All published articles of this journal are available on ScienceDirect.
The Use of Magnetic Resonance Imaging in Diagnostics of Radix Paramolaris: A Case Report
Abstract
Background and Objectives:
This case report aims to present a rare morphological variation of Radix Paramolaris (RP) diagnosed using Magnetic Resonance Imaging (MRI) to discuss its morphological associations and possible implications on dental treatment. Radix paramolaris is a buccally located supernumerary root of the permanent mandibular molars. It is very rare in the European population, with a prevalence below 4%.
Case Presentation:
A 7-year-old boy with severe Class II malocclusion is presented. The first phase of orthodontic treatment consisted of therapy with a removable activator appliance. Before the second phase of treatment, unilateral radix paramolaris on the second right permanent mandibular molar was discovered.
Results:
Supernumerary root was diagnosed using a 3T whole-body MRI system. This case confirmed the association between supernumerary roots and increased buccal crown cusps in a mandibular molar. Furthermore, it demonstrated the effectiveness of non-invasive MRI as a complementary diagnostic tool, offering clear advantages in diagnosing rare morphological variations such as supernumerary roots. Unlike conventional radiography, MRI is able to distinguish the soft tissues, including the dental pulp, and does not emit ionizing radiation.
Conclusion:
To diagnose a supernumerary root and the state of its pulpal tissue, a precise radiographic and clinical examination is required since awareness of exact root morphology can be of paramount importance in clinical decision-making for several dental procedures.
1. INTRODUCTION
Permanent Mandibular Molars (PMM) usually have two roots: mesial and distal [1]. In certain cases, a supernumerary third root is present. Depending on the anatomic location of the supernumerary root, it is either called Radix entomolaris (RE) if it is located lingually or Radix paramolaris (RP) if it is located buccally [2, 3]. Both RE and RP may be separate or fused with other roots. In comparison with the other roots, they are much more morphologically variable [2]. Their dimensions may vary from a fully independent root with its own root canal or just a simple, conical extension [2]. RP is often curved and slender, containing a round root canal. The exact cause of RP formation is unknown. Supernumerary roots could be related to external factors during odontogenesis or the penetrance of a gene or polygenetic system [4]. Higher prevalence in certain populations suggests hereditary association [5].
The presence of RE/RP in PMM is often associated with certain ethnic and racial backgrounds [6]. It is less prevalent in Europe or Africa and more frequent in Asian or Arctic populations [7-9], while in the Slovenian population, its prevalence was estimated to be approximately 0,68-1,33% [10]. Among the permanent mandibular molars, supernumerary root (either RE or RP) is least prevalent in the second PMM [10]. The prevalence of RP is even lower when compared to RE [2]. Studies found no difference in a predilection for a supernumerary root in PMM among genders, and it appears on the right and left side equally frequently [11]. It can appear either uni- or bi-laterally [12]. However, when identified, the possibility of bilateral supernumerary PMM root should be considered [10].
RP can rarely be identified clinically by thoroughly examining the morphology of the crown for an extra cusp (tuberculum paramolare), by observing irregularly prominent cervical morphology, by periodontal probing for an additional root, or by during an extraction procedure [13]. Periapical and panoramic radiography is the most frequently used method for diagnosing supernumerary PMM roots. However, 2D methods could be inaccurate because of the possible superimposition of the same structures, as they are only a projection of three-dimensional (3D) objects [6]. Authors suggest the use of 3D diagnostic methods such as CBCT as they are able to diagnose a supernumerary root of PMM more accurately [14].
A supernumerary PMM root could be both a therapeutic and diagnostic challenge [15]. An additional, often narrow and curved root canal has to be carefully negotiated and shaped [3]. In periodontics: supernumerary PMM root can accelerate the progression of the periodontal disease on PMM, or supernumerary root could be broken during exodontia [3, 16, 11].
