All published articles of this journal are available on ScienceDirect.
Dental Arch Changes with Two Different Trans-Palatal Arch
Abstract
Background:
Rapid maxillary expansion (RME) is a dentofacial orthopedic treatment often used to treat patients with narrow palate and transverse maxillary growth deficiency.
Introduction:
This treatment leads to correction of posterior dental crossbites, coordination of the upper and lower arches and gaining arch perimeter in patients with tooth size/arch size discrepancies. To stabilize the results obtained with RME and to limit or avoid the relapse, the use of Transpalatal Arch (TPA) would be recommended.
Objectives:
The aim of this study is to evaluate short-term maxillary changes in patients treated with RME followed by TPA with and without palatal arms.
Materials and Methods:
30 patients, 16 females and 14 males (mean age of 9.7 yrs ranging between 9 and 12), were treated by expansion with palatal Hyrax-type expander. After this period, it was removed and one of the two different types of TPA was used.
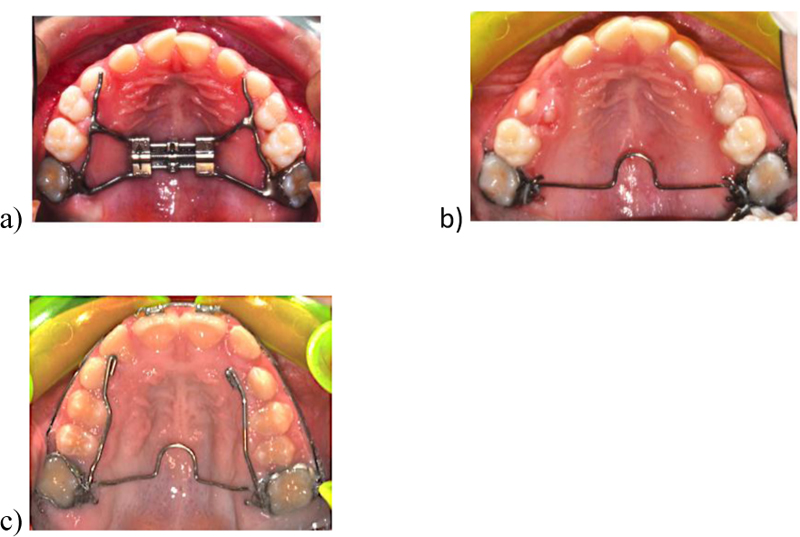
The two different TPA were a 0.036-inch stainless steel wire with a loop directed mesially in the middle, one maintained the original design (TPA), the second one presented arms extended to canines (TPAa). Dental casts were collected for each patient for each treatment step; before (T0), after expansion (T1) and after TPA or TPAa (T2). To assess differences in dental arches after the two treatment phases, three-dimensional (3D) dental casts were used to make more predictable measurements compared with caliper measurements that presented intra-examiner and inter-examiner measurements errors.
Results:
In TPAa group, differences between the value at the end of the retention period and at the end of expansion showed no statistical significance. Instead in TPA group, the same measurements suggested a reduction of value in almost all dental transverse diameters. Statistically significant differences in dental measurements were found between TPAa and TPA.
Conclusion:
Results confirm the hypothesis that TPAa can allow to better maintain dental transverse dimensions.
1. INTRODUCTION
Rapid maxillary expansion (RME) is a dentofacial orthopedic treatment often used to treat patients with the constricted palate and poor transverse maxillary growth [1].
