Correlation of Pericoronal Radiolucency Around Impacted Mandibular Third Molars Using CBCT with Histopathological Diagnosis: A Prospective Study
Abstract
Purpose:
This study aimed to correlate the pericoronal width surrounding impacted mandibular third molars with their histopathological findings.
Materials and Methods:
The present study included patients who were advised for extraction of impacted mandibular third molars with the pericoronal radiolucency radiographically. The CBCT scans were compared with histopathologic findings of the follicles.
Results:
Out of 70 patients evaluated histopathologically, 24 patients showed mild inflammatory changes, whereas 34 patients revealed cystic changes suggestive of a dentigerous cyst, followed by 12 patients showing evidence of calcifications in the pericoronal follicles. The dentigerous cyst was more likely to occur if the bucco-lingual width of the pericoronal radiolucency was 14.00-16.00mm, and calcifications were found to be most likely present if the buccolingual width was 12.00-14.00mm, both of which were statistically significant.
Conclusion:
CBCT can be a reliable tool in the evaluation of pericoronal follicular space, and the values in different dimensions can be an accurate predictor radiologically for the diagnosis of pathologies when compared to 2D imaging.
1. INTRODUCTION
By definition, an impacted tooth is a tooth that is completely or partially unerupted and is positioned against another tooth, bone, or soft tissue, such that its further eruption is unlikely as described according to its anatomic position [1]. Once the tooth has fully developed inside the jaw, the coronal part of the follicle is termed as pericoronal sac or follicle, which persists adjacent to the crown of unerupted or impacted teeth. It is composed of fibrous connective tissue and frequently contains epithelial residues of odontogenesis, which could be a potential initial trigger point of pathology [2]. In 2001, Damante characterized the follicle as the remnant of tissues that participated in odontogenesis and remained around the crown of a tooth, which has not erupted normally [3]. Radiographically, the pericoronal follicle presents as a slight pericoronal radiolucency around the unerupted tooth with a thin radiopaque border. However, enlargement and asymmetry can occur occasionally.
Dental follicular space radiographically appears as a thin pericoronal radiolucency, considered normal by some authors when confined within 2.5-3mm of thickness [4-8]. The dental follicle may show various histopathological changes during tooth development, which may lead to the development of odontogenic tumors or cysts. The fibrous connective tissue of the follicle usually contains odontogenic cell rests, which could be the source of pathologies like dentigerous cyst (DC), ameloblastoma, or ameloblastic fibroma. DC is the most common of the developmental odontogenic cysts of the jaws and accounts for 24% of them [9]. Other complications involving the third molars include conditions such as pericoronitis, dental caries, and second molar root resorption [1].
Various imaging modalities that are traditionally used for viewing impacted mandibular third molars include intra-oral periapical radiographs, panoramic radiographs, computed tomography [10], magnetic resonance imaging [10, 11], and cone-beam computed tomography (CBCT) [12]. The imaging techniques most commonly used for assessing impacted mandibular third molars are IOPAs and panoramic radiographs. However, these two-dimensional radiographs do not provide an accurate assessment of the depth of the impacted mandibular third molars. A huge disadvantage of IOPA is that the location of the tooth perceived from the crest might not be the actual position of the tooth due to the angulation of the tooth [13]. In comparison to IOPAs, panoramic imaging provides a wider area of visualization for the assessment of impacted mandibular third molar. However, the major disadvantage of this mode of imaging is the production of lower resolution images as well as the production of phantom images, which can cause misdiagnosis [14].
The two-dimensional imaging system, when compared to modern three-dimensional imaging, has a major drawback, which is the inability to depict the bucco-lingual relationship of the impacted mandibular third molar to adjacent structures [15, 16]. Hence, it does not reveal the true dimensions of the pericoronal follicle. CBCT allows the creation of “real-time” images not only in the axial plane but also 2-dimensional (2D) sections in the coronal, sagittal, and even oblique or curved image planes – a process referred to as multiplanar reformation. CBCT is valuable in the diagnosis of impacted teeth, especially the location and proximity of vital structures and involvement of cortical plates with impacted 3rd molars. CBCT can also be a useful tool in the evaluation of the follicular space surrounding an impacted tooth and can give an insight into the probable pathologies affecting it [17, 18]. Some authors have indicated that the presence of a pericoronal radiolucency greater than 2.5 mm may be suggestive of a DC [19].
The incidence of impacted teeth affects between 14% to 96% of the general population. Of these, 98% of the impacted teeth are the mandibular third molars, and only 50% of the third molars erupt into the oral cavity [16]. The mandibular third molar tooth germ is usually radiographically seen by the age of 9 years, and cusp mineralization is completed by 2 years. The crown formation is completed by the age of 14 years, and the roots are approximately 50% formed by 16 years of age, and by 18 years, the root is completely formed with an open apex. By 24 years of age, 95% of all the molars will complete their eruption [18].