Magnetic resonance imaging (MRI) is a state-of-the-art sensitive and non-invasive imaging method, which allows a precise differentiation of dental pulp status [17-20]. In addition, the MRI results are in good agreement with findings in histological sections of identical teeth [17]. It is the only imaging tool that allows a precise presentation of soft tissues (dental pulp) inside hard dental tissues (enamel, dentine) in vivo in humans [17-20]. MRI imaging was successfully applied in the diagnosis of tooth vitality following dental trauma, quantification of dental pulp response to the caries progression, and determination of the anatomy of dental pulp [17-22]
The aim of this case report is to present a rare morphological variation of RP diagnosed using state-of-the-art MRI Imaging to discuss its morphological associations and possible implications for orthodontic treatment.
2. CASE REPORT
The case report followed the CARE reporting guidelines (CARE list in appendix). A 7-year-old boy of Caucasian origin without systemic conditions or orofacial syndromes was referred to the Department of Orthodontics and Dentofacial Orthopedics, Faculty of Medicine, the University of Ljubljana due to severe Class II malocclusion, increased overjet, altered visual appearance, and deviated orofacial functions. Clinical examination revealed mouth breathing, a visceral type of swallowing pattern, open mouth posture, and biting of the lower lip. When asked, the patient could obtain lip closure only with strain in mentalis and orbicularis oris muscles.
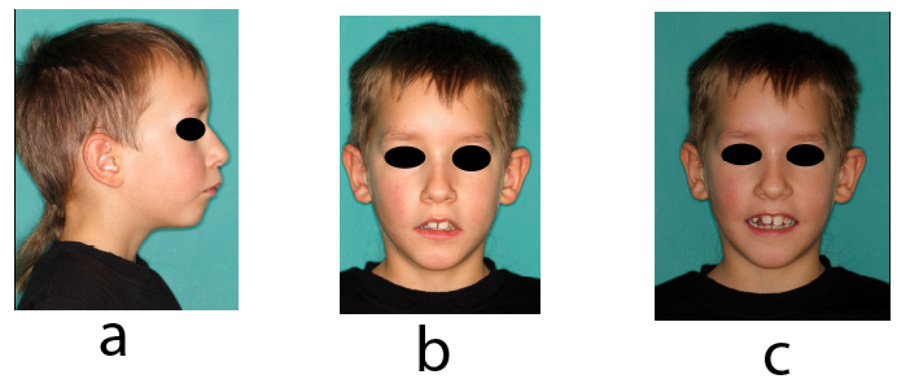
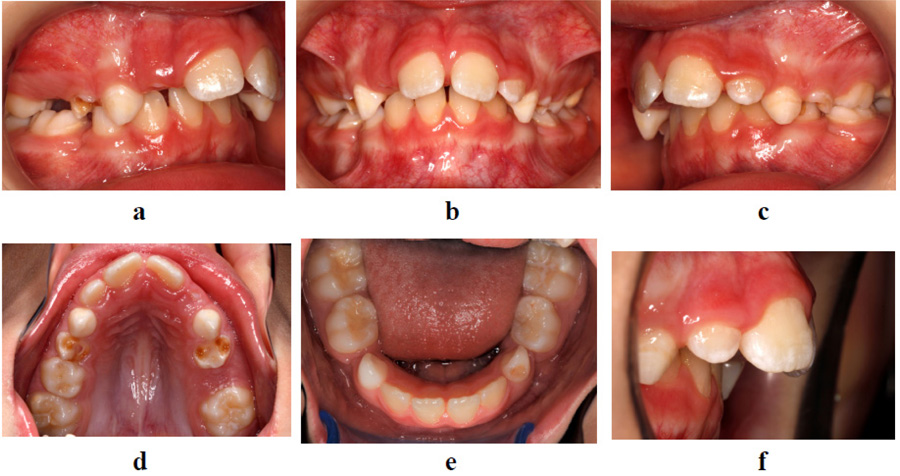
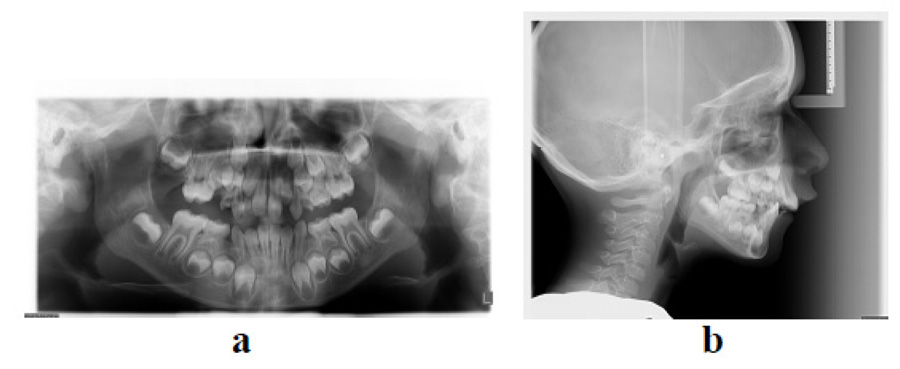
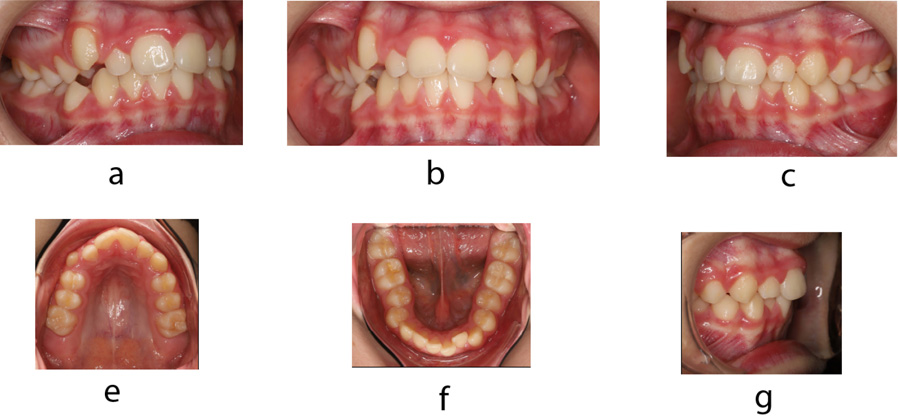
The patient had an asymmetric face with a convex facial profile. According to Schwarz typology [23], it was classified as an anteposition with retroinclinations (Fig. 1). Intraorally, the patient exhibited a Class II molar relationship, severely increased overjet (12 mm), and several carious deciduous teeth (Fig. 2). In addition to the general and dental history, photographs and impressions were taken, and panoramic and lateral x-rays were made (Fig. 3). Analysis of lateral cephalogram showed prognathic upper jaw and retrognathic lower jaw, skeletal Class II relationship, and borderline hyperdivergent (vertical) skeletal pattern (Fig. 3 and Table 1).
