All published articles of this journal are available on ScienceDirect.
Management of A Bad Split Complication: A Systematic Review
Abstract
Introduction:
Bad split is one of the well-known intra-operative complications that occur during the bilateral sagittal split osteotomy (BSSO) procedure, which is a rehabilitation procedure for patients with mandibular deformities. The prevention of further post-surgery complications required sufficient management of bad split complications.
Objective:
This study aimed to analyze the management of bad split complications during a BSSO procedure.
Methods:
The literature review was conducted in the form of library research in the field of bad split complications' management by a BSSO based on the Preferred Reporting Items for Systematic Reviews (PRISMA). Related studies were found through using a manual search using Pubmed, ScienceDirect, Ebscohost, Scopus, Medline, Embase, and Web of Science, among other search engines. The inception of incorporation standards, the process of data extraction, and the determination of the risk of bias were carried out by the authors. The process of data screening was conducted by applying the inclusion and exclusion criteria.
Results:
This paper systematically reviewed seven related studies, four of which were case series and two of which were cross-sectional. The utilization of additional osteosynthetic plates was revealed throughout the extraction process as the most acquainted course of action to manage the bad split complications during the BSSO procedure.
Conclusion:
The osteosynthetic plate and miniplate application with bicortical or monocortical screws were exposed as the most used treatment for bad split complications.
1. INTRODUCTION
Dentofacial deformities that need surgical correction affect about 5% of the world's general population through their various degrees of functional and aesthetic problems [1, 2]. Incidences of 0.2% up to 14.6% per split-site have been reported [3]. A therapy combination that mainly consists of orthodontic treatment and orthognathic surgery is mostly needed by patients with moderate to severe deformities to gain optimum oral functions [4]. Orthognathic surgery is an oromaxillofacial surgery that is designed to significantly generate a better appearance and occlusal function for patients [5]. One of the intraoral techniques used in orthognathic surgery is bilateral sagittal split osteotomy (BSSO), a technique that is used to treat various mandibular deformities [6]. The first expert who declared the technique was Obwegeser (1995). Later on, Dal Pont (1961) and Hunsuck (1968) redesigned the technique to minimize potential complications [7]. Our literature review revealed that the BSSO is one of the most popular procedures in orthognathic surgery, amongst other orthognathic surgery techniques [7-9]. This might be due to the fact that it advances as well as positions the mandible in different directions while enhancing its functions and the patient’s appearance [8-10]. Therefore, the BSSO is considered the most logical option when dealing with mandibular deformities compared to other existing techniques [11]. Nevertheless, due to the complexity of the procedure, several complications (intraoperatively and postoperatively) were still found during the BSSO procedure [12].
A retrospective study conducted by Friscia et al. [13] for 10 years in 423 cases regarding complication(s) in BSSO procedure showed that a bad split occurred in eight patients, while a study conducted by Kim and Park [14, 15] revealed that bad split occurred in nine cases (3.85%) among 234 participants. Another study conducted by Veras et al. [14, 16] found 12 cases (10.91%) of a bad split among 110 participants. Furthermore, Chrcanovic et al. [14] reported the incidence of bad split ranging from 0.21% to 22.72% in a review of 21 studies that took place from 1971 to 2010. Additionally, it was revealed that the most common intraoperative complications during the BSSO procedure were excessive bleeding and bad split [12]. A bad split is described as an unfavorable and irregular fracture of the mandible during an osteotomy procedure [14, 17]. The patterns of the split that occurred on a bad split complication were classified based on the location of the fracture, which was then classified into four types, namely fractures of the proximal segment, distal segment, coronoid process, and condylar neck [3]. Considering that a complication during a BSSO procedure, including the bad split complication, can lead to infection, bony fragment sequestration, delay of bone healing, pseudoarthrosis, and mandibular dysfunction caused by temporomandibular joint disturbance [14], correct and proper management is essential. Incorrect and improper management will result in an unstable ossification process and failed unification process of the fracture fragments [18].
Additionally, a study conducted by Vagle et al. showed that patients who had their osteosynthetic device removed, patients who experienced complications of sub-optimal splits, and patients who had post-operative infections showed a tendency to post-operative dissatisfaction. Greater dissatisfaction was reported by patients who experienced persistent postoperative pain [11], indicating the impact of the complication on patients’ daily lives. Based on the fact that bad split complications may lead to further complications that compromise the patients’ quality of life [19], further studies on how to manage bad split complications accordingly are considered to be of importance. Therefore, a systematic review that aimed at understanding how to manage bilateral sagittal split osteotomy during an orthognathic surgery was conducted.