If the impacted third molar is left intact in the jaw, the follicle may undergo cystic degeneration. The follicular sac may also develop into an odontogenic tumor. These pathological entities usually occur under 40 years of age [19-24]. The dentigerous (or follicular) cyst (DC) is the most common developmental odontogenic cyst of the jaw. It accounts for approximately 20-24% of the jaw cysts, which are lined by epithelium. It develops around the crown of an unerupted tooth and is often asymptomatic, but sometimes there may be an acute inflammatory exacerbation, pain, tooth displacement, swelling, sensitivity, and mobility. A radiograph of the dentigerous cyst usually shows a well-defined radiolucent lesion that is unilocular and has a sclerotic border surrounding the crown of the impacted teeth [25-28].
In the present study, we have attempted to radiographically assess pericoronal follicles surrounding impacted mandibular third molars and histologically evaluate the dental follicles for the presence of any pathology. The objective of our study was to diagnose any pathologic changes associated with impacted mandibular third molars and the influence of the position of the impacted mandibular third molars on any observed pathology. We also aimed to correlate CBCT and histopathology in the diagnosis of pathologies associated with the pericoronal radiolucencies.
2. METHODS
A prospective study was conducted in the Department of Oral Medicine and Radiology with a total of 70 patients above 20 years of age with an equal number of men and women. Approval was obtained from the Institutional Ethical Committee (Approval No-17031). Subjects with evidence of impacted mandibular third molars and having a pericoronal follicular space width not more than 3mm were included in the study. The exclusion criteria were patients below 20 years of age with a pericoronal follicular space width of more than 3mm.
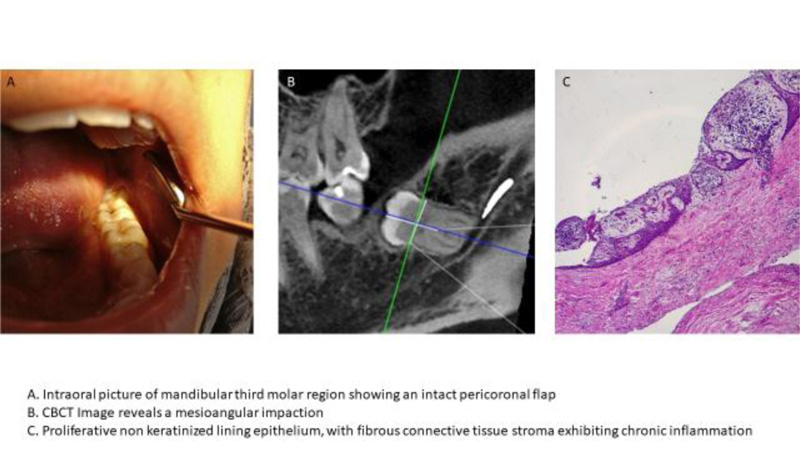
After obtaining informed consent from the patients, a CBCT scan was taken for the region of impacted mandibular third molars, which were scheduled for extraction. A CBCT scan of the area of interest was taken using the Planmeca Promax Mid 3D unit. The exposure used for the medium field of view scans were 90kV, 12 mA, and 8 seconds. Fig. (1) shows the clinical, radiographic, and histopathologic images of a subject evaluated in the study.
