All published articles of this journal are available on ScienceDirect.
Conduction of Third Molar Extraction with the Presence of Retromolar Canal: A Case Report
Abstract
Introduction:
The retromolar canal is a structure rarely identified in clinical practice. The content of this canal is composed of nerves, arteries and venous plexus that give innervation and irrigation to the third molar region and the vestibular mucosa of molars and lower premolars. Thus, knowledge of the presence of this structure is important in dental procedures, due to the complications that damage to this structure can cause.
Methods:
In this report, a 19-year-old patient sought dental care at a clinic, Dentistry course at the Federal University of Santa Maria for the extraction of third molars due to hygiene difficulties. On radiographic examination, a retromolar canal was identified at the distal of the left mandibular third molar. With the identification of this structure, preventive measures were performed during the procedure to avoid complications.
Results:
With adequate planning and prevention measures, the trans and postoperative periods occurred without any complications.
Conclusion:
The foramen and the retromolar canal may occasionally appear in the clinic radiographic routine of the Dentist, and the professional should be attentive to the management of these anatomical structures during surgical procedures to avoid accidents and complications.
1. INTRODUCTION
Knowledge about the anatomy and morphology of the face and neck region and variations in normality is paramount for the clinical practice of the Dentist. One of these anatomical variations is the retromolar canal commonly neglected in anatomy textbooks.
The retromolar canal was first described in 1967 by Schejtman et al. [1]. This canal derives from a branch of the mandibular canal due to a failure in the fusion of the primitive canal during the prenatal period [2]. It presents an upper and anterior path, to the distal of the third molar, to emerge through the retromolar foramen in the region of the retromolar fossa [3]. It is composed of nerves, arteries and venous plexus that give innervation and irrigation to the third molar region and the vestibular mucosa of molars and lower premolars [1].
Knowledge of the presence of this structure is essential to avoid complications during surgical procedures involving the retromolar region such as bone grafts, implants, osteotomy, and extraction of third molars. The literature mentions cases of failure to obtain analgesia when using classical anaesthesia techniques. There are reports of cases of retromolar foramen injury that caused infections, paraesthesias, damage to adjacent muscles and even haemorrhages [4,5]. That being said, this case report aims to explain the necessary care and management in extraction of a third molar that had proximity to the retromolar canal.

2. CASE REPORT
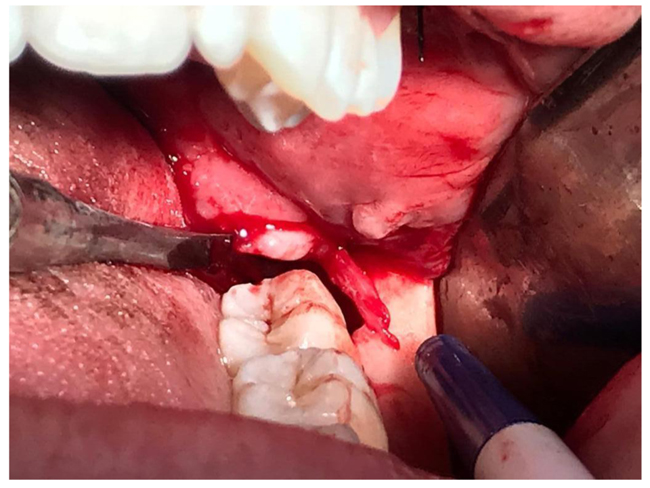
A 19-year-old female patient sought care at a clinic, Dentistry course at the Federal University of Santa Maria for the extraction of third molars because she had difficulty performing proper oral hygiene. No systemic or local alterations were observed in the anamnesis and clinical examination. A panoramic radiograph was requested as a complementary examination for the evaluation and planning of the case. During radiographic analysis, a radiolucent band was observed circumvented by two radiopaque lines, which connected the mandibular canal to the distal of element 38, which was diagnosed as the retromolar canal (Fig. 1). The treatment chosen was the exodontia of elements 38, 28 and 18. For the first session, the exodontias of elements 28 and 38 were planned. The patient was informed of the possible risks, demonstrated understanding, agreed to undergo the procedure and signed the Free and Informed Consent Form. With the knowledge of the proximity of the retromolar foramen with element 38 and possible complications, preventive measures were taken such as the arrangement of haemostatic tweezers and topical haemostatic to contain possible haemorrhagic conditions in the transoperative period; the anaesthetic technique was modified so that the nerve plexus of the canal obtained analgesia. In addition, the incision, osteotomy and dislocation of the tooth were also modified so that the foramen was not injured. In the trans operative period, after the extraction of element 38, it was possible to visualize the foramen and vascular plexus of the retromolar canal (Fig. 2). There was no haemorrhage or any other complications, because, during the procedure, we increased the anaesthetic dose with ½ tube in the posterior region to the third molar with infiltration of mepivacaine 2% with 1:100.000 adrenaline in order to increase local vasoconstriction. One week after the procedure, the patient returned for removal of the suture without reporting any problems.