| - | Measurement | Unit | Before Treatment | After Treatment | Change | Norm |
|---|---|---|---|---|---|---|
| Saggital relations | SNA | ° | 84,4 | 79,9 | -4,5 | 82 |
| SNB | ° | 74,2 | 74,2 | 0 | 80 | |
| ANB | ° | 10,2 | 5,7 | -4,5 | 2 | |
| Wits appraisal | mm | 8,7 | 3,6 | -5,1 | 0,5 | |
| SNPg | ° | 74,1 | 74,2 | +0,1 | 81 | |
| U1-APg | mm | 9,1 | 8,9 | -0,2 | 2 | |
| Vertical relations | Palatal plane/SN | ° | 9,9 | 11,3 | +1,4 | 9 |
| Mandibular plane/SN | ° | 45,2 | 44,4 | -0,8 | 32 | |
| Palatal/mandibular plane | ° | 35,2 | 33,0 | -3,2 | 24 | |
| Bjork | ° | 405 | 404,4 | -0,6 | 396 | |
| Gonial angle | ° | 127 | 128,9 | +1,9 | 120 | |
| Dental relations | U1/Palatal plane | ° | 108,3 | 116,2 | +8,9 | 109 |
| U1/NA | ° | 19,5 | 27,2 | -7,7 | 22 | |
| U1-NA | mm | 1,6 | 6,3 | +4,7 | 4 | |
| L1/Mandibular plane | ° | 84,8 | 97,6 | +12,8 | 90 | |
| L1/NB | ° | 18,7 | 34,0 | +15,3 | 25 | |
| L1-NB | mm | 2 | 9,4 | +7,4 | 4 | |
| Interincisal angle | ° | 131,7 | 113,2 | -18,5 | 135 |
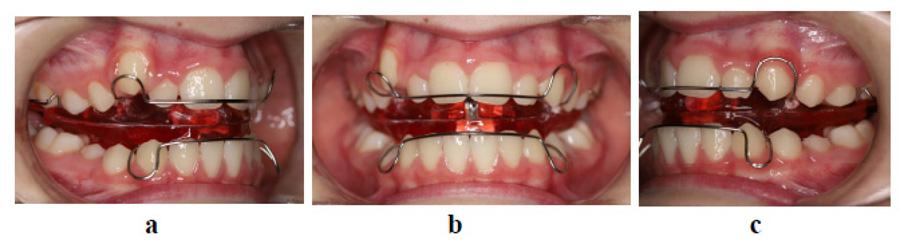
Objectives of the first phase treatments were to improve sagittal relations, reduce overjet, improve facial profile and allow a competent lip seal. Due to the patient’s young age and growth potential, functional treatment with growth modification was selected. The patient was treated with a removable functional activator appliance, which has previously been shown as very effective in early Class II/1 treatment [24, 25]. The patient was instructed to wear the appliance at least 10 hours daily; the patient was compliant with appliance wear. Active functional treatment lasted around 2 years (Fig. 4).
At the age of 12, new records were taken in order to plan the second phase of treatment. New photographs, intraoral scans, and x-rays were made (Fig. 5-7). After treatment, Class I molar relationship with normal overjet was obtained, the facial profile has improved. Panoramic x-ray indicated the presence of supernumerary root on the second right molar (Fig. 7). Analysis of lateral cephalogram showed improvement in parameters of sagittal relations, especially ANB, Wits appraisal, and SNA. There were no significant changes in vertical relations. Dental relations analysis noted proclination of both upper and lower incisors (Fig. 7 and Table 1).
Lateral cephalograms were traced, and general superimposition and maxillary and mandibular superimpositions were made according to Bjork’s structural method [ 26, 27]. During the first phase of treatment, the patient grew intensively. Relative to the stable structures of the anterior cranial fossa, the maxilla grew anteriorly and inferiorly with only a slight anterior rotation. Mandible grew forward and downward with a notable posterior rotation (Fig. 8).
Before the second phase of treatment, moderate dental crowding with incisor proclination was diagnosed. Therefore premolar extractions and fixed appliance treatment were planned.
