All published articles of this journal are available on ScienceDirect.
Patient Satisfaction and Oral Health-related Quality of Life (ohrqol) of Edentulous People after Mandibular Denture Relining With a Soft-liner Material: A Pilot Study
Abstract
Background:
Oral health-related quality of life indicators have been effectively used to assess the influence of a range of dental treatments and interventions on patient satisfaction and acceptance.
Objectives:
The purpose of this study was to evaluate the impact of the relining of mandibular dentures with a soft-liner material, using the Oral Health Assessment Index (OHIP-14).
Methods:
Forty-two full denture wearers were selected from patients who attended 9 private prosthetic clinics in New South Wales, Australia. All participants had their lower dentures relined with a soft-liner material, according to the manufacturer’s instructions. Oral health-related quality of life was evaluated before and 1 month after relining using the Oral Health Assessment Index questionnaire. A simple descriptive quantitative analysis of the survey results was undertaken, including a comparison of median scores using the Wilcoxon paired test and binomial probability test.
Results:
In all the outcome variables measured, there was a noticeable positive effect from the denture relining. Specifically, mandibular denture relining with a silicon-based soft-liner material has a positive impact on patient satisfaction and oral health-related quality of life (OHRQoL) of edentulous patients.
Conclusion:
Patient satisfaction and oral health-related quality of life (OHRQoL) of edentulous patients can be significantly improved by the use of soft-liner materials.
1. INTRODUCTION
Improvements in oral healthcare over recent decades have seen a significant decline in the number of edentulous people, however, the anticipated increase in life expectancy may indicate that edentulism will plateau and could increase in the future [1, 2]. Facial appearance and the ability to speak and masticate food without pain or discomfort are important factors, which can significantly affect the quality of life [3]. The loss of all natural teeth has functional and psychosocial consequences that can, in many cases, be remediated with the provision of removable dentures [4]. However, poorly fitting and unstable dentures represent a great challenge to both patients and clinicians, and these challenges are often increased as people age and are less able to adapt to changes due to changes in muscle tone and control. These changes tend to decrease a person’s capabilities of ageing well, and can significantly affect their quality of life [5].
Most clinicians believe that well-fitting dentures help maintain the supporting tissues in good health and improve oral function and self-esteem of the patient [6]. Although several studies have found a weak correlation between patient satisfaction and professionally perceived clinical quality of full dentures, it is evident that reliable data to substantiate this is sparse [7, 8].
Over time full dentures, most notably the mandibular denture, can lose retention, become unstable and painful due to changes in the supporting tissues [8]. One of the approaches to manage this issue i.e., poorly fitting dentures is to reline them, which involves the remodelling of the anatomical surface of the denture.
A number of studies have assessed patient satisfaction with denture relining and their preference between relining with resilient (soft) denture materials and conventional heat-activated acrylic resin, both options opposed by acrylic resin-based maxillary full dentures [9-11]. In general, these studies have reported a significant improvement in patient satisfaction and oral health-related quality of life (OHRQoL) associated with soft relining of dentures. However, these factors have not been investigated in an Australian population. Hence this study aims to assess the effect of soft relined dentures on the OHRQoL in an Australian population.
2. MATERIALS AND METHODS
Ethical approval (H-2-015-0128) for this study was obtained by the Human Research Ethics Committee of the University of Newcastle, Australia. A simple quantitative survey, the Oral Health Assessment Index OHIP14-EDENT questionnaire [12, 13], which addresses four main domains (mastication, psychological, social, and oral pain) was used to evaluate patient satisfaction and oral health-related quality of life, before and after mandibular denture relining with a soft relining material, in edentulous patients [12, 13].
Participants were selected from patients who attended nine private prosthetic clinics in New South Wales, Australia. The participants were completely edentulous patients, wearing full maxillary and mandibular dentures, and all patients were seeking prosthetic treatment to improve the functional ability and comfort of these dentures. The patients were examined by a clinician in each facility and had to meet strict inclusion criteria to be invited to participate in the project.