RME is used to open the mid-palatal suture and widen the roof of the mouth and the floor of the nose in patients before it is fully fused [2]. This treatment leads to correction of posterior dental crossbites, coordination of the maxillary and mandibular dental arches and gains in arch perimeter in patients with tooth size/arch size discrepancies [2]. However, the long-term stability of these skeletal and dental changes still remains controversial [3, 4]. Previous studies of Krebs [5] and Skieller [6] and the more recent of Akkaya et al. [7] reported that the rapid maxillary expansion appliances show stable results [8]. Conversely, according to Germane et al. [9], the outcomes of a RME treatment are not completely stable due to the increase in cheek or lip pressure in case of a small dental arch. This could potentially bring teeth back to the original positions [10]. Therefore, to stabilize the results obtained with RME and to limit or avoid the relapse, the use of Transpalatal Arch (TPA) is recommended [11]. According to McNamara, TPA is generally used to control the transverse dimension of the maxilla [11, 12]. The conventional TPA, as designed by Goshgarian, is a fixed appliance composed of a round stainless steel wire that goes across the palatal contour with a center U-loop. It is inserted into the lingual sheath of the first permanent molars bands [11-14]. According to recent studies, the use of TPA in mixed dentition followed by fixed appliances was effective in significantly increasing dental arch width and perimeter [10]. The changes remained stable after an average 6.7- years follow-up [10]. Moreover, a modified TPA with palatal arms extended up to canines may be considered as a valid retention tool after RME treatment. Thus, TPA stabilizes the palatal arch posteriorly and transversely and, when needed, helps preserve leeway spaces during the transition of the dentition [15]. Both auxiliary appliances, conventional and modified TPA, when placed passively, are used to maintain the position of maxillary molars in 3 dimensions, keeping the intercuspid widths that mostly tend to relapse [15]. To evaluate differences in dental arches after two different treatments, the adequate choice is to use digital three-dimensional (3D) dental casts [16]. Indeed, plaster models have the disadvantages, such as breakage, loss, and storage requirements [17, 18]. Therefore, the use of digital models makes the measurements more predictable compared with caliper measurements taken from plaster models. Indeed the latter ones have intra-examiner and inter-examiner measurements errors [19-24]. In literature, there is a deficiency of efficiency of two different TPA with the use of digital models. So, the purpose of this study was to evaluate short-term maxillary changes in patients treated with rapid maxillary expansion (RME) followed by TPA with and without palatal arms.
2. MATERIALS AND METHODS
This observational retrospective cohort study was performed in accordance with the Declaration of Helsinki and appropriate ethical approval was granted by the Health Research Ethics Board of University of Campania “Luigi Vanvitelli” (Naples, Italy; approval number 717/18). A signed informed consent from the subjects’ parents was obtained. The sample size was estimated based on preliminary data. A minimum sample of 28 subjects was needed in order to achieve 80% power, with an alpha of 5% to detect a 0.5mm difference (SD 0.5 mm). 30 patients, in particular, 16 females and 14 males, (mean age of 9.7 years ranging between 9 and 12) were collected from the archives of Orthodontic Program of the same university (Table 1).
Inclusion criteria of this retrospective study were:
- Mild to moderate maxillary crowding
- Mixed dentition with fully erupted upper permanent molars
Prepubertal skeletal maturation (CS1 or CS2)
- Treatment with RME followed by conventional TPA (TPAc) or TPA with arms extended to canine (TPAa)
- Presence of dental cast in the three treatment steps.
While Exclusion criteria were:
- Previous orthodontic treatment
- Previous tooth extraction
- Craniofacial anomalies
Recruited subject was divided into two groups based on TPA design.
| Total | Male | Female | Age | |
| Group | N | n | n | Mean |
| TPA | 15 | 4 | 11 | 9.73 |
| TPAa | 15 | 10 | 5 | 9.63 |
| Total | 30 | 15 | 15 | 9.7 |
The samples were treated by expansion with a palatal Hyrax-type expander with rapid maxillary expansion protocol and the operator started activation with two turns of the expansion screw (0.25 mm per turn). Then parents continued the activation two turns per day. Patients were monitored once every 2 weeks until maxillary palatal cusps touched buccal lower cups. Then the appliance was maintained in situ for at least 6 months to preserve the outcomes achieved.
After this period, the Hyrax device was removed and one of the two different types of TPA was used.
The two different TPA were made of 0.036-inch stainless steel wire with a loop directed mesially in the middle: the TPA maintained the original design, while the TPAa presented arms extended to canines (Fig. 1).