The following measurements were incorporated to record the pericoronal dimensions:
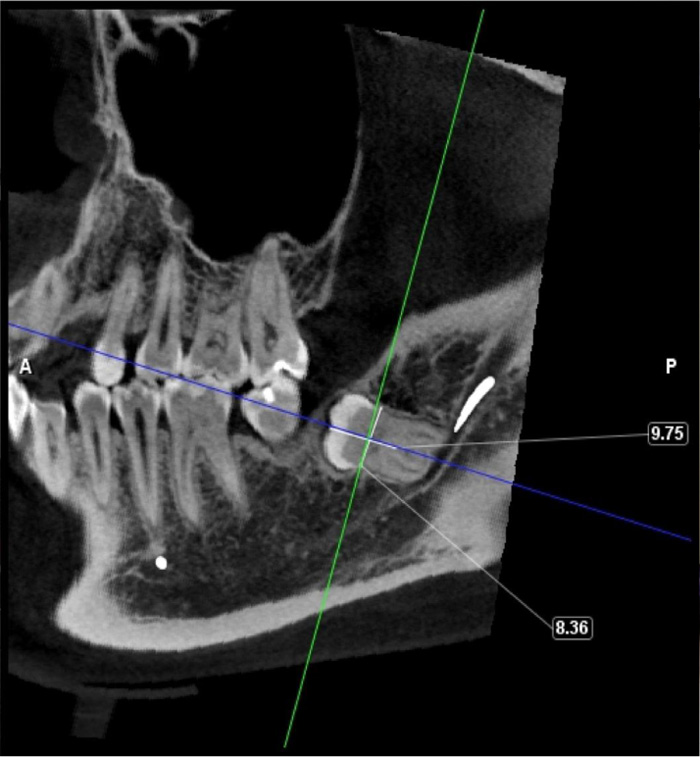
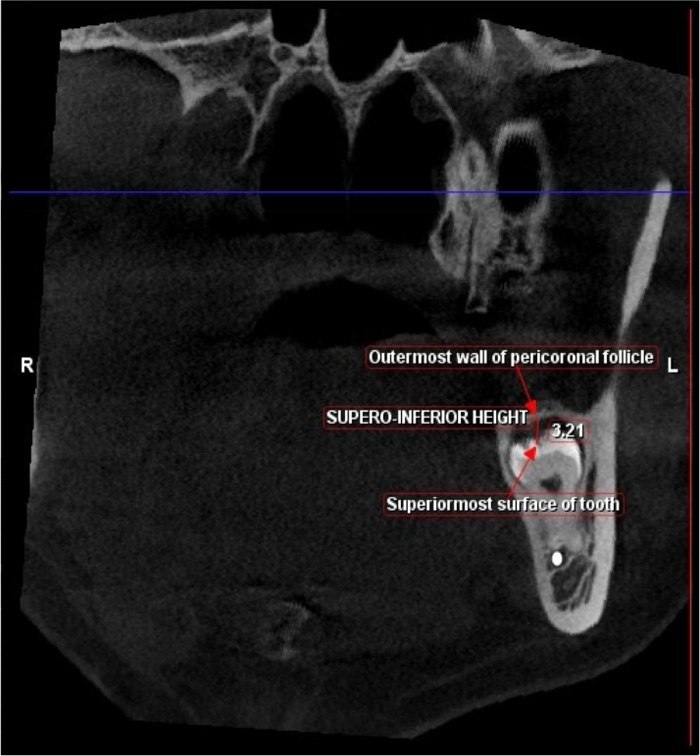
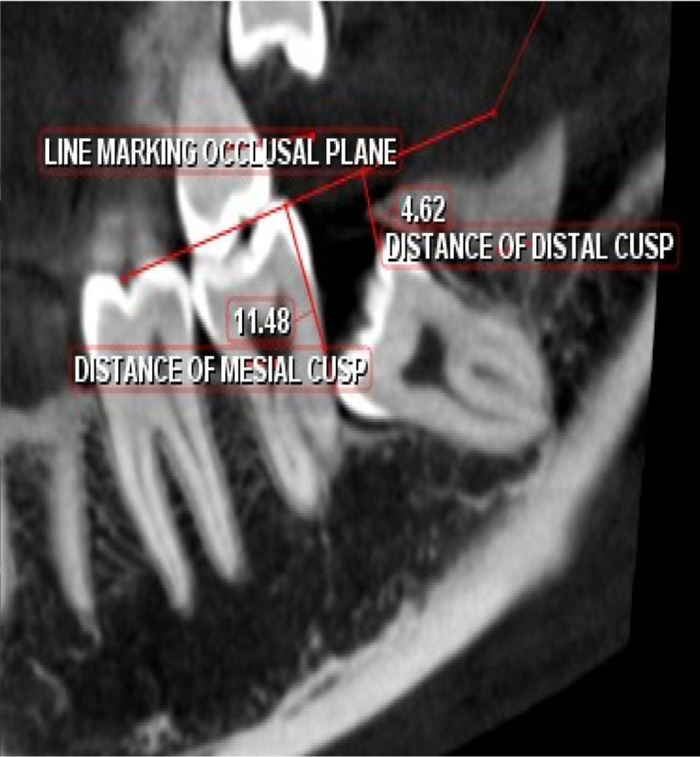
(1) A horizontal line was drawn across the maximum mesiodistal width of the crown at the level of the middle third of the tooth, and simultaneously, a vertical line was drawn perpendicular to this horizontal line corresponding to the maximum superior-inferior height (Fig. 2).
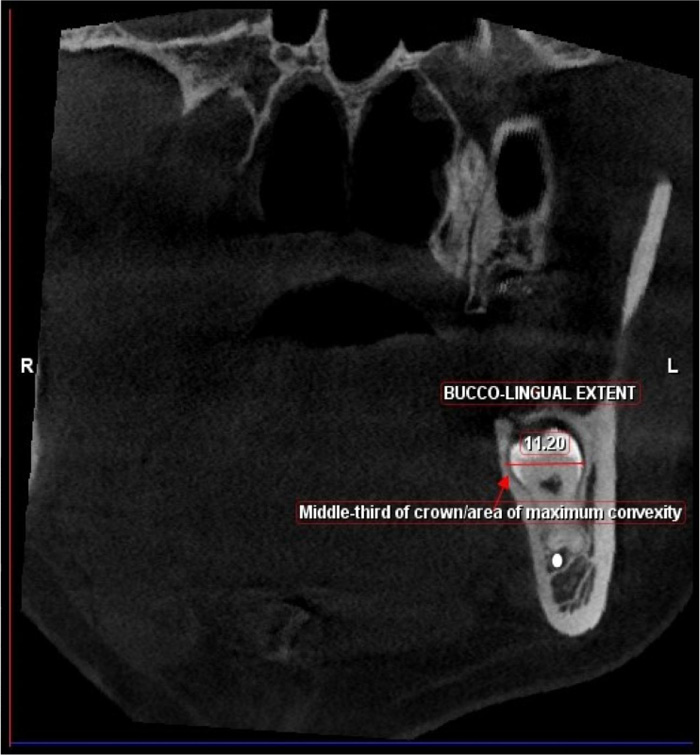
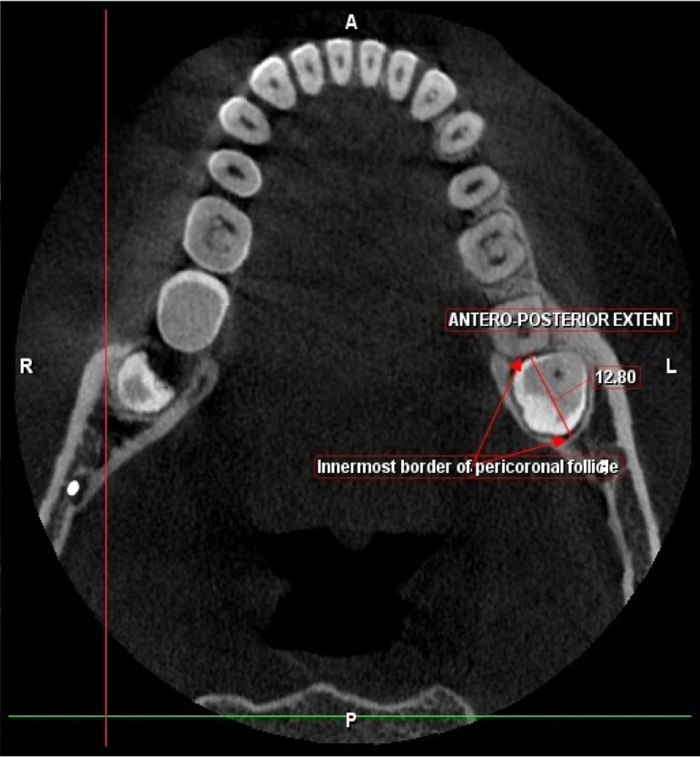
(2) The coronal plane was corrected to correspond with the horizontal line, and the axial plane was corrected to align along the vertical line. The maximum width of the pericoronal radiolucency was then measured in axial and coronal sections (Figs. 3-6) depending on the type of impaction as classified by Paul and Gregory [14] for impacted mandibular third molars.
(3) The position of the impacted mandibular 3rd molars was determined by drawing a line along the occlusal surfaces of the first and second molars and determining the distance of mesial and distal aspect of the crown of the third molar from the occlusal plane. The tooth was deemed to be impacted when the occlusal surface of the third molar was placed at a level below the cervical third of the second molar (Fig. 3).
(4) Pericoronal width space in coronal sections was measured in supero-inferior, bucco lingual direction and was categorized in mms into 8 types:
Category 1 S-I: 0.8-1.00mm
Category 2 S-I: 1.00-1.20mm
Category 3 S-I: 1.20-1.40mm
Category 4 S-I: 1.40-1.60mm
Category 5 S-I: 1.60-1.80mm
Category 6 S-I: 1.80-2.00mm
Category 7 S-I: 2.00-2.20mm
Category 8 S-I: 2.20-2.40mm
Pericoronal width space in axial sections was measured in Antero Posterior direction and was categorized in mm into 8 types:
Category 1 A-P: 8.00-10.00mm
Category 2 A-P: 10.00-12.00mm
Category 3 A-P: 12.00-14.00mm
Category 4 A-P: 14.00-16.00mm
Category 5 A-P: 16.00-18.00mm