Patients were eligible for inclusion if they experienced discomfort or inability to use their mandibular dentures due to oral pain, discomfort and/or denture instability and/or retention problems. Their current set of maxillary and mandibular full dentures must have been worn for at least one year, and up to a maximum of five years. Patients aged between 40 and 65 years, with no implants, and who exhibited no major changes in the occlusal vertical dimension and/or centric occlusion were considered for inclusion in this study.
Patients were excluded from the study if they had oral mucosal inflammation or lesions, where the screening clinician prescribed the need for a temporary/interim therapeutic soft denture liner, prior to further treatment. Presence of one or more, mild to severe signs or symptoms of temporomandibular joint disorders, significant restriction in the opening movement of the mandible, or radiographic evidence of infected retained roots, cysts, or bone spicules also excluded patients from participating. Multi-repaired dentures also excluded patients.
Prior to relining the mandibular denture, participants completed the OHIP-14 questionnaire in a paper format. The mandibular dentures were relined with a silicone-based soft liner material, according to the manufacturer’s instructions. The materials used were predominantly Vertex™ Soft (heat curing soft acrylic resin) materials, and Molloplast-B (one component-heat curing). All the participants completed the OHIP-14 questionnaire again, after using their relined dentures for one month.
All statistical analyses were conducted using the Statistical Package for the Social Sciences (SPSS), version 27. All the variables were scored using a five-level Likert scale (0: never; 1: hardly ever; 2: occasionally; 3: often; 4: very often). As the data was presented as ordinal data, a non-parametric test (Wilcoxon test) was performed to analyse all the outcome variables before and one month after denture relining. In addition, binomial probability test was conducted to statistically analyse the noted improvements between the two sets of data. The level of significance (p) was set at 0.05.
3. RESULTS
Forty-two complete denture wearers, 27 female and 15 males were selected based on the inclusion criteria. All patients had their mandibular dentures relined with a soft-liner material (silicon-based material) according to the manufacturer’s recommendations. Across all outcome variables measured there was a noticeable positive effect of denture relining with soft liner materials (p<.001). Table 1 presents the responses before relining of the dentures, and one month after relining.