2. MATERIALS AND METHODS
The study was performed according to the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) guidelines. A comprehensive electronic search was conducted from February 2021 up to May 2021. The databases used for searching were as follows: PubMed, ScienceDirect, EBSCOhost, Medline, Embase, Scopus, and Web of Science. The Boolean operators were used to combine the selected keywords by using “AND,” “OR,” or “NOT” in the following order: “(((bad split) OR (bad splits)) OR (unfavorable fracture)) OR (unfavorable fractures) AND ((bilateral sagittal split osteotomy) OR (sagittal split ramus osteotomy)) OR (sagittal ramus osteotomy) AND (((fracture pattern) OR (fracture patterns)) OR (split pattern)) OR (split patterns) AND (((management) OR (treatment)) OR (care)) OR (handling).” All authors (NA, TM, and AT) were involved during the design phase of the study protocol, the setting of the inclusion and exclusion criteria, and the data extraction process. NA and TM then independently performed the critical appraisal process. Any discrepancy issues were addressed through a discussion session that was attended by all authors.
2.1. Eligibility Criteria
Any publication on complication(s) during a BSSO procedure within the last twenty years was included. Only studies with inclusion criteria that adhered to the PICO guideline (participants, intervention, comparison, and outcome) were included. Therefore, in regard to the PICO guideline, only studies that involved patients with a bad split complication during the BSSO procedure were included. Furthermore, the studies included should clearly and specifically mention the management procedure for a bad split complication. Studies included were then screened for duplication, title and abstract suitability, and full-text assessment.
2.2. Quality Assessment
The Joanna Briggs Institute (JBI) Critical Appraisal Tools were used during the quality assessment process. Two different instruments from the JBI were individually used to evaluate the case series and cross-sectional studies. The critical appraisal tool for the case series consisted of ten questions, whilst the critical appraisal tool for the cross-sectional study consisted of eight questions. Each question was answered with closed answers in the form of “yes,” “no,” “unclear,” or “not applicable.”
3. RESULTS
Seven articles that were reviewed in this study were obtained using the PRISMA guidelines. The PRISMA flow diagram of the study is shown in Fig. (1).
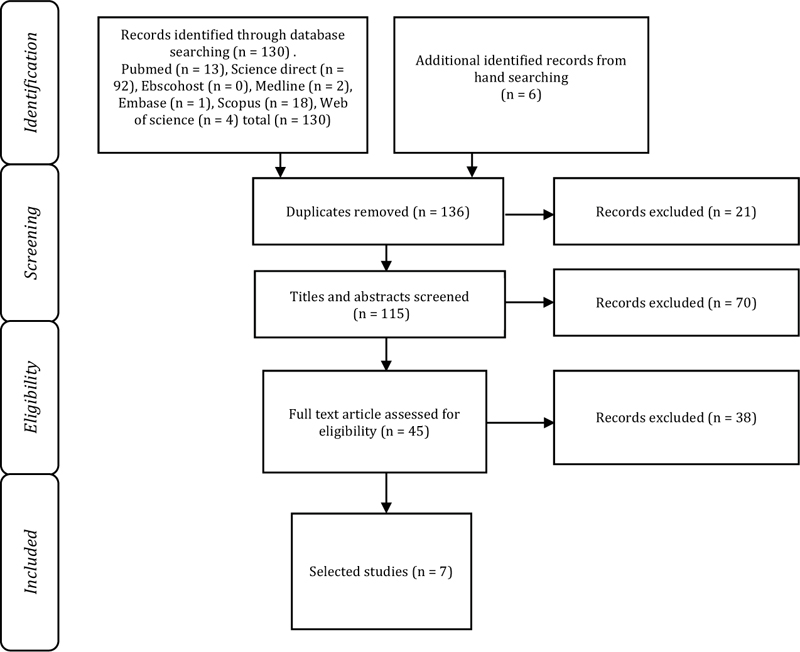
Source: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. DOI: 10.1136/bmj.n71.