Category 6 A-P: 18.00-20.00mm
Category 7 A-P: 20.00-22.00mm
Category 8 A-P: 22.00-24.00mm
The patients, once diagnosed, were referred to the Dept. of Oral and Maxillofacial Surgery for extraction of the impacted molar and enucleation of the follicle from the extraction socket. The dental follicle was then placed in a fixative and sent for histopathological evaluation. The findings after histopathologic evaluation of the follicle were compared with the CBCT findings and tabulated.
2.1. Statistical Analysis
Correlation of the diagnosis in CBCT and histopathology was done by calculating positive predictive value, the negative predictive value, and the sensitivity and specificity of CBCT in the diagnosis of DC and hyperplastic dental follicles.
3. RESULTS
Among the 70 patients (35 males and 35 females) evaluated, a total of 24 patients showed mild inflammatory changes indicative of normal dental follicle, 34 patients revealed cystic changes suggestive of a DC, and 12 patients demonstrated evidence of calcifications in the pericoronal follicular wall on histopathologic section. On comparing the age groups, it was observed that the pathologic changes suggestive of a DC were highest among the age group of 25 to 29 years with a statistically significant result (p=0.001). The age group of 30-34 years had a slight increase in the calcific changes in the follicles in comparison to cystic changes (Fig. 7).
Among males, 16 subjects had normal dental follicles, 11 subjects had cystic changes suggestive of a DC, and 8 subjects showed evidence of calcifications in the pericoronal follicles. Similarly, among females, 8 subjects revealed normal histopathological findings, 23 subjects had cystic changes suggestive of DC, and 4 subjects showed evidence of calcifications in the pericoronal follicles (Fig. 8). It was observed that the pathologic changes associated with the formation of DC were highest among females, with a statistically significant result (p=0.016). Also, the number of subjects with calcifications in the pericoronal follicles was higher in males with a total of 8 subjects in comparison to females, wherein only 4 of the subjects had calcifications.