| - | Outcome Variables | Never | Hardly Ever | Occasionally | Fairly Often | Very Often Before | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Before (%) | After (%) | Before (%) | After (%) | Before (%) | After (%) | Before (%) | After (%) | Before (%) | After (%) | ||
| 1 | Trouble pronouncing | 7 | 45 | 5 | 52 | 26 | 2 | 60 | 0 | 2 | 0 |
| 2 | Sense of taste | 5 | 36 | 7 | 60 | 14 | 5 | 71 | 0 | 2 | 0 |
| 3 | Painful aching | 0 | 41 | 0 | 57 | 26 | 2 | 62 | 0 | 12 | 0 |
| 4 | Uncomfortable to eat | 0 | 33 | 2 | 55 | 17 | 12 | 71 | 0 | 10 | 0 |
| 5 | Self-conscious | 2 | 67 | 5 | 31 | 36 | 2 | 55 | 0 | 2 | 0 |
| 6 | Felt tense | 2 | 55 | 7 | 41 | 41 | 5 | 45 | 0 | 5 | 0 |
| 7 | Diet unsatisfactory | 2 | 64 | 2 | 36 | 50 | 0 | 36 | 0 | 10 | 0 |
| 8 | Interrupted meals | 0 | 29 | 2 | 57 | 26 | 14 | 36 | 0 | 36 | 0 |
| 9 | Difficult to relax | 2 | 62 | 9 | 33 | 43 | 5 | 43 | 0 | 2 | 0 |
| 10 | Embarrassment | 2 | 72 | 2 | 21 | 52 | 7 | 38 | 0 | 5 | 0 |
| 11 | Irritability | 5 | 69 | 10 | 26 | 50 | 5 | 36 | 0 | 0 | 0 |
| 12 | Difficulty doing usual jobs | 7 | 88 | 29 | 10 | 48 | 2 | 17 | 0 | 0 | 0 |
| 13 | Life satisfaction | 5 | 74 | 33 | 24 | 50 | 2 | 12 | 0 | 0 | 0 |
| 14 | Unable to Function | 29 | 93 | 57 | 7 | 12 | 0 | 2 | 0 | 0 | 0 |
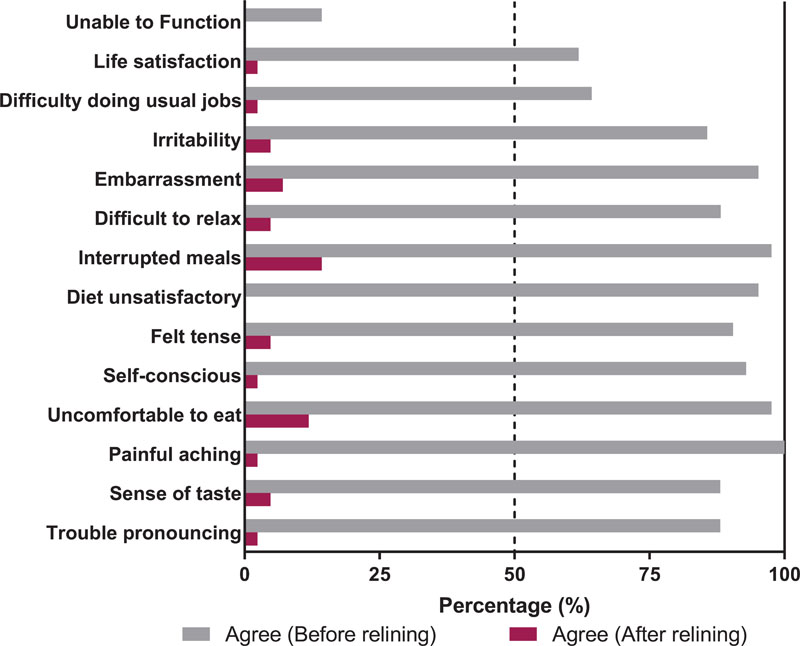
As evident in Fig. (1), the patients experienced improvement on all counts with the usage of the relined denture. In absolute numbers, the highest improvements (% of patients) were noted regarding painful aching of tissues (improved from 100% to 2.4%), unsatisfactory diet (95% to 0%) and self-consciousness (93% to 2.4%) Furthermore, regarding the ability of patients to function with dentures, all patients noted improvement after relining (14.3% to 0%).
The differences between the results obtained from the surveys before and after relining, can be expressed as Z scores, or standards scores, to statistically evaluate the significance of these differences, and the probability of them occurring by chance (Table 2). Based on the results observed, the overall effect was confirmed to be occurring not by chance but due to the positive outcomes attributable to treatment performed i.e., soft relining.
The Binomial probability (one-sided) tests across the outcome variables were conducted to assess the probability of “never” (experienced the variable) as the response by patients after soft-lined denture usage for one month (Table 3). The results showed that the statistically significant improvement was noted in seven of the fourteen outcomes recorded with the ability to function and difficulty doing usual jobs showing the highest significance (p=0.0000). Other outcomes that showed similar and significant trends included life satisfaction, irritability, embarrassment (p<0.01) and to a lesser extent, unsatisfactory diet and self-consciousness (p<0.05).
