All published articles of this journal are available on ScienceDirect.
Patient Satisfaction regarding Conventional One-Piece Versus Two-Piece Magnet-Retained Obturator for Patients with Complete Edentulism: A Preliminary Crossover Clinical Trial
Abstract
Purpose:
This study aimed at evaluating patients' satisfaction with conventional one-piece obturators versus two-piece magnet-retained obturators in completely edentulous patient maxillectomy cases.
Materials and Methods:
Ten completely edentulous participants with hemimaxillectomy (8 males and 2 females) were selected in a crossover study. Participants received a conventional obturator one-piece and two-piece obturators connected by magnet attachment in alternate periods (sequences A‐B and B‐A), and outcomes were assessed after 1 week, 3 months, and 6 months Evaluation was made using Obturator Functioning Scale (OFS) and Oral Health Impact Profile for edentulous people (OHIP-EDENT). One way ANOVA test and multivariate analysis of variance with a general linear model with repeated measures was used to test the impact of the group, time, and order on each of the studied scores (α=.05).
Results:
Magnet design showed a statistically significant lower score (P <.050) than the conventional design regarding the overall satisfaction score of OFS along all follow-up periods. Concerning OHIP-EDENT, the magnet design showed a statistically significant lower score (P <.050) than the conventional design regarding total functional limitations, total physical pain, and total social disability along all follow-up periods while for total psychological discomfort, total physical disability, and total handicap, no statistically significant difference was observed between both groups (P >.050).
Conclusion:
Two-pieces magnet-retained obturator could provide better satisfaction and better restoration of orofacial function than the conventional one to manage completely edentulous patients.
Clinical Trial Registration Number:
NCT05066828
1. INTRODUCTION
Satisfactory rehabilitation of maxillary defects of completely edentulous patients is a complicated procedure. As patients not only suffer from the anatomical limitations of having their maxilla resected, the absence of teeth, lack of cross-arch stabilization, inadequate denture-bearing area, lack of favorable tissue undercuts, presence of sensitive nasal mucosa, and the large weight of the prosthesis [1-8] but they also suffer from psychological problems, compromising patients' mastication, deglutition, speech, esthetics, and self-esteem. Satisfactory rehabilitation should allow the patients to return to daily functions and daily routines to resocialize, thus improving patients' satisfaction and quality of life [9-12].
The obturator retention is negatively affected and compromised. The best option for improving these situations is implant placement, which is questionable due to the possibility of lesions recurrence, or patient's rejection for another surgery [13-15]. The procedure involves the available soft-tissue undercuts within the defect, intact side undercut, and scar band in the lateral wall for improving the retention of the obturator [4-8, 14, 15]. Engaging these undercuts is limited by the prosthesis path of insertion and the mouth opening limits [7]. The remaining residual ridge, posterior palatal seal area, perioral musculature, and physical means of retention, such as adhesion, cohesion, atmospheric pressure, and interfacial surface tension, are served as adjunct retentive aids in this design [8, 16].
There is no sufficient evidence regarding the best obturator design for the management of completely edentulous case reports, as well as no randomized controlled trial. Different obturator designs can manage a maxillary defect, a solid bulb obturator, a hollow bulb obturator, or a two-piece obturator [17]. The prosthesis insertion is considered one of the obturator problems due to compromised anatomic morphology in different planes, which may be overcome by two-section obturators (oral and bulb parts); this is mainly indicated by restricted mouth opening [11, 18-20].
Several retentive devices (a lock-and-key mechanism) are available to secure the two sections in position. Among the various retentive devices, magnetic attachments are more applied due to simplicity, more minor complications, less time-consuming, small size, and cost-effective than internal attachments, which require extreme precision and good neuromuscular coordination to insert and use the prosthesis [20-23]. The cytotoxic effects of magnet corrosion products and magnetic field effects are eliminated or decreased in the closed field inside the obturator bulb rather than open-field magnetic systems [24, 25]. The disadvantages of magnetic attachments are less resistance to lateral stress and the possible loss of magnetism during a function for a long period. Nevertheless, they can be magnetized with reasonable ease and induced to function immediately [22].
Several materials have been used for obturator fabrication, such as silicone material, cold-cured resilient acrylic, and heat-cured resilient acrylic. The silicone material is biologically acceptable, hygienic, resilient, easy to handle, and well tolerated by intraoral tissues. However, it has limitations, such as the increased weight, cannot be hollowed out, and being expensive [25, 26]. Cold-cured resilient acrylics showed leaching out of the plasticizers, which would have resulted in the obturator becoming hard after a period of wear intraorally and liable for Candida infection. In comparison, heat-cured resilient acrylic has been proven to be one of the most durable tissue-compatible materials without leaching out of plasticizers that maintain material flexibility for a significantly longer duration [20]. Heat-cured resilient acrylic has plasticized ethyl methacrylate polymers that bind the plasticizers to the methacrylate, hence eliminating the problem of plasticizers leaching out and keeping the material resilient for a significantly longer duration [20].
