Hyperplastic Pulpitis Management with Endocrown: A Case Report
Abstract
Background:
Pulp polyp (PP) or pulp hyperplasia is a type of irreversible pulpitis that occurs more frequently in young teeth. It is characterized by an exophytic proliferation of granulation tissue with a pinkish-red colour and fibrous consistency, usually asymptomatic.
Case Presentation:
Conservative approach for a PP in a young permanent lower molar using orthograde root canal treatment and subsequent endocrown placement with a 6-month follow-up. A detailed clinical history was carried out, as well as a radiographic study of the lesion, palpation and pulp sensitivity tests. The clinical diagnosis was pulp hyperplasia or PP, confirmed by histopathological analysis.
Results:
Treatment of this case required four appointments: surgical excision of the PP, cleaning and shaping of the root canal system, three-dimensional filling of the canals, cementation and adjustment of the endocrown, thereby achieving remission of symptoms and restitution of chewing function.
Conclusion:
Conservative treatment is a reproducible procedure that has shown satisfactory results in the lower first molar with the presence of a PP.
1. INTRODUCTION
Pulp polyp (PP) or pulpal fibrous hyperplasia refers to irreversible pulpitis. It usually presents asymptomatically, although pain and bleeding on mastication are also described. It is often triggered by the presence of an open cavity (usually caused by caries) and a chronic stimulus [1]. PP vary in size, ranging from a virtually imperceptible lesion to extending beyond the tooth boundary. PPs are more frequently observed in young patients with high reactive capacity and a large pulp cavity, which may be due to the rich blood supply and abundant lymphatic drainage [2]. Histologically, the granulation tissue proliferates and becomes pink to reddish in colour (depending on the degree of fibrosis) and sometimes appears covered by a stratified surface epithelium. Although its incidence is low, numerous cases of this pathology have been reported in recent decades, especially in children, adults, and even infants [3]. PP can occur in deciduous and permanent dentitions. In some cases, two PPs have occurred bilaterally in the same patient [4], and three pulp polyps have even been described in different teeth at the same time [5]. The presumptive diagnosis is clinical and radiographic, although it must be confirmed by histopathological study.
Extraction of molars in young patients can trigger the development of malocclusions and cause functional, aesthetic and phonetic problems. The treatment of choice for a PP currently consists of its complete removal, sending the removed tissue for anatomopathological study, and performing root canal treatment if the apex is formed, although various authors have reported good clinical results by performing a pulpotomy [6, 7].
Regarding the final restoration, amalgam fillings, resin fillings, and posts with crowns have been used [7,8], and, to date, no author has previously described a case of a PP rehabilitated with an endocrown.