| Outcome Variables | Overall Effect | |
|---|---|---|
| 1 | Trouble pronouncing any words | z Ϯ = 5.285, N – Ties = 39, p < .001 |
| 2 | Sense of taste | z Ϯ = 5.470, N – Ties = 38, p < .001 |
| 3 | Painful aching | z Ϯ = 5.680, N – Ties = 41, p < .001 |
| 4 | Uncomfortable to eat any food | z Ϯ = 5.555, N – Ties = 40, p < .001 |
| 5 | Been self-consciousness | z Ϯ = 5.550, N – Ties = 38, p < .001 |
| 6 | Feeling tense | z Ϯ = 5.502, N – Ties = 41, p < .001 |
| 7 | Diet been unsatisfactory | z Ϯ = 5.722, N – Ties = 42, p < .001 |
| 8 | Interrupted meals | z Ϯ = 5.461, N – Ties = 39, p < .001 |
| 9 | Difficulty to relax | z Ϯ = 5.509, N – Ties = 40, p < .001 |
| 10 | Embarrassment | z Ϯ = 5.484, N – Ties = 38, p < .001 |
| 11 | Irritability | z Ϯ = 5.488, N – Ties = 38, p < .001 |
| 12 | Difficulty doing usual job | z Ϯ = 5.293, N – Ties = 35, p < .001 |
| 13 | Life in general less satisfying | z Ϯ = 5.350, N – Ties = 38, p < .001 |
| 14 | Totally unable to function | z Ϯ = 5.260, N – Ties = 30, p < .001 |
| Outcome Variables | Observed k | Expected k | Assumed % | Observed % | Probability of the Outcome | |
|---|---|---|---|---|---|---|
| 1 | Trouble pronouncing | 19 | 21 | 0.5 | 0.45238 | Pr(k ≥ 19) = 0.779600 |
| 2 | Sense of Taste | 15 | 21 | 0.5 | 0.35714 | Pr(k ≥ 15) = 0.978221 |
| 3 | Painful Aching | 17 | 21 | 0.5 | 0.40476 | Pr(k ≥ 17) = 0.917925 |
| 4 | Uncomfortable to eat | 14 | 21 | 0.5 | 0.33333 | Pr(k ≥ 14) = 0.990240 |
| 5 | Self-conscious | 28 | 21 | 0.5 | 0.66667 | Pr(k ≥ 28) = 0.021779* |
| 6 | Felt tense | 23 | 21 | 0.5 | 0.54762 | Pr(k ≥ 23) = 0.321984 |
| 7 | Diet unsatisfactory | 27 | 21 | 0.5 | 0.64286 | Pr(k ≥ 27) = 0.044215* |
| 8 | Interrupted Meals | 12 | 21 | 0.5 | 0.28571 | Pr(k ≥ 12) = 0.998556 |
| 9 | Difficult to Relax | 26 | 21 | 0.5 | 0.61905 | Pr(k ≥ 26) = 0.082075 |
| 10 | Embarrassment | 30 | 21 | 0.5 | 0.71429 | Pr(k ≥ 30) = 0.003958** |
| 11 | Irritability | 29 | 21 | 0.5 | 0.69048 | Pr(k ≥ 29) = 0.009760** |
| 12 | Difficulty doing usual jobs | 37 | 21 | 0.5 | 0.88095 | Pr(k ≥ 37) = 0.000000*** |
| 13 | Life satisfaction | 31 | 21 | 0.5 | 0.7381 | Pr(k ≥ 31) = 0.001444** |
| 14 | Unable to Function | 39 | 21 | 0.5 | 0.92857 | Pr(k ≥ 39) = 0.000000*** |
4. DISCUSSION
The degree to which compromised oral health impedes a patient’s normal life and social functioning can be assessed using the oral health-related quality of life [12-15]. In this study, a customised version Oral Health Assessment Index OHIP14-EDENT questionnaire (OHRQoL) was used to evaluate the impact of mandibular denture soft relining on important attributes of a successful denture including patient satisfaction and better perceived oral health-related quality of life [12]. This survey is specifically designed for oral conditions and contains different parameters, such as oral pain, function, and psychological and social aspects when compared to the more general quality of life questionnaires.
Comfort, stability, retention, ability to chew and function, ability to speak normally, and aesthetics of the denture, are the main attributes of an optimal prosthetic replacement, with more acceptance from the wearers [16, 17]. These factors are the major sources of dissatisfaction and complaints from patients due to pain, excessive pressure, maladaptation, poor function and appearance [14]. In this study, denture relining with a soft liner material has significantly improved patient QoL in all of the outcome variables measured. Specifically, in terms of the ability to pronounce words and ease of general phonetics, which may be compromised by poorly fitting dentures, patients reported a significant positive effect of denture relining with the soft liner material. Before denture relining, 26 out of 42 patients (61.9%) reported having difficulties with pronunciation fairly or very often. Following the denture relining, there was a statistically significant improvement in the patients’ perception of their ability to pronounce words, where 97.6% of patients never or hardly ever experienced problems with pronunciation, and only 1 out of 42 patients reported having occasional problems with pronunciation. These results are consistent with a study by Kimoto et al (2006) that showed improvements in chewing comfort and ability, eating enjoyment, food choices, security and ease of speaking and pronunciation, after denture relining [9]. While 48% of patients still experienced difficulty with pronouncing some words, all of the patients were satisfied with their level of speech [9].