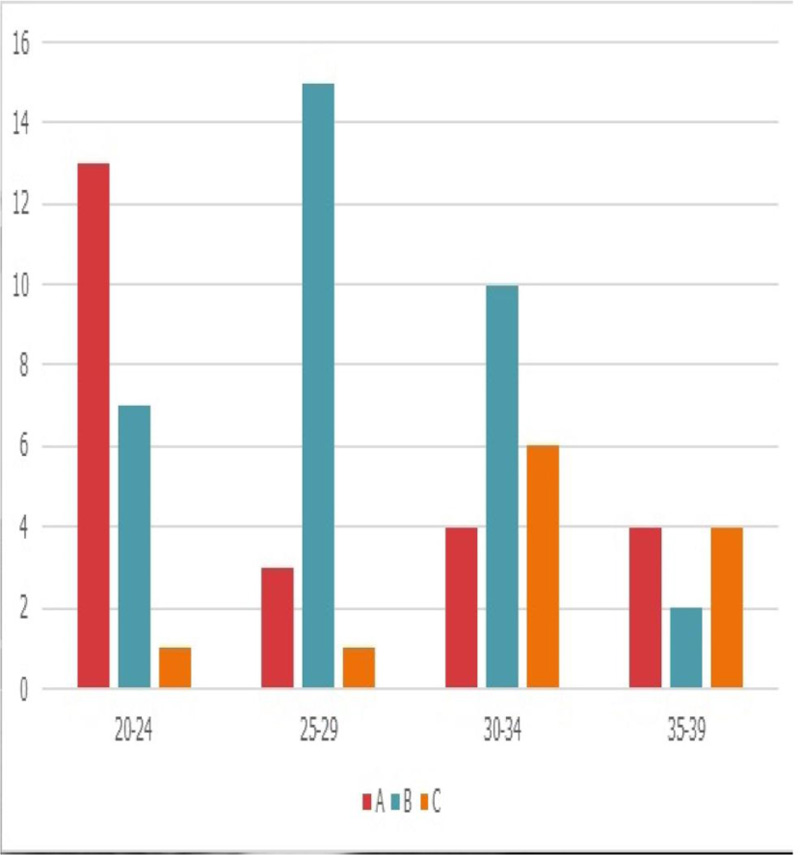
Abbreviations: A: Normal Pericoronal follicles, B: Changes Suggestive of Dentigerous Cyst, C: calcifications in relation to Pericoronal follicles.
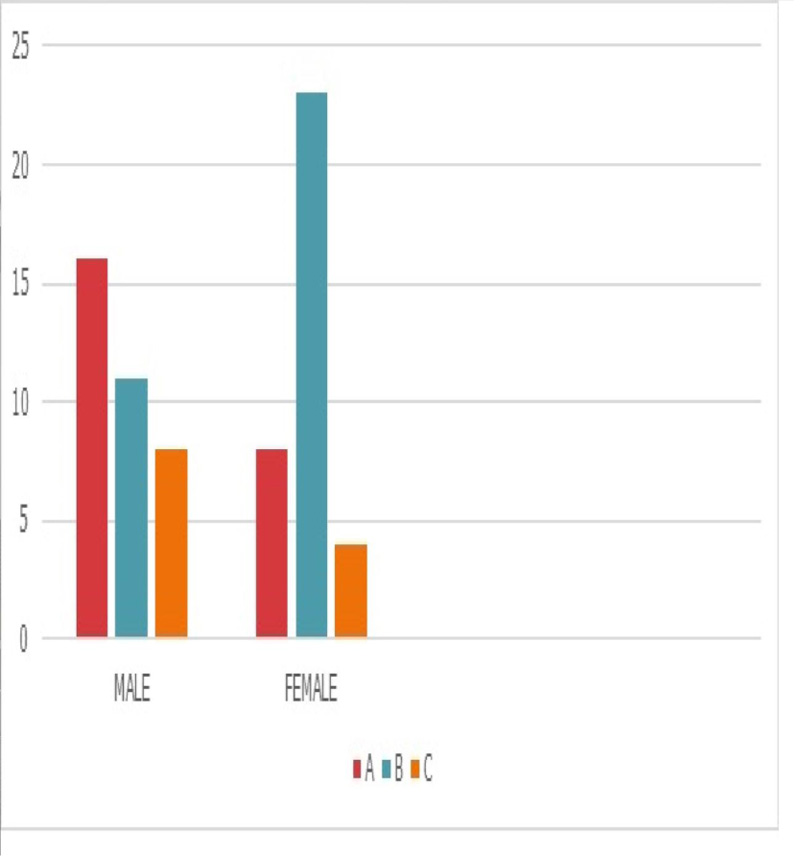
Abbreviations: A: Normal Pericoronal follicle, B: Changes suggestive of Dentigerous Cyst, C: Calcifications in relation to Pericoronal follicles.
A total of 27 teeth were observed to be horizontally impacted, followed by 22 disto-angular and 21 mesioangular impactions (Fig. 9). However, no cases of vertical impactions were recorded in our study. Incidence of DC was highest among disto-angular impactions in comparison to other types of impaction with a statistically significant result (p=0.001). Calcifications were present in 7 subjects out of 22 disto-angular impactions and in 4 subjects with horizontal impactions.
