The Contemporary Management of Cleft Lip and Palate and the Role of Artificial Intelligence: A Review
Abstract
Introduction:
Cleft management is an exhaustive process for the patient, the orthodontist, and the caregiver. In recent decades, a wide number of challenges have been addressed with the inclusion of various dental specialties for the detection, diagnosis, and treatment of orofacial clefts. The orthodontist plays a very pivotal role during the overall management of children with cleft lip and palate as they need to make critical decisions for when to intervene orthodontically and at what stage to set priorities for individual treatment goals.
Objectives:
The objectives of this study were to provide an in-depth review of the evolving role of various disciplines focusing on orthodontics in the management of cleft cases.
Methods:
A general search was carried out to identify the published data on cleft lip and cleft palate management on PubMed and Scopus until the 1st of June 2021 using keywords such as cleft lip, cleft palate, cleft orthodontics, naso-alveolar molding, and surgical cleft orthodontics. The related literature was then reviewed and analyzed.
Results:
With improvements in 3D modeling, CT scans of patients can be used to construct precise 3D models, and these can be utilized to demonstrate various clinical issues related to clefts. The orthodontist has a major role in the various stages and steps, follow-up, treatment care, and outcome assessment. With the advent of technological advancements and artificial intelligence, the role is only going to evolve and expand further in the management of the cleft lip and palate. Diagnostic techniques utilizing artificial intelligence to detect cleft during the prenatal period have also been tested and have been shown to have a high rate of accuracy. The evolution of distraction osteogenesis came into the limelight as a revolutionary modality for cleft treatment. Computer-assisted orthognathic surgery is a widely used modality for reshaping the osseous defects of the maxilla in patients with congenital clefts. With the development of additional modalities such as aligners, patients that need to undergo complex orthognathic surgeries can also be treated with aligners without compromising the outcomes.
Conclusion:
The cleft lip and palate can be managed by a multi-disciplinary team. Orthodontics has an important role in the overall management of a cleft affected individual as they must make critical decisions regarding orthodontic interventions as well as set priorities for each treatment goal. With the advent of technological advancements and artificial intelligence, the diagnosis and management of the cleft lip and palate have become simplified.
1. INTRODUCTION
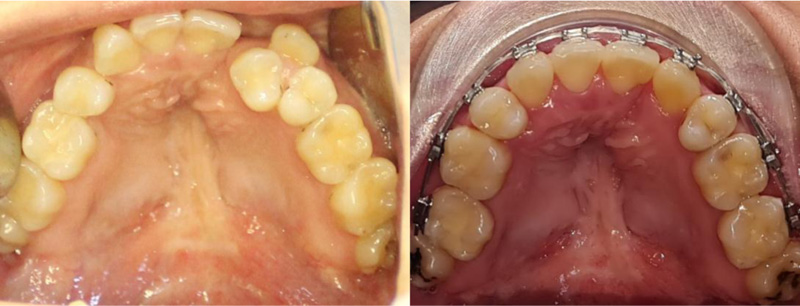
Since the beginning of the 20th century, orthodontics has found an ever-increasing role in managing cleft lip and palate cases. A wide variety of problems with the identification, diagnosis, and management of orofacial clefts have been solved in recent decades with various dental specialties [1]. On the one hand, orthodontics is involved in the usual fixed orthodontic treatment for non-cleft affected individuals and, on the other, offers treatment options for the clinical management of clefts starting from the neonatal period and extending to adult patients (Fig. 1A, 1B) [2, 3]. Treatment options include expanding the maxilla with the subsequent alignment of the teeth in their new positions to offer the patient improved esthetics.
2. THE EVOLUTION OF CLEFT CARE IN TERMS OF DIAGNOSTICS
Cleft management is an exhaustive process for the patient, the orthodontist, and the caregiver. Moreover, it extends for years and involves constant updates and communication regarding the progress [4]. The cleft management team has been around for the past few decades and has added considerably to the successful treatment of such cases. Another important factor has been the evolution of diagnostic aids such as cephalography and Cone-Beam Computed Tomography (CBCT) that have enabled the study of such cases with a focus on hard tissues and allowed for assessment of various treatment outcomes through comparison [5]. Several researchers have used CBCT imaging to demonstrate the effectiveness of treatment procedures such as alveolar bone grafting in cleft patients and even for precise analysis and estimation of the bone present at cleft sites [6]. With improvements in 3D modeling, CT scans of patients can be used to construct precise 3D models, and these can be utilized to demonstrate various clinical issues related to clefts. Soft tissues and bony structures are segmented from each scan based on intensity threshold and then reconstructed to form customized 3D models that can be utilized both for consultation and treatment planning [7].