A clear improvement was noted in the sense of taste, and an alleviation of discomfort when eating. Before denture relining, 34 patients out of 42 (80.9%) found it uncomfortable to eat with their denture and 73.4% felt their ill-fitting denture altered their sense of taste. One month following the treatment, less than 5% of patients felt that their sense of taste had not improved, and close to 12% occasionally felt uncomfortable eating. However, no participants reported that they felt their dentures contributed to difficulties with eating.
When asked about the frequency of meals being interrupted because of problems with their dentures and the impact on their diet, prior to re-lining, close to 3 out of 4 patients had to regularly and 1 in 4 occasionally interrupt their meals, while 45.2% felt their dentures regularly contributed to a poor diet while 50% felt their dentures caused them to occasionally change their diet. There was a significant improvement following the treatment, with only 14.3% reporting that they still had to occasionally interrupt their meals because of issues with their dentures, and all patients were satisfied with the quality of their diet.
Almost all participants (97.6%) reported no or minimal pain or sore areas in the oral cavity after denture relining, whereas 73.8% had reported soreness and aching fairly or very often before relining and 26.2% had reported occasional pain. These pain results are similar to those reported by Kimoto et al. (2006) [9].
The findings of this study regarding the psychological domain of denture wearing also showed noticeable improvements in patient satisfaction levels. Prior to relining 96.5% of patients were self-conscious about their dentures at some point in time, while 90.5% felt tense because of their dentures. After denture relining a significant improvement in these two outcomes was observed, with only 1 (2.4%) patient feeling occasionally self-conscious and 2 (4.8%) patients feeling occasionally tense due to their dentures after treatment.
Similar results were seen in regard to patients being embarrassed (95.2%) or irritable (85.7%) at some point in time because of problems with their dentures. One month after denture relining, 92.9% and 95.2% respectively, of the participants reported that they had not felt embarrassed or irritable due to their dentures. This corroborates the results of a previous study, where all of the patients reported a reduction in embarrassment, and 93% of patients reported a reduction in irritability [8].
The summative measures of life satisfaction and ability to function with their dentures also showed marked improvement at the end of the study period. Initially, 61.9% of participants felt that their dentures negatively impacted their satisfaction with their life, and 24.3% felt they were unable to fully function because of issues with their dentures. At the end of the study, only 1 patient felt that their dentures occasionally impacted their quality of life and no patients felt their dentures impacted their ability to function.
The results of this study investigating mandibular denture relining with a soft-liner material, have shown significantly higher overall satisfaction with their dentures and the impact on their lives, and a positive impact in terms of mastication, speech, pain the psychological aspects of wearing a denture.
There were some limitations in this study particularly due to the relatively small number of participants. Furthermore, the follow-up questionnaire was completed after one month of relined denture usage which can be only considered to be short-term effects of the treatment.
CONCLUSION
This pilot study has highlighted that soft reliner application can significantly enhance the function aesthetics and multiple domains of quality of life and overall satisfaction in edentulous patients. It would be beneficial to administer this questionnaire within the same subjects to assess the long-term effect. Additionally, long-term studies utilising randomized control trial design, involving a larger sample population and multiple timepoints throughout the intended service i.e., 12-18 months are required in the future.
LIST OF ABBREVIATIONS
| OHRQoL | = Oral Health-Related Quality of Life |
| SPSS | = Statistical Package for the Social Sciences |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval (H-2-015-0128) was obtained by the Human Research Ethics Committee of the University of Newcastle, Australia.
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All human procedures were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent has been taken from the patients included in this study.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of this study are available within the article.
FUNDING
No funds were used for this research, there are no funding conflicts to declare.
CONFLICT OF INTEREST
Dr. Dileep Sharma is the Editorial Board Member of The Open Dentistry Journal.
ACKNOWLEDGEMENTS
Declared none.