A total of 8 categories were evaluated to correlate CBCT measurements for maximum pericoronal width space in supero-inferior direction (S-I) in coronal sections and occurrence of pathologies in the specimens of pericoronal follicles (Fig. 10). Pathologic changes suggestive of a DC were highest among patients with a pericoronal follicular space width (S-I) of 1.60-1.80mm. Also, calcifications in the pericoronal follicles were higher in patients with a pericoronal follicular space width (S-I) of 1.20-1.40 mm. The difference was, however, statistically insignificant (p=0.145).

Abbreviations: A: Normal Pericoronal Follicles, B: Changes Suggestive of Dentigerous Cyst C: Calcifications in Relation to Pericoronal Follicles. Types: Type 1: Horizontal Impaction, Type 2: Mesioangular Impaction, Type 3: Distoangular Impaction, Type 4: Vertical Impaction.
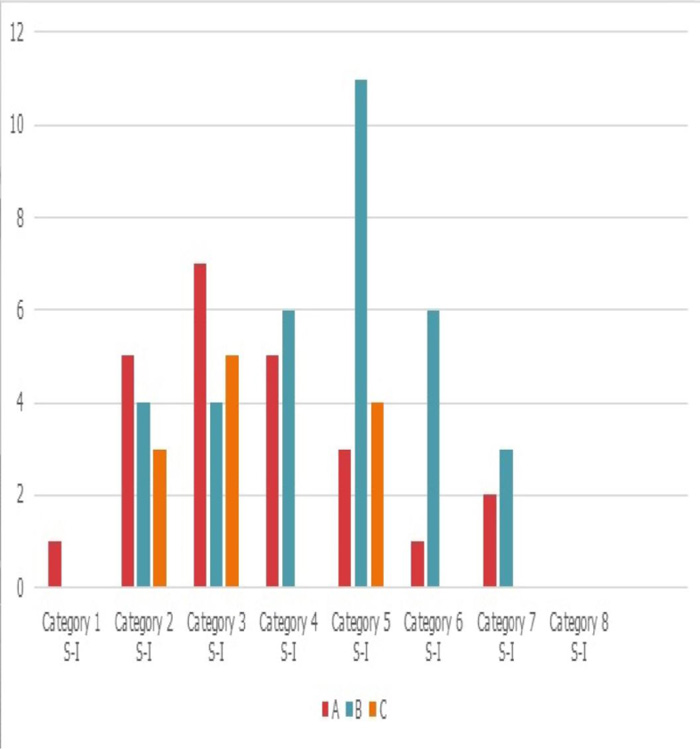
Abbreviations: A: Normal Pericoronal Follicles, B: Changes Suggestive of Dentigerous Cyst, C: Calcifications in Relation to Pericoronal Follicles, S-I: Supero-Inferior. Category: Category 1 S-I: 0.8-1.00mm, Category 2 S-I: 1.00-1.20mm, Category 3 S-I: 1.20-1.40mm, Category 4 S-I: 1.40-1.60mm, Category 5 S-I: 1.60-1.80mm, Category 6 S-I: 1.80-2.00mm, Category 7 S-I: 2.00-2.20mm, Category 8 S-I: 2.20-2.40mm.
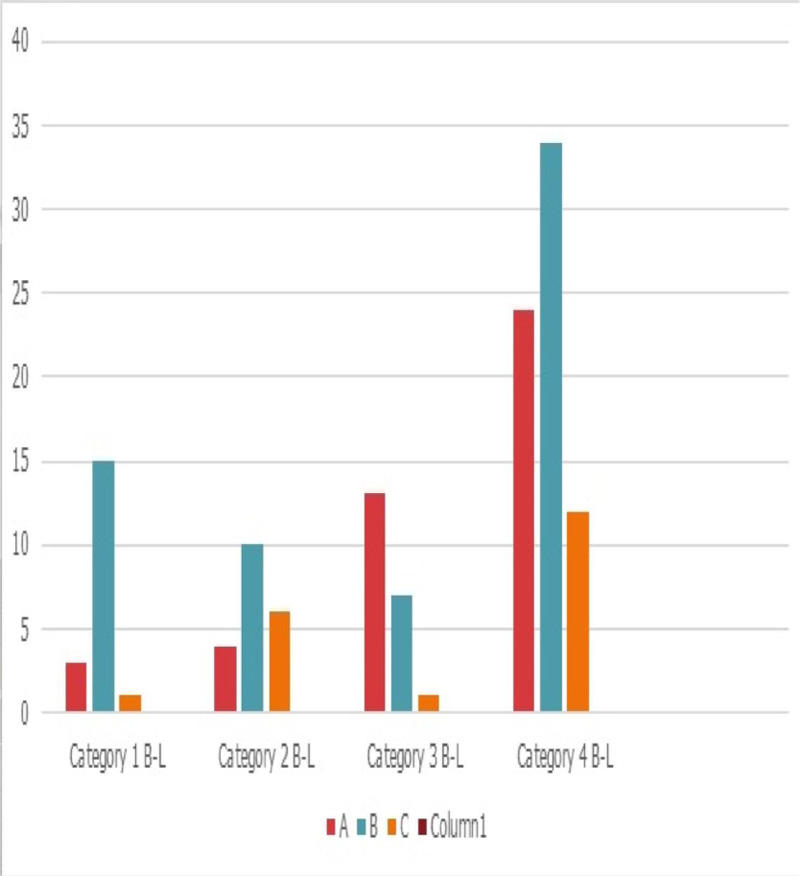
Abbreviations: A: Normal Pericoronal follicles, B: Changes Suggestive Of Dentigerous Cyst, C: Calcifications in relation to Pericoronal follicles, B-L: Bucco-Lingual, Category: Category 1 B-L: 8.00- 10.00mm, Category 2 B-L: 10.00-12.00 mm, Category 3 B-L: 12.00-14.00mm, Category 4 B-L: 14.00-16.00mm.
