Evaluation of the Relationship between Trait and State Anxiety and Temporomandibular Dysfunction
Abstract
Background:
Anxiety is an important factor in the process of chronic pain in patients with Temporomandibular Dysfunction (TMD).
Objective:
The objective of this study was to evaluate the influence of minimally invasive management of muscular TMD on the levels of anxiety (state and trait), pain, and other parameters in patients with muscular TMD.
Methods:
A total of 83 patients (64 women and 19 men; mean age, 25.16 ± 4.40 years) who were clinically diagnosed with TMD were evaluated. During the first clinical session (T1) and after clinical evaluation and diagnosis, the participants filled out a pain visual analog scale and answered the Trait Anxiety Inventory (STAI-T) and State Anxiety Inventory (STAI-S). In addition, the bite strength of the participants was evaluated, and minimally invasive management (thermotherapy, orientation exercises, and cognitive behavioral therapy) was initiated in that session. After 8 weeks (T2), all parameters were reevaluated. The results obtained were statistically analyzed and found to have a significance level of 5%.
Results:
A significant decrease in pain, STAI-T, and STAI-S scales were observed from T1 to T2 (p < 0.0001). Higher values of bite strength were observed at T2 compared to T1 (p < 0.0001). Furthermore, a significant correlation was observed between the levels of pain, trait-anxiety, and state-anxiety.
Conclusion:
Minimally invasive management of TMD resulted in a reduction in the levels of pain and anxiety (trait and state) of the participants evaluated, suggesting a possible association of these factors with chronic myofascial pain.
1. INTRODUCTION
Temporomandibular Dysfunction (TMD) is a public health problem in the adult population, with prevalence ranging between 3.7% and 12% [1-4]. The majority of this population is composed of women of childbearing age, and this predominance is related to biological, hormonal, psychological, and social factors [2, 5, 6]. Among the different types of temporomandibular dysfunction, myofascial pain is a subtype characterized by myalgia with pain that spreads all over the temporomandibular region upon palpation [1]. According to Su et al. [6], the relationship between psychological factors and TMD is multidirectional. The mental state may be related to the cause, continuation, or exacerbation of the TMD, which demonstrates the need to understand the physical and psychological characteristics of patients with this condition [6, 7].
Research on the evolutionary models of long-term pain processes suggests that psychological factors are the major agents of the chronicity of TMD. Within this context, pain, anxiety, depression, and the ability to cope with pain and stress have been identified as factors that are involved in the development and progression of TMD [8]. Additionally, there is evidence that some patients with myofascial pain are more anxious and/or depressed than asymptomatic individuals [7, 9, 10]. Pain and anxiety are closely related. Pain can lead to anxiety, and anxiety, in turn, can increase pain. Thus, in situations of increased anxiety, the pain threshold is decreased, which suggests that anxiety is a possible risk factor for TMD [11, 12].
Personality states can be regarded as transient cross-sections of a person's life, such as a person's anxiety at any given time (the state of anxiety) or emotional reactions that express the individual's personality (such as anxiety trait). Accordingly, trait anxiety refers to the relatively stable individual differences in the propensity for anxiety, that is, the differences between people and their tendency to regard stressful situations as dangerous or threatening and to react to such situations with increased intensity of anxiety state reactions [4].
Thus, although anxiety and pain are factors associated with TMDs, few studies have evaluated parameters related to anxiety in patients with myofascial pain at different times throughout treatment. Therefore, the objective of this study was to evaluate the influence of minimally invasive management of muscular TMD on anxiety levels (state and trait), pain, and other clinical parameters in patients with muscular TMD multiple times throughout treatment.
2. MATERIALS AND METHODS
2.1. Characteristics of the Participants Evaluated
The study was approved by the Ethics Committee of Faculdade São Leopoldo Mandic (#CAAE: 57079 616.2.0000.5374) and was conducted in accordance with the World Medical Association (Declaration of Helsinki). All participants signed an informed consent form prior to participation in this research. The study started in September 2016, and clinical follow-up of patients was carried out until March 2019.
The sample was composed of 83 patients with myofascial pain (both sexes and above 18 years) who attended the TMD/Orofacial Pain clinic at the Uninovafapi University Center (Teresina, Brazil). A total of 64 female and 19 male patients, with a mean age of 25.16 ± 4.40 years years, were examined (Table 1). The participants answered specific questions and underwent a clinical evaluation by a professional with clinical experience in the area, and then, they were confirmed to have a diagnosis of myofascial pain [1].