For each patient, gypsum cast models for each treatment step were collected: before (T0) and after expansion, including 6 months of retention with the same appliance (T1), and after using the two types of TPA (T2).
The dental cast models were scanned by 3Shape D700 and exported in STL surface mesh, then imported in Viewbox 4.0.1.7 software (dHAL Software, Kifissia, Greece, Athens).
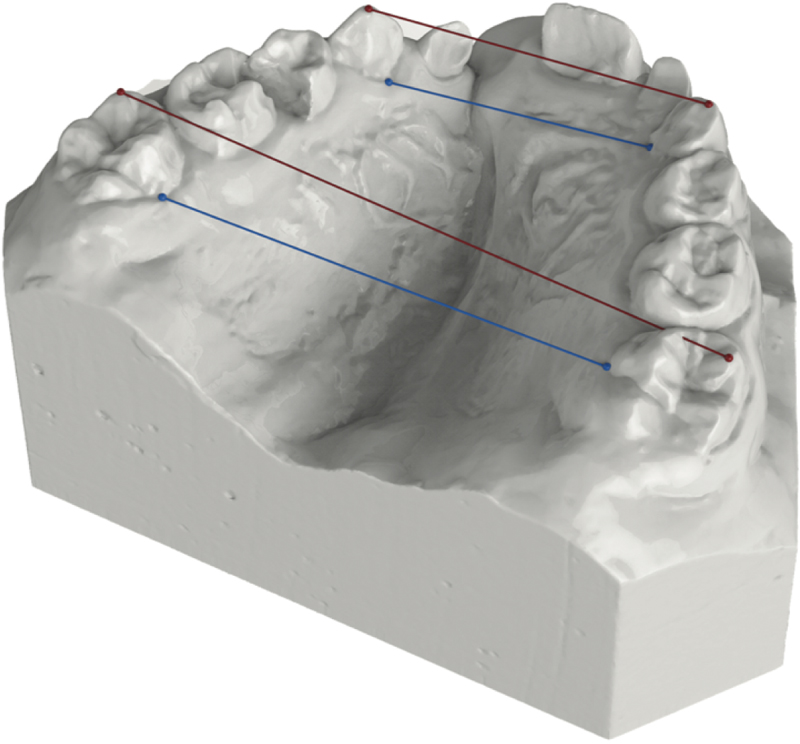
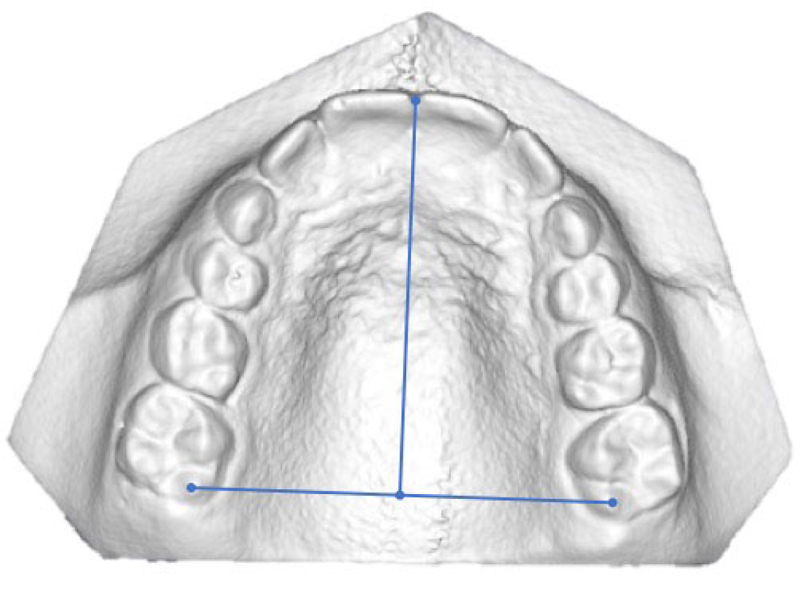
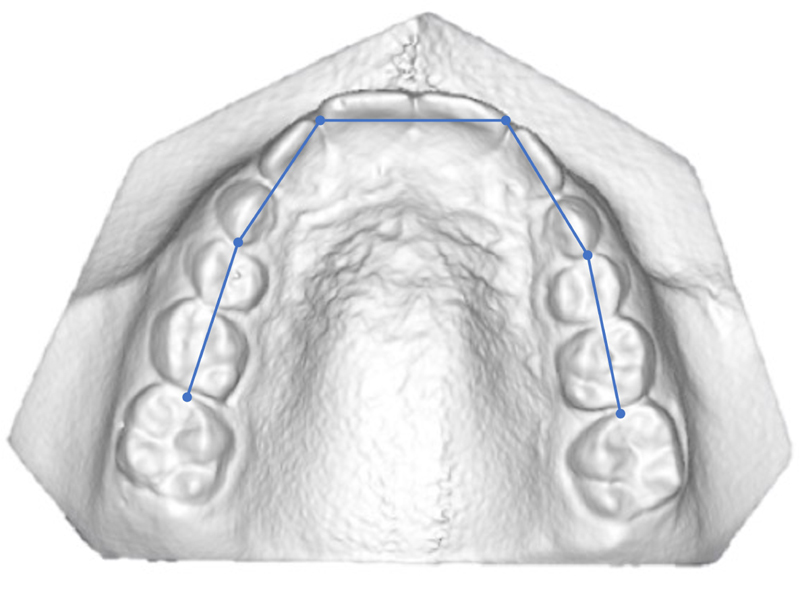
Dental reference points (Table 2) were identified to carry out linear measurements as shown in Table 3 and Figs. (2-4).
| 1-2 Mid-incisal | Point lies at the middle of right and left maxillary centrals and laterals incisal edge |
| Mid-centrals | Point midway between right and left maxillary centrals line angles |
| 3-4 OC | Buccal Cusp tip of right and left maxillary canines and first premolar |
| 6OC | Distobuccal cusp tip of right and left maxillary first molars |
| 1 -6 Ging | Most gingival points of palatal surface of clinical crown of dental elements. |
| 6 Mid | Point midway between right and left 6OC |
| 3 - 6 Occlusal | Linear distance between right and left 4-6 OC |
| 3 - 6 Gingival | Linear distance between right and left 4-6 Ging |
| Arch Lenght | Perpendicular distance between Mid-centrals and line connecting right and left 6OC |
| Arch Perimeter | Length of curve connecting incisors Mid-incisal and premolars and first molar Oc points |
2.1. Statistical Analysis
For continuous variables, means and standard deviations were calculated. For categorical variables, absolute numbers were reported. Categorical variables were compared with χ2.
Comparison of continuous variables between time points was made through unpaired t tests, while average changes within individual cases were tested through paired t tests.
The level of statistical significance was set at P < 0.05 for all statistical tests.
Five measurements were performed after 1 month by the same operator to perform error analysis. Measurements were also repeated on eight randomly selected digital models (4 upper and 4 lower arches). Dahlberg’s D was calculated to quantify the measurement error, and Student’s t test for paired data to identify any systematic error.
3. RESULTS
Each group consisted of 15 patients. In TPA group, there were 11 females and 4 males with a mean age of 9.73 years (age range from 9 years to 11 years), while in TPAa group, there were 5 females and 10 males with a mean age of 9.63 years (age range from 9 years to 12 years).
3.1. Reliability
Systematic and random errors for all the variables have been calculated. No significant systematic error was found (Table 4).
