Oral Hygiene Instruction – How it Affects the Caries Experience, Oral Hygiene Status, and sCD14 Levels?
Abstract
Background:
Caries experience, oral hygiene status, and salivary sCD14 level are three essential factors to analyse individual dental caries development risk. Therefore, regular and effective oral hygiene instruction (OHI) is essential for dental caries prevention.
Objective:
This study aims to analyse the differences in caries experience, oral hygiene status, and sCD14 levels before and after OHI.
Methods:
An observational study with intervention before and after oral hygiene instruction was conducted on 40 samples of each group taken with an accidental sampling method. The sample was calculated using the sample size formula to determine the difference between two paired means; confidence level 95%; power test 90%. The OHI materials include microbial aspects, plaque control methods and instruments, and directives for visiting the dentist. Caries' experience was obtained using DMF-T index; oral hygiene status using simplified oral hygiene instruction (OHI-S); sCD14 levels obtained from unstimulated saliva using an ELISA kit. Data analysis used the Kolmogorov-Smirnov normality test, paired t-test, and Wilcoxon signed-rank test.
Results:
Kolmogorov normality test showed that the caries experience data were normally distributed, while oral hygiene status and sCD14 were not. The paired-t difference test result for caries experience cannot be determined because the data showed a similar value. The Wilcoxon signed-rank test result for oral hygiene status showed no significant difference, while the sCD14 showed a significant difference.
Conclusion:
Oral hygiene instruction showed a similar value of caries experience before and after oral hygiene, and also no difference was found in oral hygiene status; however, the sCD14 levels showed a difference after oral hygiene instruction.
1. INTRODUCTION
The distribution and incidence of caries in society have shifted to a much higher than the recommended average value. However, there is still a sizable minority population with a significant caries burden which raises significant challenges at both clinical and public health levels in maintaining health and managing individuals with a significant burden of caries disease, most of which is preventable [1].
The prevalence and experience of dental caries, consisting of decayed, missing, and filled teeth, also well-known as DMFT, has decreased in many high-income countries for decades. However, increasing prevalence and experience of caries are noted at the global level, with an increasing plurality level, which indicates the unequal distribution of the prevalence and experience of dental caries experience [2]. Untreated carious lesions in the permanent teeth remain the most common condition, affecting 2.4 billion people worldwide in 2016 [2].
Health is one of the most valuable assets of an individual. Oral health is now recognised as equally important as general health. Oral health can be defined as the standard of dental, oral, and supporting tissue that enables a person to eat, talk, and socialise without feeling any pain, discomfort, or embarrassment, contributing to an individual's well-being [3, 4]. Oral health can improve the quality of life, enabling someone to be engaged in all activities, increasing productivity, and increasing learning capacity [5].
Poor oral hygiene can lead to severe illnesses, such as periodontitis, dental caries, pain and discomfort in the teeth or gums, infection, and tooth loss [6]. However, treatment for oral health conditions is expensive and usually not included in the universal health coverage (UHC). In most high-income countries, dental care accounts for 5% of total health spending and 20% of personal health spending. However, most low- and middle-income countries cannot provide services to prevent and treat oral health conditions [4]. Thus, low-cost care programs are a necessity.
Oral hygiene is performed by brushing and flossing. It is also supported through diet or nutrition, education regarding a healthy diet for oral and systemic health, including knowledge about foods and beverages that contribute to caries [7]. Poor oral hygiene will trigger gingivitis and decay of the tooth structure, resulting in caries.
Oral health professionals and the American Dental Association (ADA) argued the importance of educating patients to practice proper oral hygiene [8]. In dentistry, a paradigm shift has occurred where the emphasis has shifted from curative services to preventive healthcare services that serve preventive effort before any decay occurs. Therefore, oral health promotion has been considered very important for the services provided by dentists to their patients [7, 9].
Implementing oral health promotion benefits both service providers and patients as individuals to effectively implement proper daily oral health practices. However, dental service providers need to be careful in presenting information focusing on implementation time and educational materials [7]. Oral hygiene instruction is one of the most effective methods for preventing plaque formation and improving individual toothbrushing skills [10, 11]. In addition, providing education, hands-on instruction, practice and peer-to-peer problem-solving lead to increased knowledge about oral health issues [11].
