroxyapatite, and collagen [12]. Er:YAG laser should be used with sub-ablative energy for caries prevention to cause chemical changes without morphological damage to the enamel surface [7]. A previous study showed that the application of a low-energy laser decreased enamel demineralization by 90% [13, 14]. Evidence shows that Er:YAG laser irradiation without coolant is more effective than laser irradiation with coolant for caries prevention. Under suitable conditions, enamel cracks, carbonization, or melting would not occur even in the absence of coolant [7]. Liu et al. [14] reported that Er:YAG laser with sub-ablative energy following fluoride therapy induced immediate conversion of enamel hydroxyapatite to fluorapatite, and subsequently decreased enamel solubility and its demineralization. Some other studies [15, 16] have reported increased enamel resistance to demineralization following the application of Er:YAG laser combined with fluoride, compared to the use of fluoride or laser alone.
Considering the reportedly optimal efficacy of sub-ablative Er:YAG laser irradiation combined with topical fluoride therapy for caries prevention, the availability of fluoride mouthwash, and the gap of information regarding the efficacy of this laser combined with the use of fluoride mouthwash, this study aimed to assess the efficacy of combined use of fluoride mouthwash and sub-ablative Er:YAG laser for prevention of WSLs around orthodontic brackets.
2. MATERIALS AND METHODS
This in vitro experimental study evaluated 50 bovine mandibular incisors. Immediately after collection, the teeth were immersed in 0.09% saline. The attached tissues were removed, and the teeth were rinsed under running water and cleaned using a sickle scaler. They were then immersed in 0.05% chloramine T solution at 4°C for a maximum of 7 days. Next, the teeth were decoronated at 5 mm below their cementoenamel junction by a diamond disc (Degussa Dental, Hanau, Germany) and a high-speed handpiece under water coolant. The buccal surface of the teeth was then cleaned with a prophy brush without prophy paste by using a low-speed handpiece under water irrigation for 30 seconds, and was then polished with a rubber cup for 15 seconds.
The buccal surface of all teeth was then inspected under a stereomicroscope to ensure soundness and the absence of caries and cracks. Teeth with WSLs, demineralized areas, structural defects, or visible wear were excluded.
Prior to bracket bonding, the entire tooth surface was covered with adhesive tape, except for a square-shaped window corresponding to the bracket size, to prevent uncontrolled demineralization of other areas during acid etching. The respective site was then etched with 35% phosphoric acid (Total Etch, Morvabon, Tehran, Iran) for 30 seconds and rinsed for 30 seconds. It was then completely dried with air spray. Orthodontic metal brackets (Ultra-trim Edgewise Brackets; Dentaurum, Ispringen, Germany) were bonded to the tooth surface using Transbond XT composite resin (3M Unitek, Monrovia, CA, USA) according to the manufacturer’s instructions. Excess resin around the brackets was removed by a sickle scaler prior to curing. Next, the adhesive tape was removed from the tooth surface, and the excess adhesive was cleaned with ethanol (Pars Alcohol, Tehran, Iran). Teeth with brackets were then mounted in acrylic resin such that their buccal surface remained exposed. Next, a box with a length equal to the bracket length and 4 mm width was drawn around the bracket with a graphite pencil, and the entire tooth surface, except for the 4 mm margin around the bracket, was coated with acid-resistant varnish in two coats. The respective area was then polished with 1200-grit abrasive paper to obtain a suitable surface for the measurement of primary surface microhardness. The microhardness of the teeth was measured using a Vickers hardness tester (Bareiss, Germany) by applying a 300 g load for 10 seconds. The test was repeated in triplicate for each specimen, and the mean of the three values was recorded as the microhardness of the sample. During this process, the teeth were kept in screw-top containers containing a moist cotton pellet to provide > 95% humidity.
The samples were then randomly divided into five groups (n=10) of control (Gc), Orthokin fluoride mouthwash (Gf), 100 mJ/cm2 Er:YAG laser (Gl), laser + mouthwash (Glf), and mouthwash + laser (Gfl).