| T0 | T1 | T2 | ||||
| Measurements | D Dahlberg (mm) |
Systematic error P level |
D Dahlberg |
Systematic error P level |
D Dahlberg |
Systematic error P level |
| 3-3 ap | 1,23 | 0,76 | 1.55 | 0,45 | 1,33 | 0,22 |
| 3-3 oc | 1.12 | 0,56 | 0.78 | 0,33 | 1,12 | 0,24 |
| 4-4 ap | 0,87 | 0,67 | 1.56 | 0,12 | 0,76 | 0,67 |
| 4-4 oc | 1.50 | 0,45 | 1.34 | 0,67 | 1.55 | 0,12 |
| 5-5 ap | 1.45 | 0,55 | 0,56 | 0,23 | 2,05 | 0,45 |
| 5-5 oc | 1.67 | 0,45 | 1.53 | 0,23 | 0,67 | 0,33 |
| 6-6 ap | 1.07 | 0,33 | 1.67 | 0,56 | 1,03 | 0,43 |
| 6-6 oc | 0,67 | 0,12 | 0.87 | 0,45 | 1,89 | 0,18 |
| arch perimeter | 4.06 | 0,22 | 1.81 | 0,56 | 0,65 | 0,44 |
| arch lenght | 2,56 | 0,33 | 1,56 | 0,33 | 0,89 | 0,33 |
3.2. Comparison between Groups at the Start of Treatment (T0)
No statistical differences were found at the beginning of treatment between the two groups (Table 5).
3.3. Comparison between Groups at the end of Expansion Protocol (T1)
After RME activation, all linear transverse measurements were significantly increased in both groups, and there was no difference between the two groups (Table 5).
3.4. Comparison between Groups at the end of Transpalatal arch Treatment (T2)
After RME (T1), each group had a relapse during TPA phase (T2). The comparison between the two group changes between T1-T2 showed significant differences, with higher stability of TPA with arms in transversal diameters. TPA group showed significant relapse ranging between 1.72 and 4.13 mm. No differences were found between groups at T2 in arch length and palatal depth (Table 5).
3.5. Differences between Begging of Treatment and end of Expansion Treatment (T1-T0)
Both groups showed significant differences in measurements at the end of the expansion procedure except for antero-posterior length value and arch-length Occ (Tables 6 and 7).
3.6. Differences between Outcomes of Transpalatal arch Retention Period and Beginning of Treatment (T2-T0)
Both groups showed significant increases in all transversal dental diameters at the end of the palatal arch retention period compared to the beginning of the treatment (Tables 6 and 7).
3.7. Differences between Outcomes of Expansion Treatment and end of Transpalatal arch Retention Period (T2-T1)
In TPAa group, differences between the value at the end of the retention period and at the end of expansion showed no statistical significance. Instead, in TPA group, the same measurements suggested a reduction of value in almost all dental transverse diameters (Tables 6 and 7).
| T0 | T1 | T2 | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TPA | TPAa | TPA | TPAa | TPA | TPAa | ||||||||||||||
| Media | DS | Media | DS | Mean Diff | P | Media | DS | Media | DS | Mean Diff | P | Media | DS | Media | DS | Mean Diff | P | ||
| 3 - 3 OCC | 32,45 | 2,62 | 32,55 | 2,70 | -0,1 | 0,92 | 37,57 | 1,39 | 37,57 | 3,1 | 0 | 0,99 | 35,85 | 1,48 | 37,68 | 2,49 | -1,83 | 0,02 | |
| 3 - 3 AP | 25,74 | 2,20 | 25,58 | 1,96 | 0,16 | 0,84 | 29,45 | 2,00 | 29,87 | 2,70 | -0,42 | 0,64 | 28,36 | 1,68 | 29,88 | 2,63 | -1,52 | 0,07 | |