3.1. Quality Assessment Result
Based on the JBI critical appraisal tools of the case series category, a study by Falter et al. obtained the highest score with a score of 10 (out of 10; each “Yes” answer scores one point). Meanwhile, in the cross-sectional study category, the highest score was obtained by the Mehra et al. study with a score of 6 (out of 8; each “Yes” answer scores one point). The results of the quality assessment are shown in Tables 1 and 2.
| List of Questions (JBI Critical Appraisal Tools) | Acebal-Bianco et al., 2000 | Borstlap et al., 2004 | Teltzrow et al., 2005 | Falter et al., 2010 | Mensink et al., 2013 |
|---|---|---|---|---|---|
| Were there clear criteria for inclusion in the case series? | Unclear | Yes | Unclear | Yes | Yes |
| Was the condition measured in a standard way for all participants included in the case series? | Yes | Yes | Yes | Yes | Yes |
| Were valid methods used for the identification of the condition for all participants included in the case series? | Yes | Yes | Yes | Yes | Yes |
| Did the case series have consecutive inclusion of participants? | Yes | Unclear | Yes | Yes | Yes |
| Did the case series have the complete inclusion of participants? | Yes | Unclear | Yes | Yes | Yes |
| Was there clear reporting of the demographics of the participants in the study? | Yes | Yes | Unclear | Yes | Unclear |
| Was there clear reporting of clinical information of the participants? | Yes | Yes | Yes | Yes | Yes |
| Were the outcomes or follow-up results of cases clearly reported? | Yes | Yes | Yes | Yes | Yes |
| Was there clear reporting of the presenting site(s)’/clinic(s)’ demographic information? | Yes | Yes | Unclear | Yes | Unclear |
| Was statistical analysis appropriate? | N/A | Yes | N/A | Yes | Yes |
Table 2.
| List of Questions | Mehra et al., 2001 | Lee et al., 2013 |
|---|---|---|
| Were the criteria for inclusion in the sample clearly defined? | Yes | Yes |
| Were the study subjects and the setting described in detail? | Yes | No |
| Was the exposure measured in a valid and reliable way? | Yes | Yes |
| Were objective and standard criteria used for the measurement of the condition? | Yes | Yes |
| Were confounding factors identified? | Unclear | Unclear |
| Were strategies to deal with confounding factors stated? | Unclear | Unclear |
| Were the outcomes measured in a valid and reliable way? | Yes | Yes |
| Was appropriate statistical analysis used? | Yes | Yes |
| Author | Sample Size | Gender | Average Age (Years) | Dentoskeletal Abnormalities | ||
|---|---|---|---|---|---|---|
| Men | Women | |||||
| 1 | Acebal-Bianco et al., 2000 [23]; | 802 | 368 | 740 | 23 | - |
| 2 | Mehra et al., 2001 [22]; | 262 | N/A | N/A | 27.15 | - |
| 3 | Borstlap et al., 2004 [20]; | 222 | 53 | 169 | 23.4 | Indication: mandibular advancement |
| 4 | Teltzrow et al., 2005 [18]; | 1264 | 450 | 814 | 23.1 | - |
| 5 | Falter et al., 2010 [24]; | 1008 | 341 | 667 | 26 | - |
| 6 | Lee et al., 2013 [21]; | 10 | 5 | 5 | 22.3 ± 4.8 | Mandibular prognatism |
| 7 | Mensink et al., 2013 [25]; | 427 | 150 | 277 | 27 | 363 Class II malocclusion |
| 59 Class III malocclusion | ||||||
| 5 other (condylar hyperplasia) | ||||||
3.2. Main Findings
Demographical characteristics extracted from the reviewed studies were sample size, age, and gender of participants. The demographical and clinical characteristics of the participants can be observed in Table 3.
In terms of the technique used during the BSSO procedure, two studies (18, 20) reported using the Obwegeser Technique, with one study (20) using the Dal Pont modification with or without Hunsuck modification. Two studies used the Wolford method [21, 22], while the last three studies reported the usage of the Dal Pont-Hunsuck-Simpson-Epker modification, Epker method, and Hunsuck modification consecutively [23-25]. A bad split complication was found in 92 patients out of 3995 patients. Type I fracture pattern was found in 58 cases [18, 20-25], type II fracture pattern was found in 27 cases [18, 20, 22-25], type III fracture pattern was found in four cases [18, 23], and type IV fracture pattern was found in three cases [18, 25]. The results of data extraction in this systematic review can be viewed in Table 4.