Flexible or resilient materials permit the engagement of both bony and soft tissues undercuts more profoundly [27, 28]. Flexible material provides better contact with the surrounding mucosa, no injury, improves retention, and provides a better oronasal seal and patient comfort. It provides a cushion effect and favorable load distribution than a conventional hard acrylic prosthesis [11, 25], eliminating the pain associated with a conventional hard acrylic prosthesis [21, 29, 30]. Closed direct contact between the resilient obturator bulb and the residual tissues improves the obturator retention as well as patients' comfort [27, 28, 31-33].
Maxillectomy management aims to minimize facial deformity, restore oral function, and preserve psychological well-being [23, 34, 35]. Recent studies on QOL (quality of life) of maxillectomy patients reconstructed with an obturator have shown a strong correlation between obturator function and QOL [12, 35, 36]. Health-related QoL has become one of the primary determinants of outcome after treatment of head and neck cancer, unlike the more traditional survival measures [37]. Quality of life and patient satisfaction are evaluated independently of the clinician by several questionnaires, such as Oral Health Impact Profile for edentulous people (OHIP-EDENT). This depends on the original 49 items of OHIP, and it is adapted for edentulous patients. It aims to detect QOL changes, as influenced by the clinical aspects of edentulism and its treatment [38]. Obturator functional scale (OFS) assesses patients' satisfaction and the quality of their obturator prosthesis. OFS was developed at the Memorial Sloan Kettering Cancer Center (New York, NY, USA) as a means of assessing the self-reported functioning of an obturator. It was designed by Kornblith et al. [35]. The purpose of this clinical trial was to compare the patient satisfaction regarding a one-piece conventional obturator and a two-piece obturator. The research hypothesis was that the two-piece sectional obturator would provide better patient satisfaction and quality of life.
2. MATERIALS AND METHODS
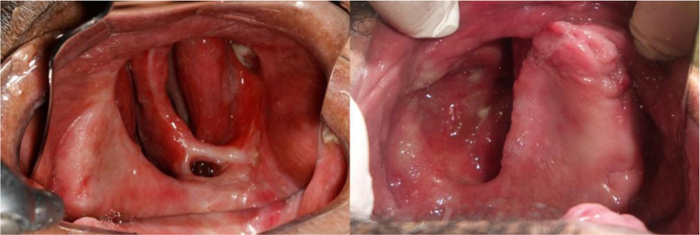
Ten participants (8 males and 2 females) were enrolled in the span of 12 months according to the following criteria: completely edentulous participants with hemimaxillectomy wearing interim or conventional obturators, partially edentulous participants wearing conventional obturators with loose remaining teeth that need an extraction, mouth opening is not less than 25 mm, and intact soft palate, as seen in Fig. (1).
Maxillary cancer is a rare tumor with increased mortality and morbidity. A small sample size (n=5) is a convenient sample and is mostly found in many studies dealing with maxillectomy patients [36].

Participants were included in a randomized crossover study, where two lines of treatment with conventional obturator, one-piece (A) and two-piece obturators connected by magnet attachments (B), were administrated for each participant; two sequences of treatment were used in the crossover study (AB and BA) for 6 months without the need for a washout period. Participants were randomly divided (sealed envelope technique) into 2 equal groups (n=5), where the allocation concealment was done by the chairman (Fig. 2). The study was approved by the research and ethics committee.
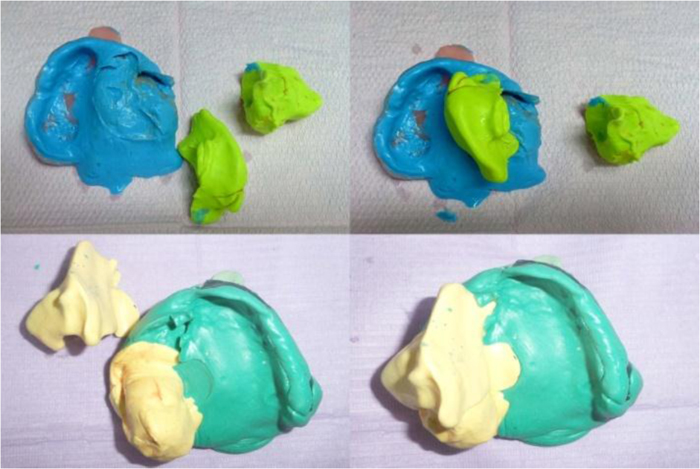
Maxillary and mandibular alginate impressions (Hydrogum 5; ZhermackSpA) were made (after modifying the maxillary stock tray) and poured into the dental stones to obtain the study casts. Maxillary custom acrylic resin trays (Acrylic resin; Acrostone Dental & Medical Supplies) were fabricated on the diagnostic casts after blocking out the defect with wax. The tray should be constructed without entering into the defect. Border molding of the special trays was carried out using impression compound (compound sticks; Prevest Direct). Two final impressions were made using a rubber base composite impression (twin stage impression). Putty rubber base (putty; Zhermack zeta plus) was inserted into the defect undercut from one side only, as seen in Fig. (3), then left for setting. Petroleum jelly was applied, and the other side was filled with a putty rubber base to prevent the binding of the two parts of the impressions. After setting an overall impression, medium consistency was made to pick up the two sections of putty rubber base). The impression was removed into three pieces and reassembled outside the patient mouth, as seen in Fig. (4). Boxing and pouring of the impression were carried out.