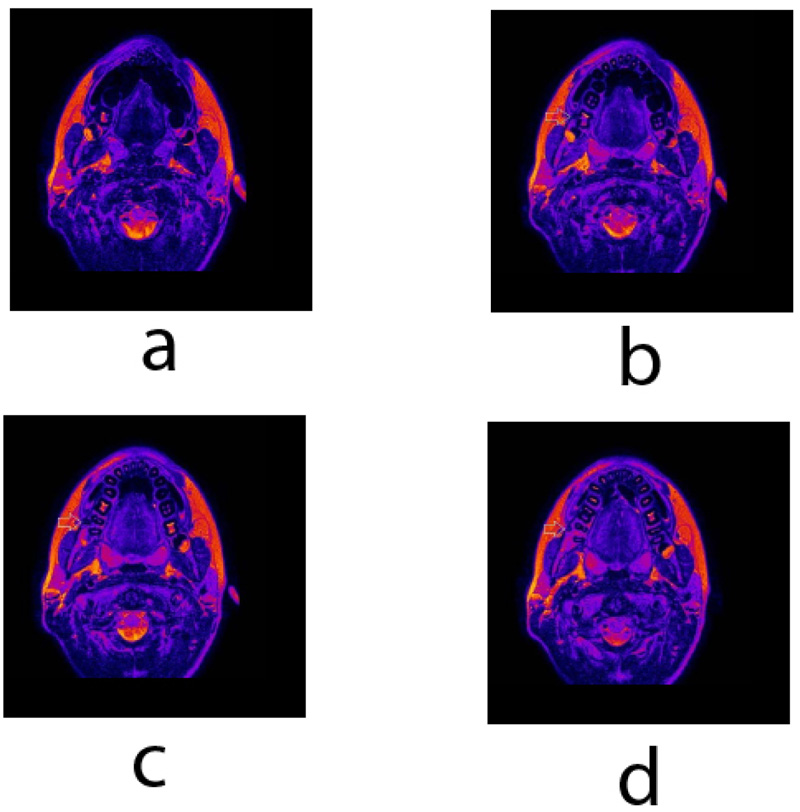
Besides the conventional diagnostic tools, teeth and jaws were scanned using clinical 3T whole-body Magnetic resonance imaging (MRI) system (TX Achieva, Philips, Netherlands) with a maximal gradient strength of 80 mT/m and the use of an S Flex coil. A T2 weighted turbo spin-echo (TSE) imaging in the transversal plane was performed with the following parameters: TR/TE 3000/100 ms, TSE factor 15, matrix 315 x 180, NSA 1, voxel 0.57 x 0.72, and FOV 181 x 144 mm. MRI slice thickness was set at 2.0 mm. MRI scans revealed a unilateral supernumerary root with an independent pulpal canal on the second permanent mandibular molar on the right side. The root is fully separated and is located buccally (Fig. 9). MRI T2 weighted TSE image in the transversal plane shows right second PMM (Fig. 9), its dental pulp extends buccally from the pulpal chamber into a round root – radixparamolaris.



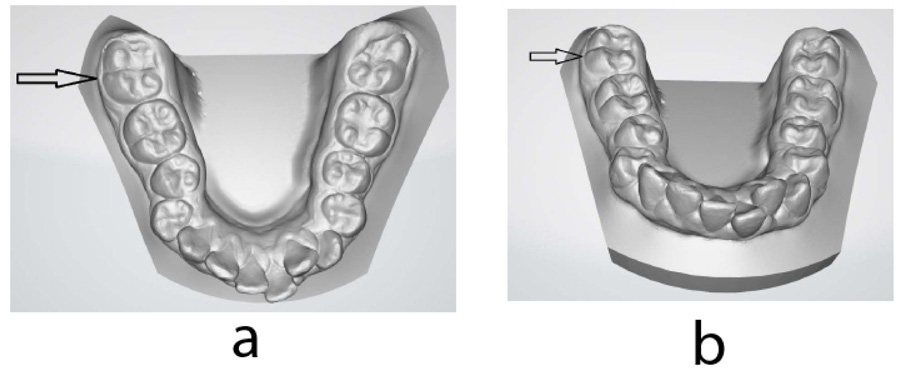
Intraoral models were obtained using a three-dimensional (3D) intraoral scanner (iTero Element, Align Technology, USA). Detailed examination of the intraoral model revealed additional buccal- protostylid-like cusp (Fig. 10). The diagnosis of radix paramolaris (RP) was made based on the findings.
3. DISCUSSION
The case study presented an early treatment of a preadolescent boy with severe Class II malocclusion. The first phase treatment with an activator functional appliance improved both orofacial functions and morphology; treatment effects were consistent with previously reported studies [24, 25]. Before the second phase of orthodontic treatment, a very rare accidental discovery of RP was made. Supernumerary root in second PMM is a rare finding, and according to the study of Strmšek and Štamfelj, it is the least prevalent in second PMM in the Slovenian population [10].