One of the proteins that play an essential role in the early detection of caries is sCD14 [12-14]. In addition, salivary sCD14 plays an essential role in protecting the oral cavity's soft and hard tissues from pathogenic bacteria infection [12]. sCD14 is a coreceptor involved in recognizing Gram-negative and positive bacteria. Infection is known to affect serum [15]. Caries state and oral hygiene status are closely related to sCD14 because oral health is correlated with general health [16]. All of the previously described backgrounds, which were fundamentals of the hypothesis, are differences in caries experience, oral hygiene and sCD14 levels before and after oral hygiene instruction (OHI). Aim of this research are to analyze the differences in caries experience, oral hygiene status, and sCD14 levels before and after oral hygiene instruction (OHI).
2. MATERIALS AND METHODS
The research method used an observational study with intervention before and after oral hygiene instruction. The population is adults from the Sekeloa region that met the inclusion and exclusion criteria. Inclusion criteria are adult, no missing teeth, able to read and write. Exclusion criteria were the subject of research which was not willing to participate in all research phases.
Research participants were obtained through the accidental sampling technique. The sample was calculated using the sample size formula to test the difference between two paired means. The confidence level was chosen at 95% (Z1-α = 1.95); power test at 90% (Z1-β = 1.28). The magnitude of Sd and μd was obtained from the preliminary research on oral hygiene status conducted by Adilah et al. [17]; Sd = 0.67662 and the mean difference (μd) = 1.366 – 0.9712 = 0.3838. Thus, from the sample size formula mentioned priorly obtained that n = 35, by increasing the drop out by 10%, therefore, it was necessary to determine the minimum number of subjects n = 1 / (1-0.1) x 35 = 39 (rounded up to 40). Based on the calculation, the research sample for each group of pretest and post-test was 40 samples.
The research setting was the oral hygiene instruction material that included microbial aspects, plaque control methods, plaque control instruments, and directions for visits to the dentist, the content of which has been validated by three experts in dental cariology and dental public health. Oral hygiene instruction was given face-to-face every three days for two weeks—the research location was in the Sekeloa region, Bandung, Indonesia. Periods of recruitment were from January until March 1, 2019, before Covid-19 was spread in Indonesia.
The exposure effect of oral hygiene instruction was assessed by a pretest examination of caries experience, obtained using the DMF-T index. Oral hygiene status was obtained with Oral Hygiene Index – Simplified (OHI-S), which has two components, the Debris Index-Simplified (DI-S) and the Calculus Index-Simplified (CI-S), and the other value measured was sCD14 level. Follow-up, post-test examination of caries experience, oral hygiene status, and sCD14 level were assessed after two weeks of pretest examination.
Data collection of caries experience was obtained using DMF-T index; oral hygiene status using Oral Hygiene Index – Simplified (OHI-S) with two components, the Debris Index-Simplified (DI-S) and the Calculus Index-Simplified (CI-S), then calculated separately and summed up to determine the OHI-S value. The examination was performed using a mouth mirror and a CPITN probe. The index was interpreted as follows: good (0-1.2), adequate (1.3-3.0), and poor (3.1-6.0) [18].
Data collection of the salivary sCD14 levels were measured on thawed samples using the ELISA method with Human CD14 Quantikine ELISA Kit (Catalog DC140, R&D Systems, Minneapolis, MN, USA/item code of ELISA kit in catalogue), and the data was recorded. All the reagents, working standards and samples were made according to the manufacturer's instructions. All the samples were analysed with the same kit in the same laboratory. The sample was aliquoted into two microtubes with a volume of about 1ml each. The sample tested was only 100µl according to the manual book kit procedure of assay in preparing all reagents.