| 4 - 3 OCC | 40,19 | 2,98 | 38,91 | 3,08 | 1,28 | 0,26 | 47,83 | 2,72 | 47,49 | 3,02 | 0,34 | 0,75 | 44,74 | 1,54 | 47,45 | 2,82 | -2,71 | 0,00 | |
| 4 -4 AP | 27,63 | 2,31 | 27,34 | 2,03 | 0,29 | 0,72 | 34,49 | 2,00 | 33,83 | 2,84 | 0,66 | 0,47 | 30,36 | 1,38 | 32,25 | 2,61 | -1,89 | 0,02 | |
| 6 - 6 OCC | 52,47 | 3,24 | 52,44 | 2,34 | 0,03 | 0,98 | 60,23 | 3,33 | 61,05 | 2,99 | -0,82 | 0,48 | 57,89 | 2,60 | 60,75 | 3,36 | -2,86 | 0,01 | |
| 6 – 6 AP | 32,65 | 3,24 | 32,44 | 2,29 | 0,21 | 0,84 | 40,61 | 3,04 | 40,87 | 1,92 | -0,26 | 0,78 | 38,51 | 2,64 | 40,72 | 2,93 | -2,21 | 0,04 | |
| ARCH LENGTH | 35,58 | 2,44 | 36,96 | 2,88 | -1,38 | 0,17 | 35,06 | 2,81 | 37,25 | 3,19 | -2,19 | 0,06 | 34,94 | 2,98 | 36,61 | 3,49 | -1,67 | 0,30 | |
| ARCH PERIMETER | 77,47 | 3,39 | 79,12 | 4,16 | -1,65 | 0,24 | 78,95 | 4,26 | 81,57 | 3,65 | -2,62 | 0,08 | 76,05 | 4,86 | 79,07 | 4,91 | -3,02 | 0,10 | |
| TPA | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| T1-T0 | T2-T0 | T2-T1 | |||||||
| Mean Diff | DS | P | Mean Diff | DS | P | Mean Diff | DS | P | |
| 3occ | 5,11 | 3,00 | 0,00 | 3,39 | 2,83 | 0,00 | 1,72 | 1,24 | 0,00 |
| 3 ap | 3,71 | 2,18 | 0,00 | 2,62 | 2,55 | 0,00 | -3,09 | 2,35 | 0,12 |
| 4 occ | 7,64 | 4,58 | 0,00 | 4,55 | 2,89 | 0,00 | -3,09 | 2,35 | 0,00 |
| 4 ap | 6,86 | 3,49 | 0,00 | 2,73 | 2,08 | 0,00 | -4,13 | 2,64 | 0,00 |
| 6 occ | 7,76 | 4,09 | 0,00 | 5,42 | 4,08 | 0,00 | -2,34 | 3,44 | 0,04 |
| 6 ap | 7,96 | 4,96 | 0,00 | 5,86 | 4,12 | 0,00 | -2,10 | 4,31 | 0,05 |
| Arch Lenght | -0,52 | 2,80 | 0,59 | -0,64 | 2,34 | 0,53 | -0,12 | 3,29 | 0,91 |
| Arch Perimeter | 6,08 | 3,77 | 0,04 | 2,23 | 5,24 | 0,28 | -1,96 | 6,32 | 0,32 |
| TPAa | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1-T0 | T2-T0 | T2-T1 | |||||||||||||||
| Mean Diff | DS | P | Mean Diff | DS | P | Mean Diff | DS | P | |||||||||
| 3occ | 5,02 | 2,51 | 0,00 | 5,13 | 2,26 | 0,00 | 0,11 | 2,40 | 0,92 | ||||||||
| 3 ap | 4,29 | 2,84 | 0,00 | 4,30 | 3,26 | 0,00 | 0,01 | 2,94 | 0,99 | ||||||||
| 4 occ | 8,58 | 2,77 | 0,00 | 8,55 | 2,65 | 0,00 | -2,75 | 3,77 | 0,98 | ||||||||
| 4 ap | 6,49 | 3,17 | 0,00 | 4,91 | 2,71 | 0,00 | -1,59 | 3,04 | 0,12 | ||||||||
| 6 occ | 8,61 | 3,36 | 0,00 | 8,31 | 3,65 | 0,00 | -0,30 | 2,04 | 0,80 | ||||||||
| 6 ap | 8,43 | 2,40 | 0,00 | 8,28 | 3,33 | 0,00 | -0,15 | 2,05 | 0,87 | ||||||||
| arch length | 0,29 | 1,95 | 0,80 | -0,53 | 2,36 | 0,34 | -0,82 | 1,46 | 0,35 | ||||||||
| Arch perimeter | 5,95 | 3,79 | 0,00 | 3,55 | 3,41 | 0,09 | -2,41 | 3,20 | 0,22 | ||||||||
4. DISCUSSION
The objective of the present retrospective study was to evaluate differences in patients treated with rapid maxillary expansion (RME) followed by TPA with and without palatal arms. Several authors, such as De Luca Canto G and Fleming PS, reported that a retention period of at least 5/6 months is necessary to permit adequate mineralization of the midpalatal suture in order to minimize the relapse tendency after rapid maxillary expansion20-21 . For this reason, the records at T1 were undertaken after 6 months with RME.