Occlusal rims and record bases were fabricated. Centric jaw relation was recorded to mount the mandibular cast using the wax wafer technique (the trial denture bases were retained intraoral by adhesive gel (Corega gel)). Acrylic resin semianatomical teeth (20 °) (Acrylic teeth; Acrostone Dental & Medical Supplies) of appropriate shape, size, and shade were selected, and the maxillary anterior was arranged with minimal overjet and overbite [8], while maxillary posterior inclined buccally. Waxing of the trial dentures was completed. The waxed obturators were tried intraoral for verifying phonetics and esthetics, as seen in Fig. (5).

For the two pieces group, the waxed-up obturators were flasked in a special flask. The defect was packed in the order of soft acrylic (Vertex- Dental), an increment of heat-cured acrylic resin (Acrostone Dental & Medical Supplies.), cellophane paper acting as a separator to prevent binding of acrylic resin, and finally, the remaining part of the flask was filled with heat-cured acrylic resin then cured. Finishing and polishing were carried out. The two parts were reassembled outside the patient mouth without magnet attachment to ensure proper adaptation between the two sections. Obturators bulb was adjusted to be inserted with a specific path of insertion without discomfort to ensure that it could fit and engage the soft-tissue undercuts without traumatizing the tissues. Pressure indicating paste was used to determine any undue pressure placed on the surrounding tissues [6]. The patient was taught to insert and remove the bulb section of the prosthesis, as seen in Fig. (6). By connecting the two sections by placing a mark with a white marker at the outer surface of the bulb section and reassembling again to mark on the opposite side, both marks were drilled by a low-speed motor to place both parts of the attachment of the magnets (magnet and keeper)(Dyna magnet system) with self-cure acrylic resin, as seen in Fig. (7). At the insertion visit, the obturators (oral section) were inserted intra-orally by picking up with magnet attachment. The participants were instructed regarding the obturators' oral hygiene measures and how to clean the inner surfaces of the obturator after separating the obturator into two sections, as seen in Fig. (8).



For conventional obturators, the waxed-up final obturators' base was flasked in a special flask. The defect was packed with soft acrylic (Vertex- Dental), and the remaining part was filled with heat-cured acrylic resin (Acrostone Dental & Medical Supplies), then cured, finished, and polished, as seen in Fig. (9). At the insertion visit, the obturators were adjusted to be inserted with a specific path of insertion without discomfort to ensure that they could fit and engage the soft-tissue undercuts without traumatizing the tissues. Pressure indicating paste was used to determine any undue pressure placed on the surrounding tissues [6]. The patient was taught to insert and remove the obturators. The participants were again instructed regarding obturators and oral hygiene measures.

2.1. Patient Evaluation
Patient satisfaction: The questionnaires were administered 1 week, 3 months, and 6 months after prosthesis insertion for all participants. Then after 6 months, the other obturators were inserted, and the same procedures were carried out again. All questionnaires were taken by the same research interviewer (assisted interviewer) from another department, and he was kept unaware of the type of prosthesis.
Two scales were followed in this study, which are:
- 1: The Obturator Functioning Scale: The questionnaires related to “noticeably clasp” were excluded.
- 2: Oral Health Impact Profile for edentulous people (OHIP-EDENT).
All questionnaires were in English and translated during the interview. The patient's responses were recorded on a 5-point Likert Scale. Points 1, 2,3,4, and 5 represent 'not at all difficult,' 'a little difficult,' 'somewhat difficult,' 'very much difficult,' and 'extremely difficult,' respectively.