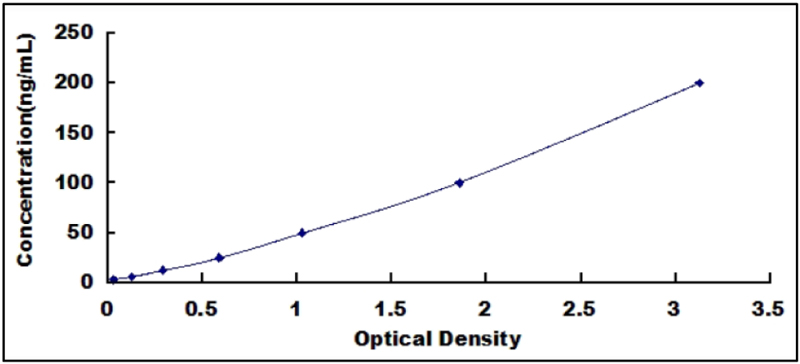
Data collection of the salivary sCD14 samples was quantified utilising a custom human protein array (Quantibody Custom Array; RayBiotech, Inc., Norcross, GA, USA). The resultant sample signals were compared against the standard curve to determine the sCD14 concentration (Fig. 1) [19, 20]. Data were extracted and analysed using the microarray analysis software (RayBio Q Analyzer software; RayBiotech, Inc., Norcross, GA, USA). The test principle, sCD14 calculation method, typical standard data curve, detection range, sensitivity, and specificity were performed according to the manufacturer's instructions (Cloud-Clone Corp., Katy, Texas, USA) [19]. The result of the measurement of sCD14 level was then categorised as follow: 0 = not normal sCD14 level (> 2-4 μg mL-1); 1 = normal sCD14 level (< 2-4 μg mL-1) [14, 21, 22].
As much as 100μL of standard or sample was added to each well, then incubated for 1 hour at 37°C. The sample was then aspirated and washed three times. Next, another 100μL of standard or sample was added to each well to prepare detection reagent B, then incubated for 1 hour at 37°C. The sample was then aspirated and washed five times, and 90μL of substrate solution was added afterwards. The next stage was incubation, performed for 10-20 minutes at 37°C, then added 50μL of stop solution. The result was read at 450nm immediately [19]. The processing time was approximately 5 hours from the start of preparation to completing the reading.
Prior to this study, ethical clearance was provided by the Universitas Padjadjaran Health Research Ethics Committee. Every procedure and ethical aspect of the current research conducted was entirely under the World Medical Association Declaration of Helsinki. All participants gave written consent to participate in the current study [23]. As required of this research, the study was conducted concerning the ethical guidelines for research and health development, and all respondents have received, filled out, and returned the informed consent to the research team.
2.1. Statistical Analysis
All the data were analysed into the SPSS version 22.0 software package. A p-value of <0.05 was considered statistically significant. Data analysis was carried out with the Kolmogorov-Smirnov normality test, while the different tests were conducted with the Wilcoxon signed-rank test for not normally distributed data and paired t-test for normally distributed data. The potential of bias was carried out by calibrating measurements for all item variables with a Kappa index of 0.7, then recorded by the recorder team while considering the inclusion and exclusion criteria. The missing data was avoided by check recheck; however, the socio-economic aspects can be potential bias in this research because the socio-economic aspect of samples is various.
3. RESULTS
The number of samples in the pretest was 55; however, samples following all phases of research were only 40 samples because 15 samples were unable to follow the complete phase due to their busy work. The characteristics of respondents who followed all of the research phases are presented in Table 1, which shows that most of the current research respondents were female.
| Categories | Before intervention | After intervention | ||
|---|---|---|---|---|
| Index/Frequency | % | Index/Frequency | % | |
| Male | 16 | 40 | 16 | 40 |
| Female | 24 | 60 | 24 | 60 |
| Total | 40 | 100 | 40 | 100 |
Table 2 shows that the caries experience was 6.2 before and after oral hygiene instruction intervention. Prior to the intervention, the highest percentage of oral hygiene status was found in the moderate category, while after, it was in a good category. The sCD14 levels prior to the intervention showed a not normal percentage of 82.5%, and after treatment was 100%.