This clinical case aimed to present a conservative approach to a pulp polyp in a young permanent lower first molar. To manage this objective, root canal treatment was carried out followed by endocrown placement. A 6-month follow-up appointment was then made to check that the treatment had been successful and that the tooth could remain in the arch, thus avoiding or delaying its extraction and subsequent fitting of a prosthesis. This article has been elaborated following the CARE guidelines for case reports [9].
2. CASE REPORT
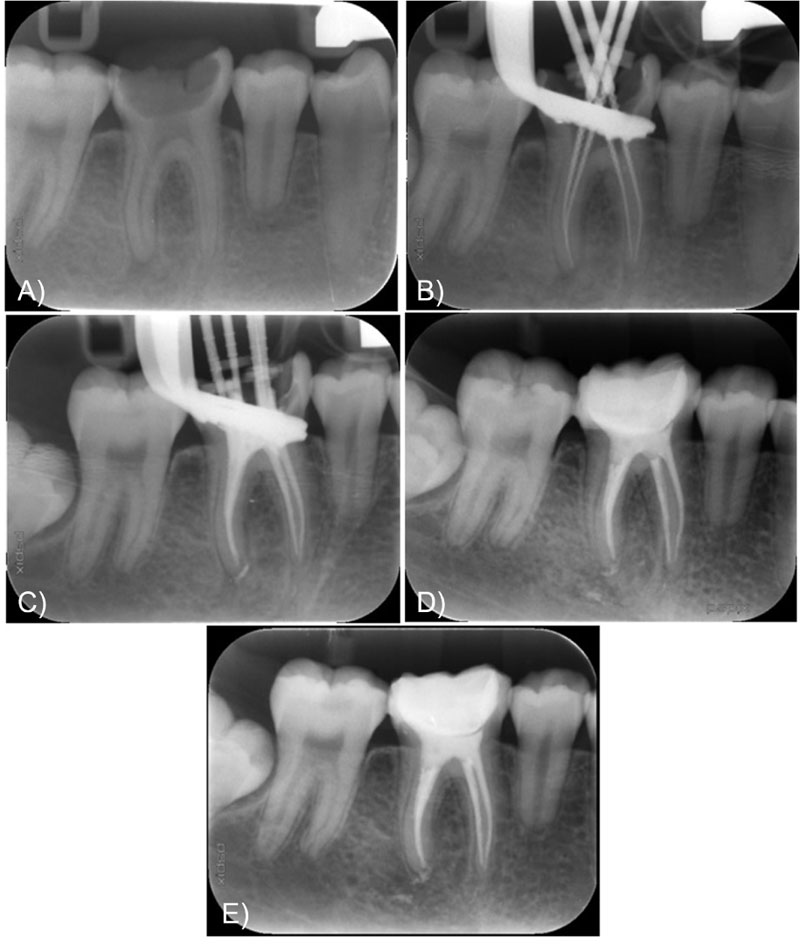
The bioethics committee of the University of Santiago de Compostela gave consent for its execution (Ref USC-33/2020). A 14-year-old female patient was referred to the Master's Degree in Oral Medicine, Oral Surgery and Implantology of the University of Santiago de Compostela for dental extraction of the lower right first molar (4.6) with the presence of a PP occupying the entire occlusal surface of the molar. The patient had no medical history of interest and was not receiving any medication. The reason for consultation was, “It hurts a lot when I bite, and my face has been swollen for a few weeks.” In the extraoral examination, no anomaly was observed at the time; in the intraoral examination, she presented gingivitis and a considerable accumulation of tartar. Regarding the lower right first molar, severe coronal hard tissue destruction was observed and the occlusal surface of the tooth consisted of the soft tissue of PP, and no fistulous tracts were detected on the adjacent mucosal surfaces. The patient could neither occlude nor achieve a stable maximum intercuspidation as there was a first contact between the upper occlusal surfaces and the pulp hyperplasia of the lower molar. This contact caused severe pain in compression. Thermal tests were carried out by applying a chemically cooled cotton ball at -50ºC with tweezers, which were positive, and percussion tests on the axial surfaces of the tooth, which were also positive indicating that vital pulp tissue persisted in the molar. No probing depths greater than 3 millimetres were observed. Radiological findings showed an apical focus in the distal root of the molar. Based on clinical and radiographic techniques, the presumptive diagnosis was hyperplastic irreversible pulpitis or PP. Signed informed consent (IC) was obtained from the legal guardian.
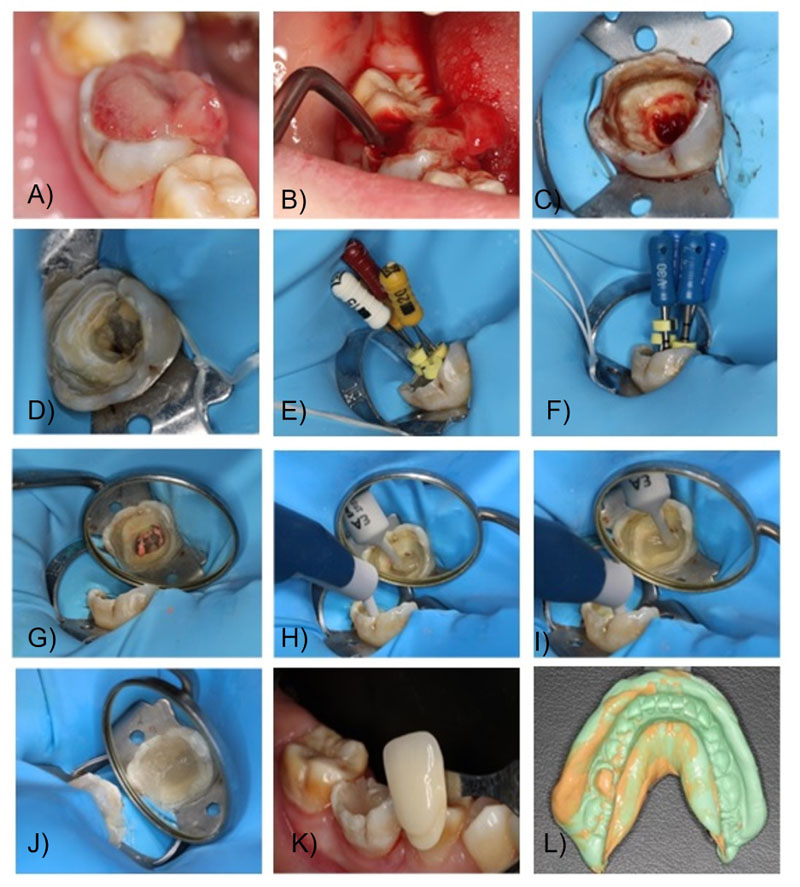
The tissues were anaesthetised using locoregional techniques: nerve block of the inferior dental nerve with vestibular and intrapulpal reinforcement with 3% articaine with epinephrine (1:100000). The PP was excised with a surgical curette until the entire lesion was removed, leaving the hard tissues of the tooth intact. The extracted tissue was immediately stored in a jar with 10% formalin, and the sample was sent to the Department of Pathological Anatomy of the University Clinical Hospital