Association between CBCT measurements for maximum bucco-lingual pericoronal (B-L) width and occurrence of pathologies in the pericoronal follicles were noted in the coronal sections (Fig. 11). A total of 8 categories were compared. It was observed that the pathologic changes associated with DC were highest among patients with a pericoronal follicular space width (B-L) of 14.00-16.00mm. The difference was statistically significant, with a p-value of 0.001. Also, calcifications in the pericoronal follicles were higher when the pericoronal width space (B-L) was 14.00-16.00mm, and the least calcifications were category 3 with a pericoronal width space (B-L) of 12.00-14.00 mm. The differences were statistically significant (p=0.001).
A total of 8 categories were compared in the axial section to demonstrate the correlation between CBCT measurements for maximum pericoronal width space in the antero-posterior direction (A-P) and occurrence of pathologies in the specimens of pericoronal follicles (Fig. 12). Pathologic changes associated with DC were highest among category 7 patients with a pericoronal follicular space width of 20.00-22.00mm. The differences were statistically significant (p=0.001). Also, calcifications in the pericoronal follicles were highest among patients with an A-P width of 16.00-18.00mm.
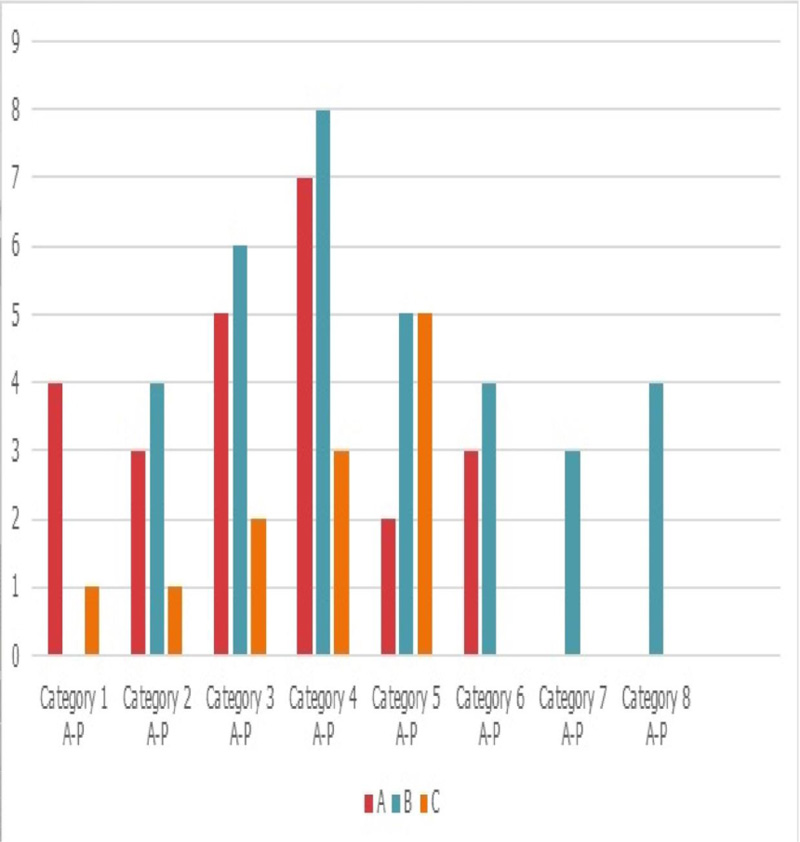
Abbreviations: A: Normal Pericoronal follicles, B: Changes suggestive of dentigerous cyst, C: Calcifications in relation to Pericoronal follicles, A-P: Antero-Posterior Category: Category 1 A-P: 8.00-10.00mm, Category 2 A-P: 10.00-12.00mm, Category 3 A-P: 12.00-14.00mm, Category 4 A-P: 14.00-16.00mm, Category 5 A-P: 16.00-18.00mm, Category 6 A-P: 18.00-20.00mm, Category 7 A-P: 20.00-22.00mm, Category 8 A-P: 22.00-24.00mm.