3. DISCUSSION
The retromolar canal is an offshoot of the mandibular canal. It follows a recurrent path and emerges through the retromolar foramen to reach the medial region of the retromolar fossa. It is composed of a vascular nerve bundle that irrigates and innervates part of the temporal muscle and the buccinator muscle,
Haas et al. [3] in their systematic review and meta-analysis found different prevalences of a retromolar foramen in situ between 3.2 and 13.22% reaching up to 25% in the study by Bilecenoglu and Tuncer [6]. These varied results are related to ethnic diversity, genetics, environmental factors as well as the different methods of evaluation and sample size of the studies [3]. The prevalence between sexes is equivalent and it seems that the incidence of the retromolar canal is higher than one imagines [7].
Panoramic radiography is widely used in the planning of extractions of third molars, being an effective method for preoperative evaluation of impacted third molars [8], for example. However, the canal and the retromolar foramen seem to be more easily identified in multislice and cone beam computed tomography scans than in panoramic radiographs [3], because they are structures that may go unnoticed during the analysis of panoramic radiography due to overlap of anatomical structures, the small diameter of the canal and possible deficiencies in image processing [9, 10]. It is important to be attentive to the imaging examination during the planning of the surgical procedure so that unexpected complications in the trans and post-surgical procedures are avoided due to the proximity of the retromolar foramen and third molar with an average of 1mm, 4.23mm [2] and 10.5 mm [1], which shows that its location is variable.
Studies cite the retromolar canal as possibly responsible for the failure to obtain complete analgesia by classical anaesthetic techniques in the 38 area [11, 12]. In view of this, in the case reported, after performing the direct anaesthetic technique for a sensory block of the lower alveolar nerve and lingual nerve, 0.9 ml of anaesthetic was injected into the retromolar region to ensure complete sensory block of the region as well as local vasoconstriction. Oliveira-Neto et al. [13] reported a haemorrhagic case during the extraction of a third molar with the presence of a double retromolar foramen discovered during procedure; haemostasis was obtained only after compression of gauze soaked with an anaesthetic solution with a vasoconstrictor.
In addition to modifying the anaesthetic technique and the incision, osteotomy was performed in the alveolar bone from the mesial third to the middle third of the vestibular face of the third molar, so as not to damage the canal. In dislocation, instead of using a straight lever at the distal of the third molar, we opted for the use of the Pott Lever, directing the tooth up and to the lingual in order to avoid rupture of the component artery of the canal.
There is still no consensus in the literature on the aetiology of paraesthesia after dental surgery, but it is believed that anatomical variation and the presence of numerous foramina and accessory mandibular canals are associated [14]. Kikuta etal. report a case of paraesthesia in the vestibular mucosa in the lower molar region after surgery of an impacted third molar, whose canal and foramen was 2.9 and 2.3 mm in diameter, respectively. The patient also presented sensorineural disorder at the follow-up of 12 months after surgery [9].
Injuries to the structure in the mucoperiosteal detachment step may occur [4]. In the present case, the lower third molar was in Pell & Gregory's I-B position [15]. Thus, the incision was carefully made on the mesiovestibular third of the third molar extending to the mesial of the first molar, with a vertical incision anterior to the interdental papilla towards the groove fundus to avoid rupture of the retromolar canal, since the retromolar canal and the third molar appeared, radiographically, to be united. After the exeresis of the dental element, one can observe the vasculonervous bundle of the retromolar canal.
CONCLUSION
The foramen and retromolar canal may occasionally appear in dental patients. Therefore, it is important for the professional to have knowledge about these anatomical structures to carefully plan the surgical procedure, such as extractions of third molars, in order to avoid accidents and perform the proper management of possible complications during the procedure.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
The data sets used during the current study can be provided from the corresponding author [N.A] ,upon reasonable request.
STANDARDS FOR REPORTING
CARE guidelines and methodology were followed to conduct the study.
FUNDING
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) – Finance Code 001.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