| Categories | Before Intervention | After Intervention | ||
|---|---|---|---|---|
| Index/Frequency | % | Index/Frequency | % | |
| Caries experience (DMF-T index) | 6.2 | - | 6.2 | - |
| Oral Hygiene Index (OHI-S) | ||||
| Good | 15 | 37.5 | 19 | 47.5 |
| Moderate | 24 | 60 | 17 | 42.5 |
| Poor | 1 | 2.5 | 4 | 10 |
| Total | 40 | 100 | 40 | 100 |
| sCD14 | ||||
| Normal | 7 | 17.5 | 0 | 0 |
| Not normal | 33 | 82.5 | 40 | 100 |
| Total | 40 | 100 | 40 | 100 |
Table 3 shows that the caries experience data before and after the oral hygiene instruction had a normal distribution, while the oral hygiene status (OHI-S) data was not normally distributed. In addition, data on sCD14 levels before and after oral hygiene instruction was also not normally distributed.
| Category | P-value | Notes |
|---|---|---|
| Caries experience (DMF-T index) before | 0.052 | Normally distributed |
| Caries experience (DMF-T index) after | 0.052 | Normally distributed |
| Oral hygiene status (OHI-S) before | 0.000 | Not normally distributed |
| Oral hygiene status (OHI-S) after | 0.000 | Not normally distributed |
| sCD14 before | 0.000 | Not normally distributed |
| sCD14 after | 0.000 | Not normally distributed |
The data presented in Table 4 showed that data before and after oral hygiene instruction have a similar value; thus, the p-value cannot be determined. The difference in oral hygiene status (OHI-S) before and after oral hygiene instruction showed no significant difference; however, the sCD14 levels showed a significant difference.
| Research Variables | Test Results | ||
|---|---|---|---|
| Mean | Standard deviation | P-value | |
| Caries experience (n=40) | |||
| DMFT pre-intervention | 6.2 | 5.21 | Undetermined |
| DMFT post-intervention | 6.2 | 5.21 | |
| Median | Z-value | P-value | |
| Oral hygiene status (OHI-S) (n=40) | |||
| Oral hygiene status (OHI-S) pre-intervention | 16.5 | -1.300b | 0.194 |
| Oral hygiene status (OHI-S) post-intervention | 33 | ||
| Median | Z-value | P-value | |
| sCD14 | |||
| sCD14 levels pre-intervention | 33.29 | -4.987b | 0.000* |
| sCD14 levels post-intervention | 80.45 |
4. DISCUSSION
Caries' experience before and after treatment with oral hygiene instruction was 6.2 (Table 2). This result was almost similar to Drachev et al. [24], which studied caries with an average DMFT index of 7.5818, while different from the study of Susilo et al. [25], which stated that the DMF-T index was 9.13. Based on the WHO category, the value of 6.2 is classified as a low category for 35-44 years [26]. However, even though this result was categorized as low, it was still suggested that each subject had 6-7 decayed teeth, which will lead to dental caries. Thus, preventive efforts must be taken to stop caries development and ensure no additional carious lesions because the more tooth decay found, the higher the negative impact on the quality of life [5].
Caries' experience before and after intervention in oral hygiene instructions showed no difference (Table 2). This result was found to be different from the study of Haque et al. [27], which stated that the prevalence of untreated dental caries in the study population after the OHE program was significantly (p < 0.01) reduced to 42.5%. This difference might occur because many research results stated that oral hygiene interventions could only reduce dental plaque [27].