4. DISCUSSION
The present study correlates CBCT and histopathology in the diagnosis of pathologies associated with the pericoronal radiolucencies. Out of 70 subjects, a total of 24 patients showed normal dental follicles, whereas 34 patients revealed cystic changes suggestive of a dentigerous cyst. Wali et al. [4], in their study, correlated the radiographic appearance and histological findings of the cystic changes in impacted mandibular third molar among 30 patients indicated for extraction. Among the 30 follicles examined, 7 revealed changes indicative of DC, and the results were statistically significant. They observed that the cystic changes were more prevalent among males in comparison to females. However, the difference was statistically insignificant. A study by Yildirim [26]. on 120 patients (38 men, 77 women) to determine pathologic changes associated with impacted mandibular third molars and the importance of their prophylactic removal revealed a higher incidence of cystic changes in women when compared to men [5]. In our study, we observed a higher incidence of cystic changes in females in comparison to males, and the result was statistically significant (p=0.016).
Satheesan et al. [27] performed a histologic study of dental follicles of 50 impacted mandibular third molars and co-related it with pericoronal radiolucency surrounding them. They observed significant histopathological changes conforming to cystic changes in about 52% of the follicles. They concluded that as age increases, there is increasing evidence of calcification in the connective tissue of the follicle. Also, calcifications were found in 54 out of the 130 dental follicles of impacted mandibular molars examined by Cutright [28]. These observations were in accordance with our study, wherein we observed an increase in the incidence of calcific changes in the follicle in a slightly older age group (30 to 34-year-olds).
A study was conducted by Majidi et al. [29] on 201 dental follicles of impacted mandibular molars by assessing the pericoronal width of the molars on panoramic radiographs and further evaluating them under histopathologic sections. After evaluating the dental follicles, it was observed that 50.7% of cases (102 cases) showed pathological changes with follicular width of 0.21 to 8.8 mm, and all of them were diagnosed as DC. In our study, we noted that an increased bucco-lingual width of pericoronal follicular space observed in the coronal sections in CBCT was indicative of cystic changes. The measurements were statistically significant (p=0.0001).
Camargo et al. [30] performed a retrospective cohort study on radiographic databases of 26 patients with 49 impacted third molars who were assessed over 10 months. The evidence of cystic changes observed was 21.1%. The authors also observed that the prevalence of cystic changes was found to be highly associated with distoangular impactions. In our study, we observed a similar significant correlation between disto-angular impactions and cystic changes.
In the present study, we observed that the dental follicle surrounding an impacted tooth has the potential to differentiate into a wide variety of lesions. Thus, it is imperative to exhaustively evaluate the pericoronal follicular space surrounding impacted third molars. Conventional radiographs can provide a valuable estimation of the width of pericoronal follicles. However, it lacks the depth and precision needed to determine the exact location of the impacted mandibular third molar. CBCT provides a better and more superior imaging modality for the assessment of impacted mandibular third molars. It helps in assessing the pericoronal width, especially in the coronal and axial sections, thus providing a more thorough assessment of pericoronal space. In our study, the supero-inferior height was much lesser when compared to the bucco-lingual and antero-posterior dimension of the pericoronal space, which can be easily overlooked when assessing impacted mandibular molars using 2D imaging, thus signifying a greater need to implement CBCT imaging as a more accurate diagnostic tool for assessment of an impacted tooth.
Conventionally, the probability of occurrence of DC increases when the width of pericoronal radiolucency is above 2.50-3.00mm. However, in our study, it has been observed that when viewed under 3D imaging like CBCT, the pericoronal follicular space can be evaluated in different dimensions, and the values in different dimensions can be a more accurate predictor radiologically for the occurrence of pathologies when compared to 2D imaging.
The follicle around the asymptomatic impacted lower third molar can be associated with potentially significant pathologies, the most common of them being a cyst. Diagnosis of the lesion should not be based on radiographic evidence alone but also clinical evidence and microscopic examination of the sample. CBCT has the advantage of multiplanar 3D imaging (axial, coronal, and sagittal planes), which provides important information on the presence and extension of bone resorption, sclerosis, cortical expansion, location of the impacted tooth, and internal or external calcifications [31]. CBCT is a complementary tool in the diagnosis of pericoronal follicles surrounding impacted mandibular third molars, which could potentially develop into a DC or other pathologies.
CONCLUSION
In the present study, we conclude that there is a high probability for the follicle around an asymptomatic distoangular impacted lower third molar to become a warehouse of potentially significant pathologies like DC. Diagnosis of the lesion should not be based on radiographic evidence alone but also clinical evidence and microscopic examination of the sample. Our study highlighted that CBCT is a complementary tool for cases diagnosed with pericoronal follicles surrounding impacted mandibular third molars, which could potentially develop into a dentigerous cyst. Thus, it is advisable to incorporate a CBCT as a vital diagnostic tool to analyze impacted mandibular third molars and to make sure that the radiographic diagnosis should be followed by a histopathologic diagnosis for a better overall evaluation.
ETHICAL APPROVAL AND CONSENT TO PARTICIPATE
The approval was obtained from the Institutional Ethical Committee (Approval No-17031).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in full accordance with the ethical standards of the committee and with the Declaration of Helsinki of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent has been obtained from the patients.
STANDARDS OF REPORTING
STROBE guidelines and methodologies were followed in this study.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