No intervention was performed in the Gc group. Samples in the Gf group were placed in a mesh in Falcon tubes containing 0.05% Orthokin mouthwash (Orthokin, McCabes Pharmacy, Spain) and incubated at 37°C for 12 hours; this period corresponded to twice daily use of mouthwash for 12 months [17]. The solution was agitated every 3 hours to ensure homogeneity. In the Gl group, Er:YAG laser (Fidelis plus III, Photona, Slovenia) was irradiated with 5 Hz repetition rate, 1 mm spot size, 0.5 W power, 100 µs pulse duration, 100 mJ/cm2 energy density, and 10 seconds time at 5 mm distance. The square-shaped area was subjected to laser irradiation with the above-mentioned settings.
In the Gfl group, the samples were exposed to fluoride mouthwash and then subjected to laser irradiation, as explained above. In the Glf group, surface treatment was performed first with laser and then with mouthwash. After the intervention, the samples underwent pH cycling for induction of artificial caries according to the following protocol:
All 10 teeth in each group were immersed in 40 mL of a demineralizing solution containing 0.075 M acetic acid (SIGMA, CAS: 64-19-7) and 2 mmol calcium hydrogen phosphate (SIGMA CAS: 7757-93-9) at 37°C and a pH of 4.3 for 6 hours. Next, the teeth were completely rinsed with distilled water for 10 seconds and dried with absorbent paper. The teeth were then immersed in 40 mL of a remineralizing agent comprising 20 mmol/L sodium cacodylate (SIGMA, CAS: 6131-99) as a buffering agent, 150 mmol/L potassium chloride (MERCK CAS: 7447-40-7), 1.5 mmol/L calcium nitrate (Panreac CAS: 13477-34-4), and 0.9 mmol/L potassium phosphate (SIGMA CAS:7778-77- 0) at a pH of 7 at 37°C for 18 hours. The demineralization and remineralization cycles were repeated every 24 hours for 9 days. Next, the teeth were placed in the remineralizing solution for 24 hours.
The teeth were thoroughly rinsed with distilled water, and their structural changes were evaluated by atomic absorption spectroscopy and the Vickers hardness test.
To assess the changes in the structure of the teeth, the amount of calcium released from the tooth structure into the demineralizing solutions was quantified at the time of exchange of solutions using atomic absorption spectroscopy (SpectrAA 220, Varian, Australia). The microhardness test was performed again after pH cycling according to the standard protocol mentioned earlier. The percentage of change in microhardness was computed by the formula below:
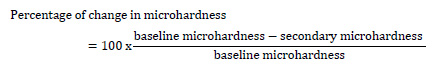 |
The data were analyzed using Statistical Package for the Social Sciences software (PASW Statistics 18; SPSS Inc., Chicago, IL, USA) by one-way ANOVA and Tukey’s test. The level of significance was set at 0.05.
3. RESULTS
Table 1 shows the mean concentration of calcium released in the study groups. The difference in the amount of calcium released into the demineralizing solution was significant among the groups (P<0.05). The groups subjected to fluoride mouthwash (Gf, Gfl, and Glf) showed minimum release of calcium ions, and significantly lower calcium release compared to the control group (P<0.05). However, the difference in calcium release was not significant among the three groups of Gf, Gfl, and Glf (P>0.05). The calcium release in the laser group was not significantly different from that in the control group (P>0.05). However, the laser group showed significantly higher calcium release than other groups (P<0.05). Table 2 presents pairwise comparisons of the groups regarding calcium release.
Table 1 also shows the percentage of reduction in microhardness of specimens. Reduction in microhardness occurred in all groups after pH cycling compared to baseline, with no significant difference between them (P>0.05).