RP was diagnosed using an MRI system. MRI is a sensitive imaging method, which has been previously used for imaging and investigation of dental and periodontal tissues [17, 20, 28, 29]. Two-dimensional radiographic methods such as periapical or panoramic x-rays are (because of possible overlapping of anatomical structures) considered limited tools and less ideal for detecting supernumerary PMM roots [15, 30]. Even though the endoral radiographs are not the most sensitive diagnostic test for supernumerary roots, they are still the most commonly used in dental practice. Several techniques of tube disparallelism in a silicone guide have been proposed in order to improve their diagnostic sensitivity [31].
The use of 3D imaging, e.g., micro-CT or CBCT, enables a more accurate determination of morphological variations such as supernumerary roots [14, 32]. The latter mentioned fact is of clinical importance because supernumerary PMM roots tend to be smaller, curved, and with a higher degree of morphological irregularity [3, 9, 13]. Our case demonstrated MRI to be sensitive and accurate enough to detect morphological variations such as supernumerary roots and can be used to determine the presence and state of the dental pulp in the root canal, as opposed to CT techniques it does not emit ionizing radiation. Therefore MRI may also be used in children during growth and development [33, 34]. A possible limitation of MRI imaging is a longer scan time, besides the higher cost, which might lead to increased patient anxiety or claustrophobia [35, 36].
It is further reported that the supernumerary PMM root with an additional root canal is often associated with an increased number of cusps; usually, an additional cusp is observed on the buccal side of the crown (protostylid) [13, 6]. It should be noted, however, that vice versa may not always be the case; an increased number of cusps may not be related to the increased number of PMM roots [6]. In this case, we observed an additional rudimentary buccal, protostylid-like cusp on the PMM with RP only. The use of digital 3D models can provide the clinician with additional tools to allow or to alleviate the identification of morphological signs indicative of possible supernumerary roots. Further development of artificial intelligence might allow automatization of special morphology recognition, indicating the possibility of special morphological features such as supernumerary roots [37].
A precise radiographic and clinical examination is therefore required for the identification of the supernumerary PMM root. Understanding exact root morphology can play an important role in planning and can increase the chances of successful treatment in endodontics, periodontology, or exodontal procedures. Apart from better-documented challenges because of supernumerary PMM root in endodontics, periodontics and oral surgery literature regarding the effects of supernumerary PMM root effects on orthodontic treatment is far less extensive. It may be speculated that supernumerary PMM root could inhibit the movement of the PMM with supernumerary root because of the increased periodontal surface attachment [11, 38]. The cervical convexity of the PMM crown could also impinge on the placement of the molar bands.
CONCLUSION
Rare morphological features such as supernumerary roots present a significant diagnostic challenge. Considering the sensitive and non-invasive nature of the MRI, this case demonstrated contemporary MRI to be a useful tool for diagnosing rare morphological variations such as supernumerary roots of PMM, enabling diagnosis of the supernumerary root, its shape, presence of root canal, the shape of the root canal and allowing assessment of pulpal state.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Republic of Slovenia National Medical Ethics Committee, approval number 0120-659, 21th Dec 2017.
HUMAN AND ANIMAL RIGHTS
No animals were used in this study. The study was conducted according to the guidelines of the Declaration of Helsinki.
CONSENT FOR PUBLICATION
Written and oral informed consent was obtained from the patient and his parents to publish his records.
STANDARDS OF REPORTING
CARE guidelines and methodologies were followed for this study.
AVAILABILITY OF DATA AND MATERIALS
Data available on request due to restrictions because of privacy. Data in the manuscript belongs to a patient and is therefore protected as personal information.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The orthodontic treatment described in the manuscript was performed at the Department of Orthodontics and Orofacial Orthopedics, Faculty of Medicine, University of Ljubljana, Hrvatski trg 6, Ljubljana, Slovenia.
Records, including a statement of informed consent, are safely kept at the Institute of Physiology. MRI imaging, analysis, case data integration, and interpretation were performed at the Institute of Physiology and Center for Clinical Physiology, Faculty of Medicine, University of Ljubljana, Zaloska Cesta 4, Ljubljana, Slovenia.