Numerical data were explored for normality by checking the data distribution and using normality tests (Kolmogorov-Smirnov and Shapiro-Wilk tests). All data showed a normal (parametric) distribution. Data were presented as mean, standard deviation (SD), and 95% Confidence Interval for the mean (95% CI) values. Repeated measures one-way ANOVA test was used to compare groups and study the changes with time within each group. Bonferroni's post-hoc test was used for pairwise comparison. The significance level was set at P <.05. Statistical analysis was performed with IBM SPSS Statistics for Windows, Version 23.0: IBM Corp.
Multivariate analysis of variance was performed using a general linear model with a repeated measure to test the impact of the group, time, and order (conventional magnet or magnet conventional) on each of the studied scores. The time points were defined as repeated measures, while the group and order were entered as independent variables. We reported the overall effect of time, time * group, time * order, and time * group * order for each analysis. In addition, we tested the main effect of group order and the interaction between group and order. Two-sided p values less than 0.05 were considered statistically significant. All statistical calculations were done using the computer program SPSS (Statistical Package for Social Science; IBM Corp, Armonk, NY, USA) release 15 for Microsoft Windows.
3. RESULTS
Demographic data: Ten patients were treated by maxillectomy during the study period and divided into two equal groups, each one consisting of 4 males and 1 female (Table 1).
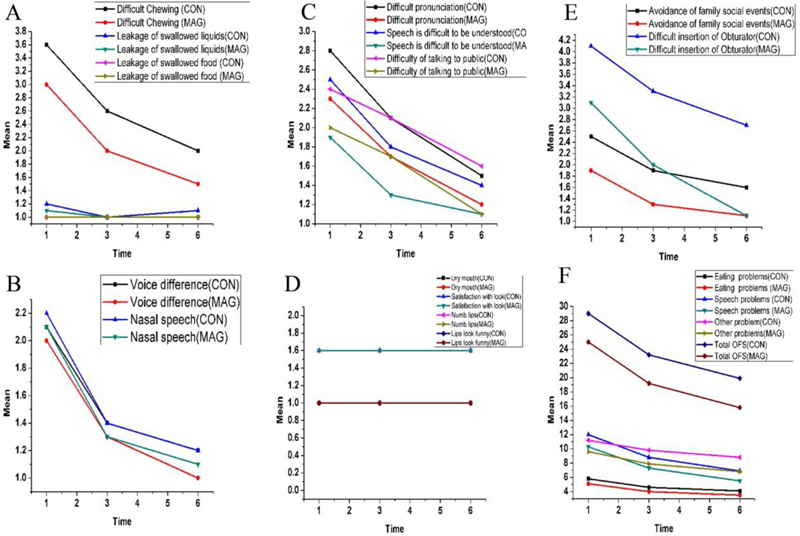
3.1. Obturator Functional Scale
The magnet design showed a statistically significant lower score (P<0.050) than the conventional design regarding the difficulty in chewing, difficulty talking in public, avoidance of family social events, difficulty in the insertion of the obturator, other problems scales, and overall score along all follow-up periods. While facing difficulty in pronunciation, difficulty in understanding the speech, and other speech problems, the magnet design showed a statistically significant lower score (P<.050) than the conventional design at 1 week and 3 months. The magnet design showed a statistically significantly lower score (P <.050) than the conventional design regarding eating problems at 3 and 6 months post-insertion (Table 2), as shown in Fig. (10).
| Patient characteristics | (n = 10) N (%) |
| Gender | Male 8 (80%) |
| Female 2 (20%) | |
| Age in years (Range 47–65) | Mean 57.5 +- (5.72) |
| 47–50: 1 (10%) | |
| 50–55: 3 (30%) | |
| 55–60: 3 (30%) | |
| 60–65:3 (30%) | |
| Marital status | Single 0 (0%) |
| Married 8 (80%) | |
| Divorced 0 (0%) | |
| Widowed 2 (20%) | |
| Educational status | |
| No graduation 2 (20%) | |
| Basic school 3 (30%) | |
| University- or technical college entrance diploma 5 (50%) | |
| Employment status | |
| Retired 4 (40%) | |
| Not retired 5(50%) | |
| Housewife 1(10%) | |
| Living place | Town 6 (60%) |
| Village 4(40%) |
| - | Conventional | Magnet | P-VALUE | F- value | Df | 95%Confidence interval for mean | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| value | ||||||||||