3. THE EVOLUTION OF CLEFT CARE IN TERMS OF TECHNIQUES AND MODALITIES
Many cleft-treated patients previously reported speech and facial defects because of nasolabial surgical repair that hampers their social lives. This led to the evolution of techniques for their management, and Distraction Osteogenesis came into the limelight as a revolutionary modality for cleft treatment [8]. It involves the separation of osteotomized bone segments, which are then stimulated to form new bone, thereby increasing the length of the bone. It has found extensive uses in the treatment of both unilateral and bilateral cleft patients and other syndromic patients such as hemifacial microsomia. The evolution of temporary anchorage devices or mini-screws as they are more popularly called has added to the repertoire of orthodontists who can use these to carry out selective tooth movement without unwanted effects on the adjacent teeth [9]. With the development of additional modalities such as aligners, cleft patients needing complex surgeries can be treated without compromising the outcomes [10, 11].
4. THE IMPORTANCE OF DATA COLLECTION
One of the more critical issues in patients with congenital anomalies is diagnostic and treatment outcome-related data collection, which is time-consuming [12]. It provides essential information regarding successful outcomes and risk evaluation and helps improve the patient’s quality of life through treatment progress assessment. Successful outcomes for cleft afflicted individuals involve restoring oral functions and aesthetics of the nose, lips, and teeth, thereby improving the quality of life of an affected individual. Orthodontic diagnosis and treatment planning for cleft lip and palate affected individuals mostly follow the same principles for non-cleft patients with added considerations given to surgical interventions, the pattern of the cleft, associated deformities, and following through with the help of a multi-disciplinary team.
5. THE EVER-INCREASING ROLE OF ARTIFICIAL INTELLIGENCE
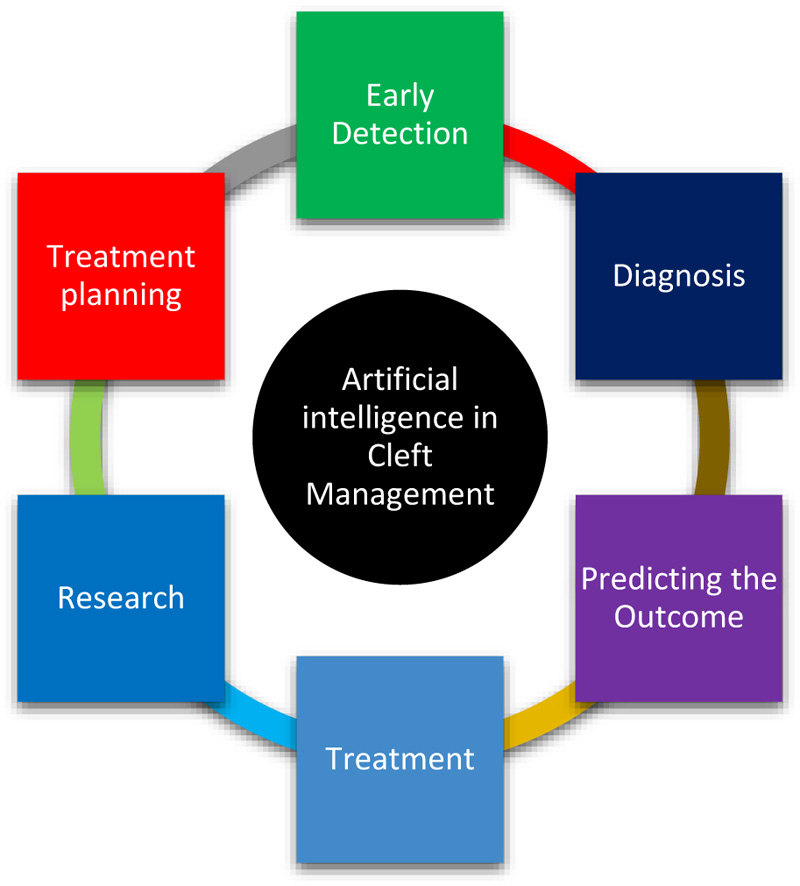
With more and more patient data being stored electronically, researchers have been exploring artificial intelligence and machine learning to improve outcomes of cleft lip and palate patients (Fig. 2). Machine learning can analyze previously stored data to develop efficient algorithms for knowledge acquisition and risk assessment. Previously conducted studies have shown that machine learning algorithms effectively created predictive models for single nucleotide polymorphisms and concluded that logistic regression was highly efficient [13]. Using artificial intelligence, the researchers demonstrated defective variations in genes that are commonly involved in the biosynthesis of vitamin A and folic acid, thereby confirming findings from other studies. Other studies have been conducted that have successfully detected cleft in the prenatal stage with 92 percent accuracy [14, 15]. Data were acquired from the patients that included information on gender, family history, number of siblings, habits, number of children, systemic concerns, among others, and used to predict the risk for cleft development.
