All published articles of this journal are available on ScienceDirect.
A Diagnostic Protocol and Management of Lingual Thyroid: A Case Report
Abstract
Introduction:
The lingual thyroid is a rare embryological abnormality caused by the thyroid's failure to descend from the foramen caecum to its normal prelaryngeal site. Although the ectopic gland at the base of the tongue is usually asymptomatic, it can cause localized symptoms.
Case Presentation:
In this case, we have a 12-year-old male paediatric patient who has hypothyroidism and is experiencing a foreign body sensation. Treatment included partial endoscopic removal via a transoral approach, followed by hormone replacement therapy.
Conclusion:
We highlighted in this article about the differential diagnosis, diagnostic protocols, and therapeutic options.
1. INTRODUCTION
The ectopic thyroid is a rare embryological variation that can occur during thyroid migration, resulting in ectopia. Ectopic thyroid glands are divided into 4 general groups; lingual (at the base of the tongue), sublingual (under the tongue), prelaryngeal (in front of the larynx) and substernal (in the mediastinum) [1, 2].
The lingual thyroid gland can be seen as circumvallate between the papillae, i.e., from the base of the tongue to the epiglottis. Although the prevalence of ectopic thyroid varies between 1: 100,000 and 1: 300,000, the lingual thyroid is the most common. Approximately 400 cases of symptomatic patients have been reported in the literature, but the actual incidence is underestimated due to asymptomatic patients [3]. The lingual ectopic thyroid is a differential diagnosis for swelling at the posterior part of the tongue that the clinician should always explore. Clinical history, basic radiography, and histologic tests can all be used to determine the presence of thyroid ectopia. The main aim of this article is to show the diagnostic pathway and treatment of the lingual thyroid in a pediatric patient with hypothyroidism.
2. CASE PRESENTATION
A 12-year-old boy who has been referred to the dental OPD with complained of swelling at the posterior part of the tongue for the past 3 months. He claims progressive dysphagia due to hard foods and sometimes, dyspnoea. His past medical history was unremarkable. On clinical examination, the swelling was 1cm×2 cm in dimension and appeared to be smooth, reddish mass at the posterior most part of the tongue. On palpation, it was rubbery in consistency and nontender was noted (Fig. 1). There was no palpable thyroid gland noticed in the neck region. Thyroid function tests showed a free triiodothyronine (FT3) of 0.4ng/mL (normal range, 0.6-1.81ng/mL), a free tetraiodothyronine (FT4) of 3.1microgm/dL (normal range, 4.7-11.1microgm/dL), and thyroid-stimulating hormone of 17.848 micro-IU/mL (normal range, 0.35-5.0 micro-IU/mL) which indicates hypothyroidism. Other haematological values were within normal limits. Ultrasonography indicated the absence of a thyroid gland in the neck. Fine needle aspiration biopsy revealed thyroid tissue, i.e., a follicular cavity filled with colloid material, suggesting a lingual thyroid (LT).
In the initial months, the patients were treated with levothyroxine 5 mcg/kg/day, and there was no change in the size of the swelling but symptoms. Therefore, it was decided to remove the mass by surgical method.
A transoral approach was used to accomplish a partial endoscopic surgical excision of the gland while under general anaesthesia. To confirm the diagnosis, the excised sample was sent for histopathological examination. The postoperative course was uneventful and was found to be symptom-free on the fifth day postoperative day, along with levothyroxine 5 mcg/kg/day was prescribed. A follow-up was done on every 1-month, 2-month, and half-year intervals and there was no adverse/ unanticipated event occurred.

The section shows a non-encapsulated collection of embryonic or mature thyroid follicles with colloid and mild inflammation suggestive of lingual thyroid on histopathological examination (Fig. 2).
3. DISCUSSION
The lingual thyroid is a rare developmental anomaly caused by faulty embryogenesis during the foetus intrauterine period [4]. Embryonic development begins approximately 24 days after fertilisation in the primitive hypopharynx floor from the median endodermal thickening, and then the primitive gland descends closely associated with the hyoid bone and laryngeal cartilage. The thyroglossal duct is a thin tube that connects the growing thyroid gland to the tongue. Its involutes about the sixth or eighth week of pregnancy. The opening of the thyroglossal duct in the tongue is known as the foramen caecum. The thyroid gland then descends to meet the lateral ultimo-branchial bodies, which fuse to form the functioning and mature thyroid gland by the third foetal month.
