Performance of Bioceramic-based Root Filling Material with Artifact Reduction Properties in the Detection of Vertical Root Fractures Using Cone-beam Computed Tomography
Abstract
Introduction:
In Cone-beam Computed Tomography (CBCT) images, metallic artifacts by root filling materials reduce the quality of images. It seems that bioceramic sealers produce fewer artifacts than gutta-percha. In this situation, the possibility of VRF detection could increase, and therefore, flap and exploratory surgery would not be needed. The purpose of this study was to evaluate the performance of a bioceramic-based root filling material in the detection of Vertical Root Fractures (VRF) in CBCT imaging.
Materials and Methods:
This study was conducted at the dental school from March to August 2019, and 100 healthy human mandibular premolar teeth were obtained and randomly divided into two equal groups. The teeth were filled with either AH26 and gutta-percha or bioceramic root filling materials. VRF was induced on half of the decoronated teeth in each group using a Global Testing Machine, and the others were considered control. CBCT imaging was performed by the Cranex 3D machine. Comparisons of the 2 groups were made using the Mann-Whitney test.
Results:
There was a significant difference between the two groups of bioceramic and gutta-percha in the measured indices, including sensitivity (P=0.017), specificity (P=0.018), positive predictive value (P=0.018), negative predictive value (P=0.018), and accuracy (P=0.011). The Area Under Curve (AUC) also showed a significant difference between the two groups (P=0.011). According to Kappa test results, no significant difference was obtained between the findings of the two observers.
Conclusion:
Different root filling materials showed a different extent of artifact in CBCT images. Bioceramic root filling material induces fewer artifacts in CBCT images, and the diagnostic value of VRF in CBCT images in the root canals filled with it is greater than those filled with AH26 and gutta-percha.
1. INTRODUCTION
According to the American Association of Endodontists (AAE), Vertical Root Fracture (VRF) refers to any complete or incomplete fracture that begins at any level of the tooth root, especially the buccolingual. It occurs from intra-dental fissures, develops over time, and happens due to chewing or any pressure-related stresses [1].
Because the fracture line may not be visible and the symptoms are similar to periodontal diseases or unsuccessful root canal treatments, VRF is difficult to diagnose. Since bone resorption around the fracture continues until tooth removal, an early and accurate diagnosis of fracture is essential [2, 3].
VRF diagnostic methods include exploratory surgery, two-Dimensional (2D) radiography, and three-Dimensional (3D) computed tomography imaging. Exploratory surgery in some patients should be performed with more caution, such as in people with blood coagulation problems or patients susceptible to osteomyelitis and who have a history of radiotherapy or chemotherapy. The two-dimensional conventional radiographic images superimpose the bone structures, resulting in inaccurate detection of root fractures, especially when the X-ray orientation is not parallel to the fracture line [4, 5]. The unclear clinical symptoms and low sensitivity of conventional radiographs in the detection of VRF are often a diagnostic problem for the dentist [3, 6]. Therefore, the development of alternative imaging systems to improve VRF detection is required [7, 8]. Cone-Beam Computed Tomography (CBCT) imaging has been widely accepted in endodontics dentistry for its ability to produce high resolution, sensitive, and accurate 3D images [9, 10].
Although CBCT has had a promising result in the diagnosis of VRF, dense endodontic materials such as gutta-percha (GP), metal posts, and crowns produce metal artifacts in CBCT images, resulting in reduced image quality which makes detection of root fractures difficult [11]. Beam Hardening (BH) artifact is one of the most important artifacts that reduce image quality. Dense gutta-percha cones are composed of non-inorganic components such as zinc oxide and barium sulfate, which contribute to the radioactivity of gutta-percha [12].
Recently, bioceramic sealers have been widely used due to their extraordinary properties in dentistry. Bioceramics are actually ceramics used in today's dentistry. Different materials such as zirconia, alumina, bioactive glass, hydroxyapatite, and absorbable calcium phosphate have been used in the structure of these sealers [13]. Bioceramics are non-toxic sealers with good radiopacity, biocompatibility, antibacterial activity, and root dentin bonding that produce minimal tissue stimulation [14]. It seems that bioceramic sealers produce fewer artifacts than gutta-percha [15]. In this situation, the possibility of VRF detection could increase, and therefore, flap and exploratory surgery would not be needed. The purpose of this study was to evaluate the performance of a bioceramic-based root filling material in the detection of Vertical Root Fractures (VRF) in CBCT imaging.