| - | Mean | SD | Mean | SD | Lower bound | Upper | ||||
| Bound | ||||||||||
| 1 | Difficult Chewing- | 3.6 | 0.516 | 3 | 0.00 | .001* | 13.499 | 19 | --0.942 | 0.257 |
| at 1week post insertion | ||||||||||
| 1 | at 3 months post insertion | 2.6 | 0.516 | 2.0 | 0.00 | .001* | 13.499 | 19 | -0.942 | -0.257 |
| 1 | at 6 months post insertion | 2.00 | 0.00 | 1.5 | 0.527 | .007* | 9.000 | 19 | -0.850 | -00.149 |
| 2 | Leakage of swallowed liquids | 1.2 | 0.421 | 1.10 | 0.316 | .555 | 0.36 | 19 | -0.449 | 0.249 |
| at 1week post insertion | ||||||||||
| 2 | at 3 months post insertion | 1.0 | 0.00 | 1.0 | 0.0 | 1.0 | NaN | 19 | 0.00 | 0.00 |
| 2 | at 6 months post insertion | 1.1 | 0.316 | 1.0 | 0.0 | .330 | 0.999 | 19 | -0.109 | 0.309 |
| 3 | Leakage of swallowed food- at 1week post insertion | 1.00 | 0.0 | 1.00 | 0.0 | 1.0 | NaN | 19 | 0.00 | 0.000 |
| at 1week post insertion | ||||||||||
| 3 | at 3 months post insertion | 1.00 | 0.0 | 1.00 | 0.0 | 1.0 | NaN | 19 | 0.00 | 0.000 |
| 3 | at 6 months post insertion | 1.00 | 0.0 | 1.00 | 0.0 | 1.0 | NaN | 19 | 0.00 | 0.000 |
| Eating problems1week post insertion | 5.6 | 0.843 | 5.1 | 0.316 | .017* | 6.784 | 19 | -1.098 | 0.098 | |
| at 3 months post insertion | 4.6 | 0.516 | 4 | 0.00 | .001* | 13.499 | 19 | -0.942 | -0.257 | |
| at 6 months post insertion | 4.1 | 0.316 | 3.5 | 0.277 | 0.006* | 9.52 | 19 | 0.879 | -0.320 | |
| 4 | Voice difference- at 1week post insertion | 2.1 | 0.316 | 2.0 | 0.00 | .330 | 0.999 | 19 | -0.309 | 0.109 |
| 4 | at 3 months post insertion | 1.40 | 0.516 | 1.30 | 0.483 | .660 | 0.200 | 19 | -0.569 | 0.369 |
| 4 | at 6 months post insertion | 1.2 | 0.421 | 1.0 | 0.00 | .150 | 2.250 | 19 | -0.479 | 0.079 |
| 5 | Nasal speech- at 1week post insertion | 2.2 | 0.421 | 2.1 | 0.316 | .555 | 0.360 | 19 | -0.249 | 0.449 |
| 5 | at 3 months post insertion | 1.4 | 0.516 | 1.3 | 0.483 | .660 | 0.200 | 19 | -0.569 | 0.369 |
| 5 | at 6 months post insertion | 1.2 | 0.421 | 1.10 | 0.316 | .555 | 0.360 | 19 | -0.449 | 0.249 |
| 6 | Difficult pronunciation- at 1week post insertion | 2.8 | 0.421 | 2.3 | 0.483 | .023* | 6.081 | 19 | -0.925 | -0.074 |
| 6 | at 3 months post insertion | 2.1 | 0.316 | 1.7 | 0.483 | .041* | 4.799 | 19 | -0.783 | -0.016 |
| 6 | at 6 months post insertion | 1.50 | 0.527 | 1.2 | 0.421 | .176 | 1.975 | 19 | -0.748 | 0.148 |
| 7 | Speech is difficult to be understood- at 1week post insertion | 2.5 | 0.527 | 1.9 | 0.567 | .024* | 6.000 | 19 | -1.114 | -0.085 |
| 7 | at 3 months post insertion | 1.8 | 0.421 | 1.30 | 0.483 | .023* | 6.081 | 19 | -0.925 | -0.074 |
| 7 | at 6 months post insertion | 1.4 | 0.516 | 1.1 | 0.316 | 0.134 | 2.454 | 19 | -0.702 | 0.102 |
| 8 | Difficulty of talking to public- at 1week post insertion | 2.4 | 0.516 | 2.0 | 0.0 | .024* | 5.999 | 19 | -0.742 | -0.057 |
| 8 | at 3 months post insertion | 2.1 | 0.316 | 1.7 | 0.483 | .041* | 4.799 | 19 | -0.783 | -0.016 |
| 8 | at 6 months post insertion | 1.6 | 0.516 | 1.1 | 0.316 | .017* | 6.818 | 19 | 0.098 | 0.902 |
| Speech problems at 1week post insertion | 12 | 1.699 | 10.3 | 0.948 | .017* | 6.826 | 19 | -2.992 | -0.407 | |
| at 3 months post insertion | 8.7 | 1.567 | 7.3 | 1.357 | 0.086 | 3.282 | 19 | -2.777 | -0.022 | |