The above results occurred because the results of the post-test examination showed that oral hygiene instructions to perform a dental visit to perform dental fillings were not followed by all research subjects. These results indicated the need to provide treatment-seeking motivation, as stated by Nagarajan et al. [28], who stated that motivation is the basis in physiological, behavioural, cognitive and social areas and is the basis in encouraging well-being optimisation, minimising physical pain, and maximising happiness. Therefore, motivation also plays an essential role in increasing oral treatment-seeking behaviour. Different theories and models, such as the push-pull model [29] and the self-determination theory [24-33], have attempted to explain the various intrinsic and extrinsic influences that influence individual motivation to undergo or refuse treatment. However, the difference test result of oral hygiene status (OHI-S) before and after oral hygiene instructions showed no significant difference. This result was in line with the studies of Shamani et al. [30] and Chang et al. [31], which stated that the effectiveness of oral hygiene instructions is often poor. The motivational interviewing technique has been practised to change behaviour and is suitable for an individual treatment plan. However, the current study contradicts the study of Soldo et al. [32], which suggested a significant difference in oral hygiene status after oral hygiene instruction, although decreasing six months afterwards. Yandi et al. [33] also noted an improvement in oral hygiene status (OHI-S) after oral hygiene instruction.
The level of oral hygiene might cause explanations for results previously described, and oral health knowledge was low, requiring a communication-behavioural approach to choose a more appropriate method to improve oral hygiene. People have different learning styles or characteristics to process information, so it is necessary to determine effective oral health education programs [32]. A comprehensive and effective oral health education program must be designed to meet the knowledge gap and adapted to target the least recognised topics, such as the aetiology and association of systemic conditions [34].
The sCD14 levels before and after giving oral hygiene instructions showed significant differences. This result, however, cannot be compared with previous studies because there has been no research on a similar topic; also, the oral hygiene instruction package only provides directions for dental visits, not directing how to remove carious lesions. However, the current research was conducted because oral diseases are closely related to oral hygiene, especially regarding dental plaque [35]. Plaque is the leading cause of dental caries, and periodontal disease is the most common oral disease in the community. Therefore, the human oral cavity requires more treatment than the rest of the human body [35].
The subjects in this study had decayed, missing and filling teeth due to caries. However, this value remained during oral hygiene instructions, indicating the possibility of developing caries lesions or additional lesions. This finding was consistent with Pellegrini et al. [20], who stated that several studies suggested a significant increase in the salivary sCD14 of subjects with dental caries. The mean salivary sCD14 concentration was 28.3±10.8μg/ml (range: 10.3–53.1μg/ml) in subjects without dental caries (Healthy-H Group) and 22±9.6μg/ml (range: 3.6–46.6 g/ml) in subjects with dental caries (Decayed-D Group). Supporting finding was also discovered from the research conducted by Aripin et al. [15], which stated that sCD14 was one of the first receptors to recognise caries.
The limitations of the present study were the socio-economic aspect as the potential bias. Therefore, further research must assess this particular aspect because it strongly influences caries experience, oral hygiene status, and sCD14 as an infection marker in oral health. However, this research's limitation does not indicate that the present study result's generalisability (external validity) was not good. Previous research has also suggested that socioeconomics does not influence caries experience, oral hygiene status, and sCD14 as infection markers in oral health.
CONCLUSION
Oral hygiene instruction showed a similar value of caries experience before and after oral hygiene, and also no difference was found in oral hygiene status; however, the sCD14 levels showed a difference after oral hygiene instruction.
LIST OF ABBREVIATIONS
| OHI | = Oral Hygiene Instruction |
| UHC | = Universal Health Coverage |
| ADA | = American Dental Association |
| (DI-S) | = Debris Index-Simplified |
| (CI-S) | = Calculus Index-Simplified |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study has been approved by the Universitas Padjadjaran Health Research Ethics Committee, with an approval number of 302/UN6.KEP/EC/2020.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures were followed by the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
All subjects participated voluntarily and gave their informed consent.
STANDARDS OF REPORTING
STROBE guidelines and methodologies were followed for this study.
AVAILABILITY OF DATA AND MATERIALS
The current study data is available in the Faculty of Dentistry Universitas Padjadjaran, Indonesia, and will be available from the corresponding author, [D.A.] on request.
FUNDING
This research was funded by the Faculty of Dentistry and Directorate for Research and Community Engagement (DRPM) of Universitas Padjadjaran with the grant number 1959/UN6.3.1/PT.00/2021.
CONFLICT OF INTEREST
The authors certify that they have no commercial or associative interest representing a conflict of interest in connection with the manuscript.
ACKNOWLEDGEMENTS
Declared none.