2. MATERIALS AND METHODS
2.1. Sample Collection
In this in vitro study, 100 human mandibular premolar teeth extracted in Hamadan clinics due to periodontal diseases or other dental problems were collected. Reported experiments were in accordance with the ethical standards of the committee responsible for human experimentation and with the Helsinki Declaration of 1975, as revised in 2013. Single rooted teeth and those with uniformly straight roots were included in the study. Before teeth extraction, a consent form was signed by patients in the surgery department. Teeth with any root fracture and resorption, as well as those previously treated endodontically, were excluded. This study was approved by the Ethics Committee of Hamadan University of Medical Sciences by ethical code IR.UMSHA.REC.1397.700.
2.2. Sample Preparation
The collected teeth were fixed in 0.5% sodium hypochlorite, and cavity access was prepared by a turbine (Nsk, Seoul, Korea) and diamond disk (Luster Dent, Zhengzhou, China). Rotary ProTaper NiTi files (Dentsply Maillefer, Ballaigues, Switzerland) were used to instrument the canals according to the manufacturer’s instructions. The prepared teeth were divided into two equal groups. In the first group, the teeth were root-filled with AH 26® (Dentsply DeTrey Gmbh, Konstanz, Germany) and gutta-percha (Meta, Chungcheongbuk, Korea). The teeth in the second group were root-filled with a bioceramic sealer (Sure Dent, Gyeonggi-do, Korea) and bioceramic coated gutta-percha (Sure Dent, Gyeonggi-do, Korea). Lateral condensation and single cone techniques were used to fill the roots with gutta-percha and bioceramic, respectively. After the filling process, the roots were stored at 37 °C in 100% humidity for 10 days to ensure all sealers had been set. After 10 days, the crowns were removed from the cementoenamel junction (CEJ) using a laboratory disk.
A total of 25 teeth in each group were selected randomly, mounted on an acrylic monomer, placed on a fixed platform, and finally, a 200N force at 1 mm/min was applied by the Universal Testing Machine (Iran, Tehran, Sentam) to induce VRF. When a 20% drop in force was recorded, the process was stopped. The VRF was examined by a surgical operating microscope (Zeiss Meditec AG) at 10x magnification (Fig. 1). The teeth with no fracture were again subjected to the pressure in the Universal Testing Machine. In some cases, the teeth were excluded, and alternative teeth were used to induce VRF. The other 25 teeth in each group were also considered as a control.
2.3. CBCT Imaging
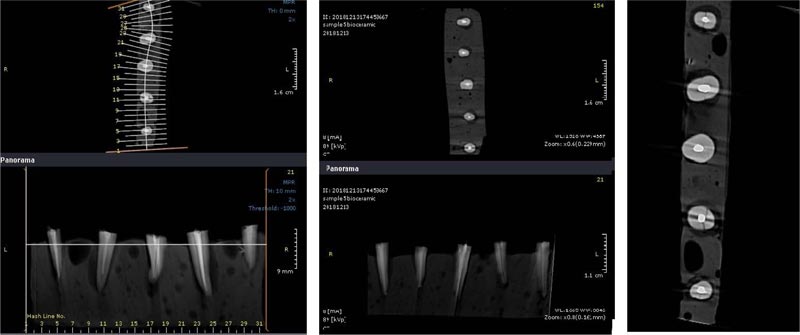
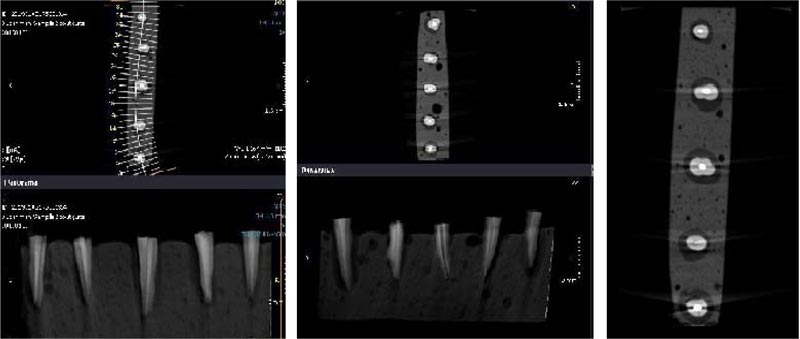
The apex of the prepared teeth was inserted into the wax, and then the teeth were placed in acrylic blocks (1 * 10 cm). A Cranex 3D CBCT device (Soredex, Tuusula, Finland) with 200 µm voxel size and 6 × 8 cm2 field of view (FOV) was used for scanning root fractures. Device settings were set to Kvp: 90, mA: 10, and time: 12 s. The images were then saved in DICOM format and evaluated using Ondemand 3D dental (Cybermed, Seoul, South Korea) software (Figs. 2 and 3). A 15-inch liquid crystal display monitor (Toshiba Satellite L40, Tokyo, Japan) with a 768 * 1367 pixel matrix was used for observation and interpretation of images in a dimly lit room with no time restriction. The images were assessed twice by an expert oral and maxillofacial radiologist and a dentist separately in two weeks. The two observers were allowed to adjust the brightness, contrast, and magnification of images to obtain the best visual results. All cross-sectional slices had 1-mm intervals and 0.5-mm thickness. Coronal, sagittal, and axial sections were used to detect VRF.