The lingual thyroid is the most common type of ectopic thyroid tissue in the head and neck region, with other areas involved including the trachea, submandibular gland, lateral cervical region, maxilla, palatine tonsils, carotid bifurcation, mediastinum, iris of the eye, pituitary gland, pharynx, trachea, lung, cardiac tissue, heart, ascending aorta, breast, thymus [5-8]. Few researchers believe that genetic factors play a role in thyroid gland morphogenesis and differentiation, specifically the genes of the transcription factors TITF-1 (Nkx2-1), Foxe1 (TITF-2), and PAX-8. If there is a mutation in these genes that causes the developmental abnormality [9]. However, no known gene mutation has yet been linked to human thyroid ectopy.

Around 70% of cases of the lingual thyroid gland are related to cervical athyreosis, while 33% of cases are associated with hypothyroidism [3]. Other diseases that may be associated with the lingual thyroid include thyroid hypofunction or hyperfunction, benign tumours and malignant tumours such as Primary papillary, follicular, mixed follicular and papillary, Hurthle cell tumour and medullary carcinomas, primary B cell lymphoma, and thyroid carcinoma [5, 9-11].
Ectopic thyroid is more prevalent in women than in men, with a female: male ratio ranging from 4:1 to 7:1 [3, 6]. It can strike anyone at any age, but it is most common in the third decade. Because they are asymptomatic, the majority of ectopic thyroid glands do not require therapy. The body's demand for thyroid hormones alters the level of circulating TSH, leading to the formation of ectopic thyroid tissue, which can cause the symptom.
The lingual thyroid is visible on clinical examination as a pink and firm mass near the posterior part of the tongue. Symptoms of thyroid tissue growth include dysphagia (moderate to severe), dyspnea, dysphonia with stomatolalia, Globus pharyngeus, lump-in-throat sensation, persistent cough, sleep apnea, stridor, haemorrhage, and congenital hypothyroidism [12, 13].
Thyroid scan using technetium Tc-99m sodium or iodine-131 or iodine-123 for confirmation of thyroid tissue is the most effective and common diagnostic technique, but ultrasonography, computed tomography, and magnetic resonance imaging will help in determining the boundary and position of the gland [3]. The MRI procedure is more expensive than the CT scan, but exposure to radiation will be less. In the paediatric population, imaging takes longer and may necessitate anaesthetic [9].
Ultrasound should be the initial diagnostic tool used to evaluate the thyroid gland in the neck of children and immunocompromised patients [14] They are noninvasive, low-cost, and capable of detecting an ectopic thyroid. Technetium-99 pertechnetate differs from other isotopes in that it provides higher-quality images while emitting less radiation, making it suitable for use in youngsters. It is also well known for its extended longevity. A common marker, iodine-123, can also be used to screen youngsters, but its use is limited due to its high cost and short half-life period [9]. The surgeon uses angiography to study the patterns of vascularization of the lingual thyroid.
Although fine-needle aspiration cytology or biopsy (FNAC/FNAB) is a reliable diagnostic procedure, there is a risk of bleeding. It is the most accurate method of distinguishing between benign and malignant lesions [9, 15]. Thyroid function tests, which evaluate T3, T4, TSH, and thyroglobulin levels in the blood, are used to determine an ectopic thyroid's functional status [9]. Differential diagnosis of paediatric lingual thyroid includes lymphangioma, minor salivary gland tumors (pleomorphic adenoma), midline branchial cysts, thyroglossal duct cysts, and dermoid cysts which are ruled out shown in Table 1 [6]
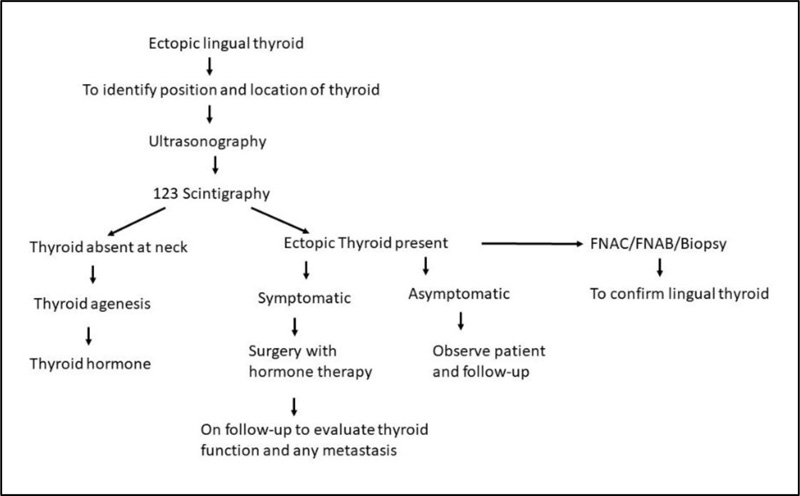
The most successful treatment is determined by the patient's age, location, local symptoms, surgery and anaesthesia risk management, and thyroid functioning status (Fig. 3). Patients who are asymptomatic or euthyroid should be monitored on a frequent basis [3, 16, 17].