of Santiago. Complete isolation was then carried out with a rubber dam, and the canals were located and permeabilised with K10-K15 hand files. The molar was temporarily obturated with cotton wool and Fermin (Detax, Germany). Histological analysis revealed granulation tissue with an ulcerated surface, devoid of lining epithelium, with many vessels (angiogenesis), polymorphonuclear neutrophils, lymphocytes, mononuclear plasma cells and fibrin. These histological findings are not pathognomonic of PP but are characteristic of all inflammatory processes (Fig. 1). On the second visit, after the signs and symptoms had subsided, the provisional material was removed, and conductometry was carried out with manual files and the Root ZX mini electronic apex locator (Morita, Japan). The working length of the four canals was 18mm. Instrumentation was performed with Protaper Next (Maillefer instruments, Switzerland) up to the X3 file, with irrigation with 5.25% sodium hypochlorite activated ultrasonically. Final irrigation was performed with sodium hypochlorite at the same concentration, 17% ethylenediaminetetraacetic acid (EDTA) and saline. The canals were dried with paper points and then checked with V30 testers that both the previously obtained working length and the smaller diameter of the apical constriction were correct before obturation. AH Plus sealing cement (Dentsply, Germany) was introduced with paper tips, and all four canals were obturated with Thermafil (Maillefer instruments, Switzerland). Finally, both channels' entrance and chamber floor were sealed with Wave fluid composite (SDI, Australia), before cavity preparation for indirect restoration.
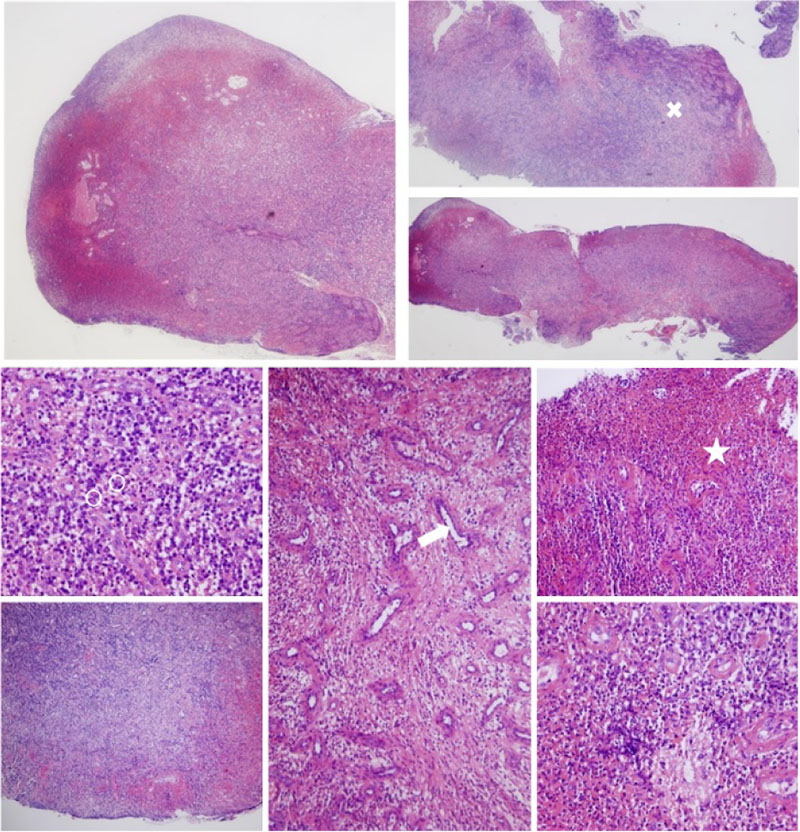
X- collagen formation
OO neutrophilic polymorphonuclears
-> blood vessel
* fibrin
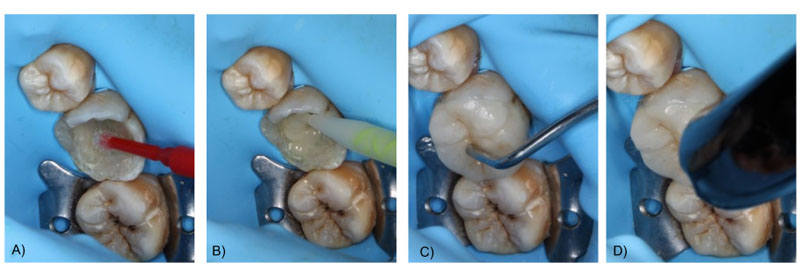
On the third visit, the colour was selected, and the crown was minimally milled. This was followed by a one-step impression of the lower arch with heavy and flowable silicone, an impression of the antagonist arch with alginate and an occlusal registration with Occlufast Rock (Zhermack, Italy). Photographs of the procedure can be seen in Fig. (2). On the fourth visit, after receiving the resin endocrown from the laboratory, fitting was checked before being bonded to the tooth structure. Once the adjustment had been verified, the endocrown was cemented using a dual adhesive and Variolink resin cement (Ivoclar Vivadent, Madrid), applying a thin layer of glycerine to promote final light-curing. Subsequently, its adaptation was checked once cemented, and a minimal occlusal adjustment was carried out. Finally, a control radiograph was taken to check the internal fit of the framework to the remaining tooth tissue and the periradicular status. The radiographs of the complete treatment (and six months control) can be seen in Fig. (3). Also clinical images of the cementation procedure and the 6-month follow-up appointment can be seen in Fig. (4) and Fig. (5) respectively.