| Author | BSSO Method | Occurrence of Bad Split | Fracture Pattern | Management | Outcome | ||||
|---|---|---|---|---|---|---|---|---|---|
| Type 1 | Type 2 | Type 3 | Type 4 | ||||||
| 1 | Acebal-Bianco et al., 2000 [23]; | Dal Pont-Hunsuck-Simpson-Epker modification | 8 | 6 | 1 | 1 | 0 | - Osteosynthetic plate - Bicortical screw - Releasing of maxillomandibular fixation (MMF) |
- Two infections - One patient with hematoma - 4 patients with pain around TMJ lasted for 6 months - One patient with disc displacement - One patient with lower lip hypesthesia - One patient with mandibular angle asymmetry |
| 2 | Mehra et al., 2001 [22]; | Wolford Method | 11 | 4 | 7 | 0 | 0 | - 2.00 mm bicortical screw - One extra screw - Additional 1.1 mm bone plate with 4-6 monocortical bone screws |
- No postoperative infection - Procedure can be completed |
| 3 | Borstlap et al., 2004 [20]; | Obwegeser Method with Dal Point Modification (with or without Hunsuck Modification) | 20 | 8 | 12 | 0 | 0 | - Additional plate - The use of tight elastics for 2-5 days - The use of loose elastics for maximum 6 weeks - Soft diet food for 6 weeks |
- Most patients are satisfied with the final result - No neurosensory disturbance and skeletal relapse |
| 4 | Teltzrow et al., 2005 [18]; | Obwegeser technique, with modification if needed | 12 | 6 | 1 | 3 | 2 | - Osteosynthetic plate - Maxillomandibular fixation (MMF) |
Bone healing and bone union processes were found to be stable. |
| 5 | Falter et al., 2010 [24]; | Epker Method | 14 | 13 | 1 | 0 | 0 | - Osteosynthetic plate | Good occlusion function after six months |
| 6 | Lee et al., 2013 [21]; | Wolford method | 10 | 10 | 0 | 0 | 0 | - Miniplate and monocortical screw - Additional bicortical positioning screw |
- Delay of bone healing - Enhancement of mandibular plane angle and anterior face height |
| 7 | Mensink et al., 2013 [25]; | Hunsuck Modification | 17 | 11 | 5 | 0 | 1 | - Osteosynthetic plate - Permanent intermaxillary fixation (IMF) |
- Good recovery of function and esthetic - Two patients with neurosensory disturbance after a bad split |
As for the management of the bad split complications, an additional plate to stabilize fracture fragments was used in all studies [18, 20-25]. Furthermore, two studies [21, 22] described the type of the osteosynthetic plate, the miniplate, as well as the bone plate used in the management of the complication. The usage of an osteosynthetic bicortical screw was reported in three studies [21-23], where the two studies [21, 23] simply reported the usage of the screw as an addition to the main fixation of the osteosynthetic plate, and the third study [22] elaborated on the type and the amount of bicortical screw used.
Additionally, the usage of a monocortical screw to secure free bony segments was reported in two studies [21, 22]; the usage of maxillomandibular fixation was reported in one study [18], and one study reported a possible release of the fixation once the BSSO procedure was completed [23]. One study reported the usage of permanent intermaxillary fixation for occlusion guidance [25], and one study reported postoperative management that consisted of a placement of a tight elastic for the duration of two to five days followed by the usage of a loose elastic for the maximum duration of six weeks [20].
Data extraction on management outcomes reported stable fracture fragments formation and union in one study [18], good occlusion function in one study [24], accomplished aesthetic expectation in one study [25], and no further complications in one study [22]. These expected outcomes resulted in a completed BSSO procedure. Yet, three studies did report several complications, whereas one study reported infection, hematoma, pain around the temporomandibular joint, disc displacement, hypesthesia of the lower lip, and asymmetrical angle of the mandible [23]; one study reported delayed bone healing process, increasing mandibular plane, and facial vertical height [21] and one study reported neurosensory disorder experienced by patients with bad split complications [25].
4. DISCUSSION
Post-operative complication(s) should always be kept to a minimum to achieve optimum results. This systematic review managed to reveal several risk factors that may contribute to the occurrence of bad split complications, namely gender, age, diagnosis of the abnormalities, and the method used to perform BSSO [26-28]. Yet, no significant association between these risk factors and the occurrence of bad split complications was found. Additionally, no articles elaborated on whether the management procedure was based on the existence of any of the risk factors.
Bad split complications were classified into four types of fractures and were mentioned in every article included in this systematic review. Based on this classification by Steenen and Becking, the four types of fractures are [3] type I, a fracture that occurs in the proximal (buccal) segment; type II, a fracture that occurs in the distal (lingual) segment; type III, a fracture that occurs in the coronoid process; type IV, a fracture that occurs in the neck of the condyle [3]. Amongst the other fractures, the type II fracture is the type of fracture that is very unlikely to occur because the bone separation takes place on a thin cortical bone [29]. In comparison, the type IV fracture is the most challenging fracture to treat due to the possible attachment and detachment of the condyle to the distal segment [16]. Considering the difficulty level, the best treatment for type IV fracture is to discontinue the BSSO procedure [3]. However, based on the results of this systematic review, all fracture cases were successfully treated by intraoperative management and supported by postoperative management, resulting in the completion of the BSSO procedure.