2.4. Statistical Analysis
Data from two observers were entered into Microsoft Excel 2016 (Microsoft ® Corporation) and analyzed by SPSS 21 (SPSS Inc, Chicago, IL) software to measure sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), accuracy, and area under the curve (AUC). Cronbach’s alpha was used to evaluate inter- and intraobserver agreements. Comparisons of the 2 systems were made using the Mann-Whitney test. P values ≤ 0.05 were considered as a statistical significance difference.
3. RESULTS
There was a strong agreement between the two observers. It showed 88% intraobserver agreement and 83% interobserver agreement. Sensitivity, specificity, accuracy, PPV, and NPV are reported in Table 1.
As the results showed, an increase in sensitivity (P = 0.017), specificity (P = 0.018), PPV (P = 0.018), NPV (P = .018), and accuracy (P = 0.011) was observed when the bioceramic sealers were used. These results indicated that the diagnostic value of VRF increases when bioceramic sealers are used instead of AH26 plus gutta-percha.
| p value | Gutta-percha Material | Bio ceramic Material | - |
|---|---|---|---|
| Mann-Whitney | |||
| 0.017 | 84±3.26 | 93±2.00 | Sensitivity (%) |
| 0.018 | 78±5.16 | 95±2.00 | Specificity (%) |
| 0.018 | 79±3.91 | 94.25±1.50 | PPV (%) |
| 0.018 | 82.75±2.21 | 92.75±1.50 | NPV (%) |
| 0.011 | 81±2.00 | 94±0.00 | Accuracy (%) |
| 0.011 | 81±2.00 | 94±0.00 | AUC (%) |
4. DISCUSSION
Due to its high accuracy and reliability, the use of CBCT in the diagnosis of dental lesions such as root fractures is nowadays expanding [7, 8]. However, it is highly affected by the presence of metal artifacts caused by dense endodontic materials such as gutta-percha [11]. Recently, the use of bioceramic sealers with a central core containing calcium silicate has been introduced in endodontics dentistry [16]. Bio-ceramics are biocompatible ceramic materials or metal oxides with enhanced sealing ability, antibacterial and antifungal activity and are used in medicine and dentistry. They have the ability to either function as human tissues or to resorb and encourage the regeneration of natural tissues. They include alumina and zirconia, bioactive glass, glass ceramics, calcium silicates, hydroxyapatite and resorbable calcium phosphates, and radiotherapy glasses [17, 18]. However, few studies have investigated the effect of these sealers in the diagnosis of dental lesions such as VRF.
The results of this study showed that gutta-percha reduces the accuracy of VRF detection in CBCT images. Consistent with our study, Fox et al. showed that gutta-percha reduces the quality of CBCT images even when BH artifact reduction algorithms are used [16]. The same results are found by Barbosa et al. when root canal fillers containing metallic compounds such as gold and gutta-percha were used [18]. Hekmatian et al. showed that gutta-percha reduced the accuracy of CBCT images and suggested removing root canal materials before CBCT imaging [19].
The main cause of reducing image quality in gutta-percha filled root canal is attributed to the Beam Hardening (BH) artifacts, which are difficult to remove even by artifact reduction algorithms (ARA). When an X-ray beam passes through an object, lower-energy photons are more preferably absorbed than higher-energy photons. This phenomenon is called beam hardening and occurs by high-dense materials in all CBCT devices [20, 21]. It seems that the nonlinear attenuation of X-rays is the main cause of beam hardening [22]. Therefore, the use of low, dense materials in endodontic dentistry has been suggested [23].
Based on the results of this study, the use of bioceramic sealer instead of gutta-percha significantly increased the diagnostic value of vertical root fracture in CBCT images. Celikten et al. study also showed that bioceramic sealers produce fewer artifacts in CBCT and microCT devices, so their use is recommended in endodontic dentistry [15]. A study by Fox et al. also showed that zirconium-based root filling material produces fewer Beam Hardening (BH) artifacts and increases the sensitivity of CBCT images when compared to the gutta-percha [16]. Bioceramic sealers have less radiopacity than other endodontic materials such as gutta-percha and metal posts which cause lower beam hardening and lower artifacts in CBCT images [24]. In the present study, the bioceramic sealer produced low artifacts in a way that accuracy, sensitivity, specificity, positive predictive value, and negative predictive value of CBCT images increased up to 95%. Therefore, it may not need to remove this root filling material to diagnose VRF accurately by CBCT in clinics.