| Group | Gc | Gl | Gf | Glf | Gfl |
|---|---|---|---|---|---|
| Calcium release (µg/mL) ± std. deviation | 99.20±8.32 | 103.40±9.39 | 89.10±6.99 | 88.80±7.22 | 85.50±5.12 |
| Mean percentage of change in microhardness ± std. deviation | 40±67.40 | 56.74±19.12 | 53.77±43.84 | 61.21±18.22 | 63.65±23.51 |
| Group (I) Group (J) | P value | |
| Laser | Fluoride mouthwash | 001.0 |
| Laser + fluoride mouthwash | 001.0 | |
| Fluoride mouthwash + laser | 000.0 | |
| Control | 726.0 | |
| Fluoride mouthwash | Laser + fluoride mouthwash | 000.1 |
4. DISCUSSION
This study assessed the efficacy of the combined use of fluoride mouthwash and sub-ablative Er:YAG laser for the prevention of WSLs around orthodontic brackets. Several methods have been used to assess the efficacy of interventions on the tooth structure to confer resistance to demineralization, including measurement of microhardness [13, 18], electron microscopic assessments [6, 13], quantification of calcium and phosphorous ions released into the demineralizing solution by atomic absorption spectroscopy [19], and measuring the depth of lesions under a polarized electron microscope [20, 21]. In the present study, the microhardness was measured, and the calcium ions released into the demineralizing solution were quantified.
Our null hypothesis was partially rejected since calcium release into the demineralizing solution in the Gf, Glf, and Gfl groups, was significantly lower than that in the Gc and Gl groups. However, all groups showed a significant reduction in microhardness after pH cycling compared to baseline (P<0.05).
In this study, Er:YAG laser was used without water irrigation similar to the study by Nair et al. [22]. Water irrigation was not performed because it has been demonstrated that laser irradiation without water coolant confers higher caries resistance to enamel [19]. The results of the present study showed that calcium release in the laser-irradiated group was the same as that in the control group; this result was in accordance with that of other studies [22-24]. Several theories have been proposed to explain the cariostatic effects of Er:YAG laser. The first theory explains that laser irradiation decreases the permeability of the enamel surface due to the loss of carbonate structure and the formation of pyrophosphate, which is more stable and has less solubility [18, 19]. The second theory is the original matrix blocking theory, which explains that changes in the organic matrix of the tooth structure by laser irradiation obstruct the microscale routes of infiltration in the enamel structure [12]. The laser energy absorbed by the surface is converted to thermal or thermomechanical energy, which alters the surface [25]. It appears that laser irradiation without water irrigation might have resulted in the accumulation of debris caused by laser pulses, affecting the change in photo-crystals of the tooth structure and resulting in the inefficacy of laser. Kuscer and Diaci [26] demonstrated that in the absence of water irrigation, using a brush can enhance the ablative efficacy of laser, and stated that the residual products on the surface would prevent the penetration of subsequent laser pulses and their optimal efficacy. Also, an additional explanation was that the peak rise of temperature in their study was not enough to create crystallographic changes in the enamel, and the changes were limited to water evaporation and carbonate loss [22]. However, some other studies showed increased resistance of enamel to acid demineralization following sub-ablative laser irradiation [27, 28]. This difference in the results may be attributed to the variations in laser parameters, such as repetition rate and power, use of water irrigation, type of laser handpiece (contact or non-contact mode), type of tooth (human versus bovine enamel), type of fluoride product (acidulated phosphate fluoride gel in their study versus fluoride mouthwash in our study), and the pH cycling protocol. Additionally, this type of demineralizing agent is essential when assessing the calcium release pattern of the demineralizing agent.
Another finding of the present study was that calcium release was the lowest in the Gfl group, followed by the Glf and Gf groups; although the difference in this respect was not significant among the three groups, and they all showed similar changes in their surface microhardness.
The results of calcium release in the Glf and Gf groups were the same as those reported by Alten et al. [19], while the results of calcium release in these groups were in contrast to other studies [24, 29]. Regarding the mechanism of laser irradiation prior to topical fluoride application, it should be noted that laser must create crystallographic changes to enhance fluoride uptake [19] and provide a strong bond between the fluoride and tooth structure [18].
In contrast to our study, Altan et al. [19] reported that laser irradiation after topical application of fluoride significantly decreased its efficacy. They explained that the use of water spray during laser irradiation might have resulted in the removal of fluoride from the surface. On the other hand, laser irradiation may cause the breakdown of the newly formed fluorapatite crystals [19].