3. RESULTS AND DISCUSSION
An endocrown is a fixed prosthesis that covers the entire occlusal surface of the tooth and is bonded with resin cement to the tooth structure, taking advantage of the inside of the tooth to increase the bonding surface. This type of restoration can be made of feldspathic ceramics, lithium disilicate or different types of composite resins, and its main indication is the restoration of teeth with a large loss of tooth structure that retains their axial walls [10, 11]. For the definitive restoration of this molar, whose crown remnant was reduced to the axial walls with a minimal layer of dentine and enamel thickness, there are different therapeutic alternatives: direct reconstruction with hybrid composite with nanometric and micrometric particles (providing hardness, durability and acceptable aesthetics), indirect reconstruction, or a full veneer crown. Once the restorative technique has been selected, the most appropriate material is chosen according to the case.

We now know resin materials have a high long-term clinical performance in rehabilitating posterior teeth, whether used in direct or indirect restorations. The choice of the direct or indirect method remains subjective, and the technique should be chosen on an individual basis, as it has been observed that there are no significant differences in short- and long-term success rates that would indicate the superiority of one technique over the other [8, 9]. However, it has been observed that the equivalent stresses in molars with direct composite restorations were higher than in those restored with inlays. In addition, inlays guarantee a better seal compared to direct restorations and the risk of fractures or cracks due to polymerisation shrinkage is minimised as much as possible as the material is polymerised outside the mouth [12]. A systematic review published in 2019 concluded that an endocrown is a good alternative for restoring endodontically treated molars with extensive loss of tooth structure. The most suitable materials are the new nanocomposite resins and lithium disilicate ceramics [13]. For the reconstruction, in this case, we have opted for a milled resin endocrown, a material that has given good clinical results for large restorations [14]. The endocrown offers multiple advantages over the placement of a full crown [14]. It has been observed that the strength of endodontically treated teeth is reduced due to hard tissue loss, so further reduction of healthy tissue should be avoided when planning the restoration [15]. The advantages of an endocrown over a full veneer crown include greater occlusal thickness (3-7 mm compared to 1.5-2 mm for a conventional crown), better stress distribution as it is a monobloc structure compared to the variety of materials with different moduli of elasticity that make up a conventional restoration, and it does not require minimal ferrule or weakening of the axial walls of the tooth, as it is bonded to the inside of the tooth and does not need to embrace its outer surface. These three characteristics that differentiate them from a conventional restoration with a full veneer crown give them properties that make the available studies support their choice in certain cases. Some authors indicate that endocrowns have higher success rates in terms of fracture resistance, survival and stress distribution in both the restoration and the tooth (particularly in molars, as they receive more axial forces and less lateral forces) [16]. Despite being a relatively recent restoration method, its success rate at 10 years is around 98% of cases [17]. Our results with a six-month follow-up align with the current literature.
CONCLUSION
The definitive restoration with a composite endocrown successfully restores morphology and function to a permanent molar with a closed apex and great coronal destruction, with irreversible hyperplastic pulpitis. The development of new materials, the technological revolution applied to dentistry, and the discovery of new, more reproducible and predictable techniques means it is now possible to adopt a conservative approach to teeth with a compromised prognosis.
LIST OF ABBREVIATION
| PP | = Pulp Polyp |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This case report was approved by the Bioethics Committee of the University of Santiago de Compostela (Ref USC-33/2020).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Signed informed consent was obtained from the legal guardian.
STANDARDS OF REPORTING
CARE guideline has been followed.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
This study was partly funded by a pre-doctoral grant (on a competitive basis) from the Health Research Institute of Santiago de Compostela that was awarded to Alba Perez Jardón.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