The results of the current study revealed the frequent usage of the osteosynthetic plate in bad split complications treatment, a rigid appliance that has become the standardized plate of choice when treating mandible fracture [30]. This might be due to the fact that it provides great fixation, anatomical reduction, and rapid restoration of (oral) functions. Due to its intraoral placement, the osteosynthetic plate is unlikely to cause any scars on the patient’s facial area. Additionally, the usage of an osteosynthetic plate reduces the possibility of injuring the marginal mandibular branch of the facial nerve [31]. The disadvantage of the osteosynthetic plate would be its thickness, making it less adaptive to the mandible surface, regardless of the strong stabilization that it may provide [32]. Alternatively, the use of a mini plate is also an option. A mini plate is quite easy to handle, less invasive, and, therefore, has a less intra-operative duration [33].
Another alternative treatment was reported by one study that implemented the bicortical and monocortical screws [21]. Both appliances are common to use to stabilize the proximal segment up to the distal segment during the BSSO procedure. There are no significant differences in terms of strength between the two instruments. Another study also recommended the usage of the bicortical screw as an attempt to avoid displacement of the proximal segment and the condyle due to the activity of the elevator muscle [34]. Additionally, the usage of a maxillomandibular fixation (MMF), which is the primary method to manage facial trauma, facial reconstruction, and orthognathic surgery, was also reported [35]. This method is performed by placing instruments in both jaws, aimed at initiating the fixation process of the maxilla and the mandible after the occurrence of a fracture and jaw immobilization [36]. The common appliances used for an MMF are arch bars, Ernst ligatures, and intermaxillary fixation (IMF).
One prospective study included in this review reported post-operative management by using an elastic band. An elastic band is indicated when a jaw fracture is accompanied by a moving segment, a vertical step is found during occlusion, a condyle fracture occurs, an occlusal adjustment after an open reduction is required, and internal fixation of the jaw is required [37]. An elastic band treatment is intended to provide the ability to adjust to the treatment design as well as to produce tensile forces between fracture segments. Consequently, it is expected that the jaw can perform its functional movements in a more natural course, something that is unlikely to occur when rigid fixation is in use. Eventually, the usage of an elastic band will result in a better bone healing process [38].
Lastly, the current study indicated that the type of treatment, as well as the modification of treatment, performed is based on the type of fracture. For example, in the case of low severity fractures of the buccal segment(s), fracture management would be less difficult compared to other segments. An important point would be that in case of a minor fracture where no functional impairment is indicated, no treatment is required, and the BSSO procedure can proceed to completion and function accordingly [21]. In the case of the occurrence of unexpected bilateral fractures, both sides should be simultaneously treated. Yet, considering the complexity of the treatment of bilateral fracture, discontinuation of the BSSO procedure should be considered if the operating surgeon does not possess adequate skill and experience. Reoperation might be considered after a six-month period, which is the maximum period for bone consolidation after the occurrence of a fracture [3].
The current systematic review has several study limitations. Considering that the authors would like to review articles that were published in the last ten years, the first limitation of the study would be the difficulty in finding article(s) within this time frame. The “latest” article that can be found was from 2013; no older articles after 2013 were able to be identified. Another limitation is the lack of outcome information provided by the articles. All articles only provided general outcome information, resulting in the lack of outcome details information provided in this systematic review.
CONCLUSION
Based on the findings of the current systematic review, it can be concluded that various materials and techniques can be applied during the management of bad split complications during the BSSO procedure. The most used materials for the treatment of bad split complications are an osteosynthetic plate and a mini plate with a bicortical screw or monocortical screw. Additionally, the MMF method is recognized as a common method used to treat bad split complications. Importantly, most studies reported that regardless of the occurrence of bad split complications, BSSO procedures were able to be completed and that most patients showed promising post-treatment results.
REGISTRATION OF THE SYSTEMATIC REVIEW
This systematic review has been registered on PROSPERO with the following registration ID: CRD42021246079.
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
PRISMA guidelines were followed.
FUNDING
None.
CONFLICT OF INTEREST
All authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGMENTS
Declared none.
SUPPLEMENTARY MATERIAL
PRISMA checklist is available as supplementary material on the publisher’s website along with the published article.