An interesting finding in our study was that the results of calcium release were different from the microhardness test results. The Gl group showed minimal change in microhardness after pH cycling, followed by the Gl, Glf, Gfl, and Gf groups; however, the difference was not significant. Behroozibakhsh et al. [29] showed that the microhardness significantly decreased in the laser-irradiated group. They concluded that laser creates microcracks and fissures, and increases the enamel surface roughness, enhancing demineralization. However, the microhardness increased in the Glf and Gfl groups in their study; this increase in microhardness may be related to the use of acidulated phosphate fluoride in their study in comparison to the mouthwash used in our study [29]. A search of the literature by the authors yielded no study assessing both calcium release and microhardness of enamel to compare our results with.
As mentioned earlier, the type of remineralizing agent and the pH cycling protocol can affect the results. Dihydrogen phosphate potassium is commonly used in pH cycling [30]. However, we used dihydrogen calcium phosphate, which might have affected the calcium release pattern, and may be responsible for the discrepancy in the results of calcium release and microhardness test. Moreover, 300 g load was applied for 10 seconds at a minimum distance of 5 µm in the microhardness test; however, the range of load varies in the literature [31].
Most studies on the combined use of fluoride and laser therapy have used fluoride varnish and fluoride gel, which provide a higher percentage of fluoride ions compared to the mouthwash used in our study. Clinical studies have not shown no significant difference between different forms of topical fluoride, such as varnish, gel, or solutions in terms of caries prevention [32]. Thus, the selection of the form of fluoride product depends on the cost, availability, patient’s preferences, and safety. Since fluoride mouthwashes are available over-the-counter and are of low cost, they are often preferred by patients. Moreover, orthodontists routinely prescribe fluoride mouthwash for their patients. Orthokin mouthwash has shown superior results with respect to the reduction of Streptococcus mutans count and plaque index, compared to Listerine and Oral-B mouthwashes [33]. Thus, Orthokin was used in our study, which contains 226 ppm fluoride (0.22%), zinc acetate (0.24%), and chlorhexidine (0.06%), and is alcohol-free [33]. The authors believe that the low concentration of fluoride in this mouthwash may be responsible for the inefficacy of fluoride in the Glf and Gfl groups to enhance the microhardness and decrease calcium release in comparison to the Gf group.
This study has some limitations. The technique of application of mouthwash was different from the clinical setting. Moreover, the laser was irradiated without water coolant, which is not performed in the clinical setting due to the risk of thermal damage to the pulp. Kuscer and Diaci [26] did not use water irrigation during laser irradiation; instead, they used water spray between the pulses. This was done to minimize the effect of excess water on ablative laser energy and, at the same time, eliminate the concerns related to thermal damage. This strategy should be evaluated in future studies. However, the concerns related to the removal of fluoride from the tooth surface by water irrigation still exist in this technique. Future studies are required to assess the surface topography of the samples using scanning electron microscopy. Moreover, the clinical setting should be better simulated in future studies.
CONCLUSION
Within the limitations of this in vitro study, the results showed no significant difference in the microhardness of the groups. However, fluoride mouthwash + laser, laser + fluoride mouthwash, and fluoride mouthwash alone showed significantly superior results in the prevention of demineralization.
LIST OF ABBREVIATIONS
| WSLs | = White spot lesions |
| Nd-YAG | = Neodymium-doped yttrium aluminum garnet |
| Er:YAG | = Erbium-doped yttrium aluminum garnet laser |
| Gc | = Control group |
| Gf | = Orthokin fluoride mouthwash group |
| Gl | = Er:YAG laser group |
| Glf | = Laser + mouthwash group |
| Gfl | = Mouthwash + laser group |
ETHICAL STATEMENT
This in vitro experimental study was approved by the ethics committee of the Tehran University of Medical Sciences (ethical approval code: IR.TUMS.VCR.REC1397.595).
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author [M.S.A.A] upon reasonable request.
FUNDING
This study was supported by a grant from the Dental Research Center Dentistry Research Institute, Tehran University of Medical Sciences, Tehran, Iran (grant no 97037040139).
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest related to the publication of this article.
ACKNOWLEDGEMENTS
Declared none.