After the 6 months with RME, TPA (conventional and modified) was applied to each patient to maintain but also to improve the transverse diameters during the transition period, before starting the fixed appliance.
In this study, it was important to evaluate the difference between ap (cervical evaluations) and the occ (occlusal evaluations) to understand the changes of the position of the tooth, influenced by its inclination, therefore to differentiate the real movement of the tooth from the tipping. The maintained arch length was useful to correct crowding. The difference in T2 of the arch length between TPA and TPAa was not significant, therefore even if we have had significant reductions in transverse diameters, clinically there would be no difference in the diameters.
In this study at T0-T1 there were no statistical differences at the beginning of treatment between the two groups. All patients, after RME activation, showed significantly increase of all the linear transverse measurements in both groups, so there was no difference.
After the treatment with RME (T1), each group had a relapse during the TPA phase (T2). This decrease in transverse diameters in this phase, in both groups, is attributable to relapse due to expansion with RME. It is therefore clear that everyone has had a significant decrease in all transverse diameters in the retention phase and that is why there lies a big difference between T1 and T2. Certainly, however, between the great relapse of the two groups, the TPAa group maintained more transversal diameters than the TPA group. This is because of the use of the arms, adhering to the palatal part of the teeth up to the canines, in the relapse phase, they have maintained, even if only in the form of torque, the transverse diameters. While, as regards length, there was no significant difference at T2 between the two groups. From the results, it is clear how effectively in both groups there has been an effective expansion of the upper maxillary arch. Results showed that the amount of treatment changes between T1-T0 means that the groups are homogeneous and comparable. The T2-T0 results showed an increase in all transverse diameters indicating that the treatment required for the patients was completed, with an expansion of the maxillary arch. Results showed that using modified TPA the transversal dimension was maintained better and showed less relapse. This means that after RME, the TPA with the arms maintains the inter-molar, inter premolar and inter-canine diameter above all the better than the conventional TPA.
4.1. 3D Models
For prevalence of few errors for the measurements 3D dental casts were used.
The advantage of using the digitalization of 3D models through the use of a scanner guarantees the elimination of errors relating to plaster models, increasing the convenience of storing and managing them and greater accuracy of measurements [15, 16].
However, the possibilty of no errors cannot be excluded in the calculation of the measurements made on the computer, but this is dictated by the operator himself [17]. The percentage of error was low, showing high reliability of location, tracing, and measurements, confirming that the use of 3D methods is a useful method to assess transverse changes.
CONCLUSION
- At the end phase of expansion, teeth showed a significant decrease after TPA treatment.
- The use of modified TPA with arms to canines showed higher stability than conventional TPA.
- Thus, results confirm the hypothesis that TPA with arms may allow maintaining dental transverse dimensions better. Statistically significant differences in dental measurements were found between TPA with arms and conventional TPA.
- The change in A-P length and arch length was not significant.
- TPA with arms up to the canines allows us to maintain and also to improve the results obtained during the expansion treatment.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Appropriate ethical approval was granted by the Health Research Ethics Board of University of Campania “Luigi Vanvitelli” (Naples, Italy; approval number 717/18).
HUMAN AND ANIMAL RIGHTS
No animals were used in this study. The study on humans was conducted in accordance with the ethical rules of the Helsinki Declaration.
CONSENT FOR PUBLICATION
A signed informed consent from the subjects’ parents was obtained.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data of this research are available, please contact the corresponding author [G.V] to request them.
FUNDING
No funding was obtained for this research.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