The therapy of the lingual thyroid is still controversial. Surgery may be recommended if the lingual swelling is causing considerable problems. There are two approaches for gaining access to the lesion and performing surgery: transoral and external [16].
The transoral method yields a good cosmetic result because there is no external scar on the neck. It does not necessitate the dissection of neck tissue, and the danger of postoperative infection is minimal. This strategy, on the other hand, gives insufficient exposure to large groups. The lingual arteries can cause significant and difficult-to-control bleeding. The transoral procedure is less complicated, less expensive, and requires a shorter hospital stay [9].
| Differential Diagnosis | Clinical Feature | Histologic Feature | Diagnostic Tool |
|---|---|---|---|
| Lymphangioma | • Irregular nodules or pebbly surface • Gray and pink projections • Soft in consistency |
• Multiple intertwining lymph vessel in a loose fibrovascular stroma | • Clinical examination • Histopathology findings • Angiography |
| Minor salivary gland tumors (pleomorphic adenoma) | • Female • Palate is common site |
• Combination of glandular and mesenchyme component • Epithelial component is highly cellular arranged in nest, sheet, cord. • Chondroid, myxoid, Osseous and hyalinised material |
• Clinical examination • FNAC • Histopathology findings • CT & MRI |
| Midline branchial cyst | • Painless submucosal nodule with yellow-white discolouration. • Soft in consistency • Present above the pharyngeal tonsil |
• Stratified squamous or columnar epithelial cystic lining in a lymphoid aggregate • Cystic fluid is foul smelling, cheesy keratinaceous material |
• Ultrasonography • Computed tomography (CT) • Magnetic resonance imaging (MRI) |
| Thyroglossal duct cyst | • Cyst in midline neck mass at or below the level of the hyoid bone. | • Connective tissue contains epithelial lined cyst which is stratified squamous and pseudostratified ciliated columnar epithelium. | • Ultrasonography • Thyroid function test, FNAC, • Radioisotope scanning. • Computed tomography (CT) • Magnetic resonance imaging (MRI) |
| Dermoid cysts | • Painless swelling growing slowly and surrounded by a normal mucosa | • Cyst wall is lined by a stratified squamous epithelium and contains mature epidermal appendages | • Ultrasonography • Computed tomography (CT) • Magnetic resonance imaging (MRI) |
The external approach (midline mandibulotomy and tongue splitting technique) gives good visualization, especially when excising large masses. There is a lower risk of bleeding and can be easily controlled. However, particularly young generations will not accept the scar on the neck. Vascular injury (lingual artery and veins) and nerve injury are the two main risks of surgery (hypoglossal nerve). There may be the formation of a fistula as a complication [3, 9].
Ablative radioiodine therapy is a treatment option for elderly patients or those who are not surgical candidates. This treatment should be avoided in children and young adults because it may harm the gonads or other systems. Although radioactive iodine 131 treatment is an option, it should not be utilised in people who do not respond well to thyroid medication [9].
The present case was approached with partial endoscopic surgical excision of the gland employing transoral methods, in combination with substitutive hormone treatment and a soft diet, maybe the best option in younger patients with extensive lesions in the caudal region of the base of the tongue.
CONCLUSION
The lingual ectopic thyroid is a rare developmental anomaly in the clinician should always consider as a differential diagnosis of swelling in the posterior part of the tongue. The presence of thyroid ectopia can be diagnosed using clinical history, basic radiographic, and histologic analyses. For many patients, conservative management is an ultimate option with surgical intervention for severe symptoms or malignancies. Evaluation of thyroid function is recommended before and after surgery due to the risk of postoperative hypothyroidism.
The treatment of the lingual thyroid has remained controversial, i.e., surgery is recommended in cases with symptoms like severe dysphagia, airway obstruction, etc., and asymptomatic cases are monitored by thyroid profiling check.
LIST OF ABBREVIATIONS
| OPD | = Outpatient department |
| FT4 | = Free tetraiodothyronine |
| FT3 | = Free triiodothyronine |
| TSH | = Thyroid Stimulating Hormone |
| FNAC/FNAB | = Fine-needle aspiration cytology or biopsy |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
Informed written consent was obtained for using patient photographs and data obtained.
STANDARDS OF REPORTING
CARE guidelines and methodology were followed.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