It seems that changes in device parameters could affect the quality of CBCT images in root canal-filled teeth. As shown in a study by Gaêta-Araujo et al., when gutta-percha or metallic posts are used, reduction in the current (mA) can improve the quality of CBCT images to detect VRF [25]. Iikubo et al. have shown that smaller voxel size and placement of the target at the FOV center could reduce the artifacts created by gutta-percha [26]. Similar results were also shown in the studies of Brito-Junior et al. [27] and da Silveira et al. [28]. However, changes in these parameters are also not desirable for final image quality. Although these changes could improve the quality of CBCT images, the final output is not acceptable enough to detect root fractures. Therefore, there is a need for other endodontic materials with more desirable properties to produce fewer artifacts. Bioceramic sealers can be of this type of material.

In the present study, the Cranex 3D CBCT device was set to 200 μm voxel size, 90 kvp voltages, and 5 mA current. The recommended voxel size in most diagnostic protocols is 200 μm. Similar to our study, da Silveira et al. obtained high sensitivity and specificity with 200 μm voxel size. This study showed that the quality of CBCT images decreases at higher pixel sizes [28]. Brady et al. suggested the smaller voxel size to detect root fractures. However, incomplete root fractures with a length of 50 μm were evaluated in this study [29]. In a study by Fox et al., CBCT images were recorded at 75 μm voxel size, 70 kvp, and 3.2 mA [16]. This study recorded a low sensitivity in the detection of VRF in the presence of zirconium and gutta-percha (58.3% and 46.59%, respectively). However, in our study, the sensitivity was 84% for gutta-percha and 93% for bioceramic sealer, which was significantly higher. The differences could be due to the use of different voxel sizes, which were lower in the Fox et al. study [16]. Although reducing the voxel size seems to improve the image quality, it is more likely to create noises. Therefore, the minimum voxel size is not always recommended. In addition, shorter width fractures in Fox et al. study makes VRF detection more difficult.
In addition to current, the voxel size, the Field of View (FOV), and voltage could affect the diagnostic value of the CBCT images, and the adjustment of these three factors determine the best outcome [30-33]. The type of CBCT machine also influences the quality of the images. It is shown that the quality of images increases by a decrease in voxel size, although it may be associated with increased noise. Some studies have shown that voxel size decreases with increased image quality, while others have reported a decrease in voxel size with increased noise [27]. Finally, most studies on CBCT images in the diagnosis of VRF are experimental, which is different from in vivo conditions.
In the present study, CBCT was used to scan root fractures because of its high sensitivity and specificity. A study by da Silveira et al. showed that radiography, similar to CBCT, has high sensitivity and specificity in the diagnosis of VRF in non-root canal-filled teeth. However, this study showed that the use of endodontic materials significantly reduced the quality of radiographic images. This decrease in image quality was also observed to a lesser extent in CBCT [28]. Similar results were also observed in a study by Junqueira et al. [34]. As a result, the use of endodontic materials that produce fewer artifacts is important not only in CBCT but also in radiographic imaging systems which are commonly used to diagnose endodontic lesions.
Some advantages of bioceramic sealers include brilliant biocompatibility properties due to their similarity with biological hydroxyapatite, as well as intrinsic osteoinductive capacity because of their ability to absorb osteoinductive substances if there is a bone healing process nearby. They also have the ability to achieve a perfect hermetic seal, form a chemical bond with the tooth structure, and have good radiopacity. These also possess antibacterial properties as a result of precipitation in situ after setting, a phenomenon that leads to bacterial sequestration [35, 37].
CONCLUSION
The use of high opacity endodontic materials such as gutta-percha increases the artifacts in CBCT, thereby reducing the diagnostic value of the images. The reduced beam hardening of the bioceramic root filling materials improves the sensitivity of VRFs detection, and it seems that when it is used, there is no need for invasive techniques to diagnose root fractures.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Ethics Committee of Hamadan University of Medical Sciences, Iran with ethical code IR.UMSHA.REC.1397.700.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from all participants.
AVAILABILITY OF DATA AND MATERIAL
The data supporting the findings of the article is available from corresponding author [A.S] upon reasonable request.
FUNDING
The Vice-Chancellor of Research and Technology of Hamadan University of Medical Sciences provided funding for this study (Grant No. 9802241624).
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