Even though artificial intelligence still has limitations, it can be improved further to ensure more predictable outcomes when it comes to cleft diagnosis and management. It has tremendous potential in diagnostics, treatment planning, and even improvement of patient-to-doctor communication. There have been studies conducted on the facial attractiveness of cleft treated patients, and it was seen that the ratings delivered by both humans and artificial intelligence were similar, which suggests it could become a more valuable tool in the future for treatment planning and analysis of post-treatment results [16]. Diagnostic techniques utilizing artificial intelligence to detect cleft during the prenatal period have also been tested and shown to have a high accuracy rate [17]. These have been studied using various criteria such as gender, familial history, number of children, smoking habit, and history of miscarriage and were found to have more than 90 percent accuracy, which suggests artificial intelligence could have a profound role to play in cleft prediction in the future.
6. COMPUTER-ASSISTED SURGICAL PLANNING FOR CLEFT PATIENTS
Orthognathic surgery is a widely used modality for reshaping the osseous defects of the maxilla in patients with congenital clefts. It can help restore facial soft tissue balance and bring about significant esthetic change in a cleft-affected individual. Achieving a successful result needs sound surgical technique, orthodontic management, and precise planning for alignment before the surgery. Most orthognathic surgical procedures are still planned with two-dimensional cephalometry, but slowly, there is the transition towards three-dimensional simulations [17]. 3D planning can help a patient and the dentist to reach a consensus easily on the treatment plan by utilizing a simulation based on more information. 3D planning is also being utilized with computer-aided manufacturing (CAD/CAM) to produce splints and has shown highly accurate results. 3D simulations have demonstrated higher information yield than their 2D counterparts and render accurate information in complex cases, thereby improving the outcome of the surgeries.
7. ORTHODONTIC INTERVENTION
An orthodontist has a significant role in the overall management of a cleft affected individual as they must make critical decisions regarding orthodontic interventions and set priorities for each treatment goal. Orthodontic treatment is most effective in the rehabilitation phase following orthognathic surgery or as an adjunctive modality for alveolar bone grafting. In younger patients in early mixed dentition, alveolar grafting is more successful than adult patients with mixed dentition, where a combination of surgery and fixed orthodontic treatment has traditionally yielded better results [18].
8. LIMITATIONS
At present, the neural network architecture is inherently complex, with many hidden layers with values that cannot be interpreted and demonstrate the presence of a non-linear layer-to-node relationship [19]. A significant limitation is that artificial intelligence relies heavily on algorithms, and till it reaches a stage where its functioning is transparent, understandable, and reliable, it cannot be fully incorporated into dentistry as an aid (Fig. 3). Since patient treatment success largely depends on the orthodontist’s communication skills, rapport, behavior modification, and emotional status of the patient, there are many factors still missing from the artificial intelligence armamentarium. Also, machine learning models require large amounts of energy and emit high levels of CO2, which are added limitations to widespread implementation across all branches of dentistry [20].

CONCLUSION
There has been significant improvement in managing the cleft lip and palate. A multi-disciplinary team can manage the cleft lip and palate. With the advent of technological advancements and artificial intelligence, diagnosing and managing the cleft lip and palate have become simplified. With improvements in 3D modeling, CT scans of patients can be used to construct precise 3D models, and these can be utilized to demonstrate various clinical issues related to clefts. The orthodontist has a significant role in the various stages and steps, follow-up, treatment care, and outcome assessment. With the development of additional modalities such as aligners, patients that need to undergo complex orthognathic surgeries can also be treated with aligners without compromising the outcomes.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