| at 6 months post insertion | 6.9 | 2.024 | 5.5 | 1.269 | .080 | 3.431 | 19 | -2.987 | 0.187 | |
| 9 | Dry mouth- at 1week post insertion | 1.0 | 0.00 | 1.1 | 0.00 | 1.0 | NaN | 19 | 0.0000 | 0.000 |
| 9 | at 3 months post insertion | 1.0 | 0.00 | 1.0 | 0.00 | 1.0 | NaN | 19 | 0.0000 | 0.0000 |
| 9 | at 6 months post insertion | 1.0 | 0.0 | 1.0 | 0.00 | 1.0 | NaN | 19 | 0.0000 | 0.0000 |
| 10 | Satisfaction with look- at 1week post insertion | 1.6 | 0.516 | 1.6 | 0.516 | 1.0 | 0.000 | 19 | -0.484 | 0.484 |
| 10 | at 3 months post insertion | 1.6 | 0.516 | 1.6 | 0.516 | 1.0 | 0.000 | 19 | -0.484 | 0.484 |
| 10 | at 6 months post insertion | 1.6 | 0.516 | 1.6 | 0.516 | 1.0 | 0.000 | 19 | -0.484 | 0.484 |
| 11 | Numb lips- at 1week post insertion | 1.00 | 0.00 | 1.00 | 0.00 | 1.0 | NaN | 19 | 0.000 | 0.000 |
| 11 | at 3 months post insertion | 1.00 | 0.00 | 1.00 | 0.00 | 1.0 | NaN | 19 | 0.000 | 0.000 |
| 11 | at 6 months post insertion | 1.0 | 0.00 | 1.0 | 0.00 | 1.0 | NaN | 19 | 0.000 | 0.000 |
| 12 | Lips look funny at 1week post insertion | 1.0 | 0.00 | 1.0 | 0.00 | 1.0 | NaN | 19 | 0.000 | 0.000 |
| 12 | at 3 months post insertion | 1.00 | 0.00 | 1.00 | 0.00 | 1.0 | NaN | 19 | 0.000 | 0.000 |
| 12 | at 6 months post insertion | 1.00 | 0.00 | 1.00 | 0.00 | 1.0 | NaN | 19 | 0.000 | 0.000 |
| 13 | Avoidance of family social events- at 1week post insertion | 2.5 | 0.527 | 1.9 | 0.567 | .024* | 6.000 | 19 | -1.114 | -0.085 |
| 13 | at 3 months post insertion | 1.9 | 0.567 | 1.3 | 0.483 | .020* | 6.480 | 19 | 0.105 | 1.094 |
| 13 | at 6 months post insertion | 1.6 | 0.516 | 1.1 | 0.316 | .017* | 6.818 | 19 | 0.098 | 0.902 |
| 14 | Difficult insertion of Obturator- at 1week post insertion | 4.1 | 0.316 | 3.1 | 0.316 | .001* | 49.99 | 19 | -1.296 | -0.703 |
| 14 | at 3 months post insertion | 3.3 | 0.483 | 2.00 | 0.471 | .001* | 37.097 | 19 | -1.620 | -0.979 |
| 14 | at 6 months post insertion | 2.7 | 0.483 | 1.10 | 0.316 | .001* | 76.799 | 19 | 1.216 | 1.983 |
| Other problems at 1week post insertion | 11.2 | 1.619 | 9.6 | 0.843 | .006* | 9.602 | 19 | -2.812 | -0.387 | |
| at 3 months post insertion | 9.8 | 1.032 | 7.9 | 1.197 | .003* | 11.402 | 19 | 0.850 | 2.950 | |
| at 6 months post insertion | 8.8 | 1.398 | 6.8 | 0.918 | .001* | 14.977 | 19 | 0.888 | 3.111 | |
| 15 | Overall score at 1week post insertion | 23.2 | 3.259 | 19.9 | 1.663 | .009* | 8.470 | 19 | -5.730 | -0.869 |
| 15 | at 3 months post insertion | 18.5 | 2.505 | 15.2 | 3.190 | .012* | 7.610 | 19 | -5.994 | -0.605 |
| 15 | at 6 months post insertion | 15.7 | 3.301 | 12.3 | 2.110 | .006* | 9.426 | 19 | 0.797 | 6.002 |
| Conventional | Magnet | p-value | F -value | 095%Confidence Interval for Mean | ||||
| Mean | SD | Mean | SD | Lower bound | Upper bound | |||
| Total functional limitations 1 week | 8.4 | 1.505 | 7 | 1.414 | .046* | 4.59375 | -2.7720 | -0.0280 |
| Total functional limitations 3 month | 6.4 | 1.173 | 5 | 1.414 | .026* | 5.802629 | -2.6206 | -0.1794 |
| Total functional limitations 6 months | 5.2 | 1.032 | 4.1 | 1.197 | .041* | 4.839998 | -2.1500 | -0.0500 |
| Total physical pain 1 week | 12.6 | 2.221 | 10.1 | 2.514 | .029* | 5.552813 | -4.7287 | -0.2713 |
| Total physical pain 3 month | 7.6 | 1.646 | 5.8 | 1.549 | .10.021* | 6.339133 | -3.3016 | -0.2984 |
| Total physical pain 6 months | 6.5 | 1.779 | 4.5 | 1.032 | .007* | 9.230772 | -3.3664 | -0.6336 |
| Total psychological discomfort 1 week | 5.1 | 0.994 | 5 | 0.942 | 0.82 | 0.0532544 | -1.0098 | 0.8098 |
| Total psychological discomfort 3 month | 4.5 | 0.722 | 4.2 | 0.918 | 0.423 | 0.669421 | -1.0759 | 0.4759 |
| Total psychological discomfort 6 months | 3.3 | 0.948 | 2.8 | 0.918 | 0.246 | 1.433121 | -0.3767 | 1.3767 |
| Total physical disability 1 week | 7.4 | 1.505 | 7 | 1.333 | 0.537 | 0.395605 | -1.7357 | 0.9357 |
| Total physical disability 3 month | 6.5 | 0.707 | 6.3 | 0.674 | 0.525 | 0.418604 | -0.8490 | 0.4490 |
| Total physical disability 6 months | 5.5 | 1.08 | 5 | 1.414 | 0.385 | 0.789474 | 1.6821 | 0.6821 |
| Total psychological disability 1 week | 5.5 | 1.178 | 5.1 | 1.1 | 0.442 | 0.615385 | -1.4708 | 0.6708 |
| Total psychological disability 3 month | 4.8 | 1.135 | 4.4 | 1.074 | 0.429 | 0.654546 | -1.4381 | 0.6381 |
| Total psychological disability 6 months | 3.8 | 1.033 | 3.2 | 1.032 | 0.21 | 1.687499 | -1.5701 | 0.3701 |
| Total social disability 1 week | 8.5 | 1.429 | 7.1 | 1.449 | .0316* | 5.428952 | -2.7521 | -0.0479 |
| Total social disability 3 month | 7.1 | 1.197 | 5.6 | 1.505 | .023* | 6.081083 | 0.2224 | 2.7776 |
| Total social disability 6 months | 5.4 | 1.074 | 4.1 | 1.197 | .019* | 6.527895 | -2.3684 | -0.2316 |
| Total handicap 1 week | 6.3 | 0.823 | 5.8 | 0.918 | 0.216 | 1.642334 | -1.3191 | 0.3191 |
| Total handicap 3 month | 4.9 | 0.875 | 4.4 | 1.173 | 0.294 | 1.165803 | -1.4722 | 0.4722 |
| Total handicap 6 months | 3.4 | 0.843 | 2.8 | 0.918 | 0.145 | 2.314285 | -1.4280 | 0.2280 |
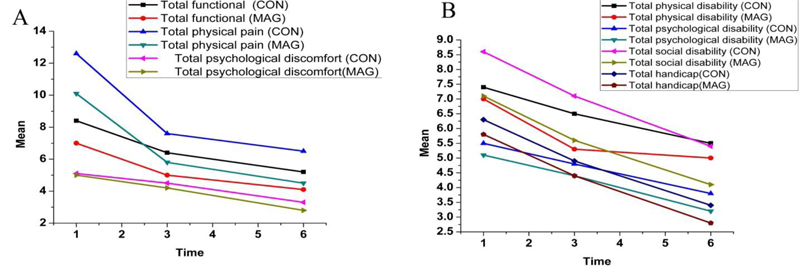
3.2. Oral Health Impact Profile for Edentulous People (OHIP-EDENT)
The magnet design showed a statistically significant lower score (P<.050) than the conventional design regarding total functional limitations, total physical pain, and total social disability along all follow-up periods. There was no statistically significant difference between both groups (P>.050) regarding total psychological discomfort, total physical disability, and total handicap (Table 3), as shown in Fig. (11).
Multivariate analysis of variance was performed to test the effect of group, time, and order on each of our tested scores. Multivariate analysis showed that the effects of order and groups were not significant on time. A significant overall effect of time was observed for all measured parameters except leakage of swallowed liquids, leakage of swallowed food, dry mouth, satisfaction with the look, numb lips, and lips looking funny. However, no significant interaction was observed concerning group or order. In addition, the significant main effect of the group was observed (Difficulty in chewing, difficulty in pronunciation, speech is difficult to be understood, difficulty in talking in public, avoidance of family social events, difficult insertion of the obturator, overall score, total functional limitations, total physical pain, and social disability). In comparison, the order was found to have no effect on the group.
Nearly all patients did not show any complaint except one who mentioned an increase in nasal secretion and corrected after several follow-up visits. Most of the patients preferred the sectional obturators; only one preferred the conventional one.
4. DISCUSSION
Using a sectional obturator is promising regarding improving patients’ satisfaction that supports the study hypothesis.
Poorly retentive and functioning obturators exhibited significant psychological distress that affects orofacial functions (speech, smiling, swallowing, and chewing), which are essential for social interaction and quality of life [35]. In the past, the absence of validated questionnaires was one of the major problems in evaluating the QOL and satisfaction of maxillofacial prosthesis wearers. However, currently, there are several validated questionnaires [35, 38, 39]. The evaluation only included 6 months, which is sufficient as most studies evaluating QOL in patients with head and neck tumors have shown that the most significant QOL changes occur during the first year after diagnosis [40-42]. Our OHIP-EDENT and OFS results disclosed actual significant differences between the two patient groups as the data were recorded after prosthetic rehabilitation. There is a possibility that due to long interval periods between prosthetic rehabilitation and data collection, patients might tend to adapt over time and fail to report deficits, affecting the reality of the result “response shifts” [43].
All participants of both groups showed improved satisfaction levels with their definitive obturators, but with different levels. The satisfaction started from prosthesis insertion time and increased gradually until the end of the study period as patients tend to adapt over time [43]. Most of the patients preferred the sectional obturator. Only one preferred the conventional one. The problems related to swallowing, leakage of liquids, and solid food are mainly affected by the obturator adaptation, the remaining structures, and the degree of separation between the oral and nasal cavities as incompetent separation results in the ingress of fluids and food to the nasal cavity, which are not present due to a resilient, flexible bulb that contacts the soft tissue tightly [21, 33]. The problems related to chewing and functional limitations showed a slight improvement in both groups as resilient obturator bulbs significantly improved masticatory ability in rehabilitated areas, such as the soft, resilient bulb will buffer the mastication forces during chewing, reducing the transmission of forces to the sensitive tissue. Mastication was found to be excellent on the intact side for most of the participants [44]. These problems are mainly affected by the obturator adaptation, which is better in the magnet design due to better stability and retention, which are gained by the small, easily inserted bulb sections that engage the undercuts rather than larger conventional ones, reflecting better results regarding ease of insertion [3, 16, 23, 45].
Speech generally was relatively improved in both groups as speech is an adaptive process. Speech is found to be better in the magnet design due to accurate fit, the obturator adaptation, improved retention, and stability, leading to speaking comfortably [3, 23, 46, 47]. Social interaction and talking in public were improved in the magnet design due to improved retention and stability; considering esthetics and adaptation while designing administrated treatment contribute to treatment success in terms of improvements in the patient’s social life and social well-being [45, 48, 49]. A study conducted by Kornblith et al. revealed that as patient satisfaction with obturator orofacial functions (speech, smiling, swallowing, and chewing) increased, their social adjustment improved, as well as their psychological distress decreased [35].
Regarding handicap, psychological discomfort, and psychological disability, no clinical difference was reported as this might be explained by the nature of most questions related to general aspects of life that could not be altered by prosthesis design. Patients suffering from maxillofacial tumors develop coping strategies to gain a better quality of life after prosthetic rehabilitation. Most of the patients think that being alive outweighs the problems of obturator therapy [50].
Physical pain and sore spots were recorded for both groups until the dentures settled and markedly ended at the second and third evaluation periods. The increased size and weight of the prosthesis, causing soreness and discomfort and periodic recalls, helped the clinician identify the sore spots, and they were corrected [25]. As all selected patients did not receive postoperative radiation, no significant trismus, dryness, and soreness of the oral mucosa were observed [51]. A study conducted by Mittal revealed that obturators of different designs play an essential role in rehabilitating maxillary defects with a satisfactory outcome, and the most satisfactory results were reported with magnet retained, and the least outcome was observed in the conventional obturator group [23].
CONCLUSION
A two-piece magnet-retained obturator could provide better satisfaction and restoration of orofacial function than the conventional one for the management of completely edentulous patients.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the ethics committee of the faculty of dentistry, Cairo University, Egypt 11, ElSaraya street, Almanyal, Cairo, Egypt (Approval no. 214/2018).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures were followed in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written and informed consent was obtained from the participants.
STANDARDS OF REPORTING
CONSORT guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
Data are available from the author upon request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflicts of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We dedicate this work to the spirit of our professor Samira Ibrahim who has helped us from the student level so far greatly throughout her life and we will follow her advice forever.