2.2. Data Collection
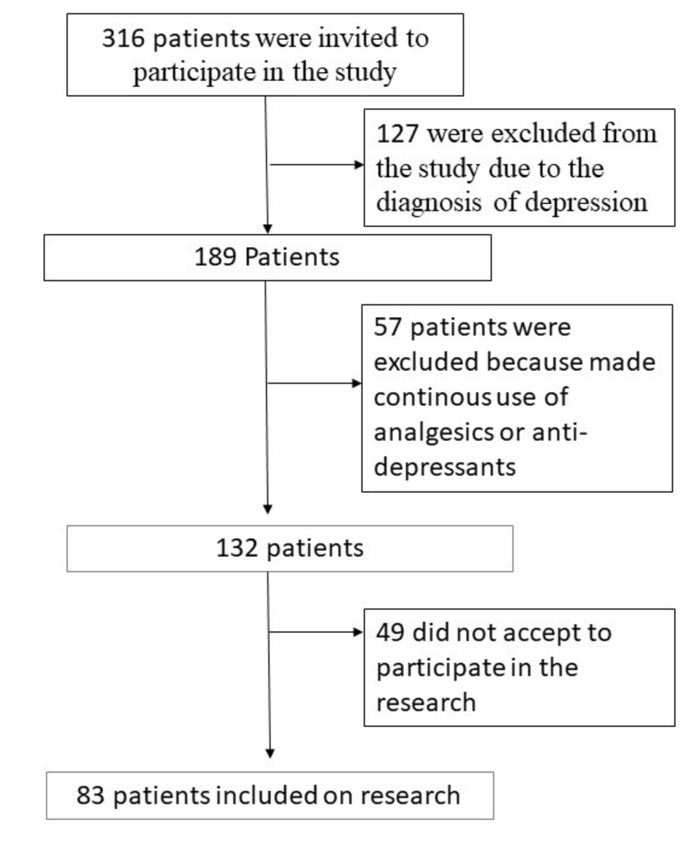
A total of 316 patients who attended the first consultation at the Integrated Health Center of the Uninovafapi University Center (CIS) were invited to participate in the study. However, only 83 patients met the inclusion criteria and agreed to participate in the study. The initial study time (T1) was considered to be the moment after the patient completed the consent form and agreed to participate in the study during the first visit. The patients were then asked to fill a Hospital Anxiety and Depression Scale (HADS) questionnaire to evaluate the presence of anxiety and possible depression [13].
| - | - | Total | % |
| Sex | Female | 64 | 77.1 |
| Male | 19 | 22.9 |
This stage of the evaluation was carried out to identify patients with possible depression. Patients with high values were referred for psychiatric evaluation (with a specialist). In this context, 127 patients were excluded from the study due to a diagnosis of depression (Fig. 1). Additionally, patients who used tranquilizers, analgesics (including non-steroidal anti-inflammatory drugs [NSAIDs]), or antidepressants or presented with some level of depression (in accordance with the questionnaire and clinical evaluation) were excluded from the study.
The patients were then asked to fill out two questionnaires of the State-Trait Anxiety Inventory (STAI) to assess their levels of trait-state anxiety [11]. They were also examined based on the pain visual analog scale (VAS) scores. After completion of all the questionnaires as well as assessment of bite strength, minimally invasive management of each participant was initiated with the following procedures: dry needling at all myofascial trigger points in the masseter and temporal muscles using a 20× acupuncture needle 13 (Quinzou, China), surface thermotherapy with a thermal mask for 20 min (Thermomaxx, Brasília, Brazil) (Fig. 1), transcutaneous electrical stimulation (TENS) using the dual FESVIF 995 device (Quark Medical, Piracicaba, Brazil), therapeutic exercise guidance, and cognitive behavioral therapy. Patients returned weekly to continue their minimally invasive management treatments for a total of 8 weeks. On completion of the study, patients were again asked to fill questionnaires and underwent evaluations, and the responses were compared to those of the initial questionnaires.
Therefore, for the purpose of analysis, the time corresponding to 8 weeks after the commencement of the minimally invasive management was considered time 2 (T2). Patients with TMD undergoing minimally invasive management usually show improvement after 6 weeks of treatment, which is why the evaluation period (T2) for this study was 2 months [14, 15].
2.3. State-Trait Anxiety Inventory
The STAI comprises two distinct self-reported scales to measure two distinct concepts of anxiety: state anxiety (S-A) and trait anxiety (T-A). Although originally developed as a research tool for investigating anxiety phenomena in adults, the STAI has also been found to be useful for measuring anxiety in 1st and 2nd-grade students and other volunteer profiles [16].
The STAI trait anxiety scale consists of 20 statements that require subjects to describe how they generally feel. The anxiety state scale also consists of 20 statements, but instructions require individuals to indicate how they feel at any given time. For each statement, the subjects must tick one of the four alternatives, indicating how they feel: absolutely not, a little, enough, and very much (on the S-A scale); and almost never, sometimes, often, almost always (on the T-A scale). For example, I feel tired - 1. almost never; 2. sometimes; 3. often; and 4. almost always.
The S-A scale is a sensitive indicator of the level of transient anxiety experienced by patients and can also be used to measure changes in the intensity of S-A, which occurs in these situations. The essential qualities evaluated by the S-A scale involve feelings of tension, nervousness, preoccupation, and apprehension [8].
2.4. Data Analysis
The numerical variables (VAS, STAI, and bite strength) were first submitted to the Shapiro-Wilk test for normality and Bartlett's test to observe homoscedasticity of their variances. As there was no normal distribution, all numerical variables were compared using the Wilcoxon test.
The Spearman correlation test (rS) was used to assess correlations between the VAS, STAI, and bite strength. All tests had a significance level of 5% and were carried out using statistical packages (BioEstat 5.0, GraphPad Prism 7.0).
3. RESULTS
The majority of the sample consisted of women (Chi-square test, p < 0.0001) with a diagnosis of myalgia. (Fig. 2) shows the VAS scores before and after treatment. There was a highly significant decrease (p < 0.0001) in the values (median [interquartile range]) of the VAS between those measured initially (7 [6-8]) and after the treatment (0 [0-0]). Figs. (3 and 4) also show that there was a significant reduction in the STAI-trait and STAI-state, respectively.
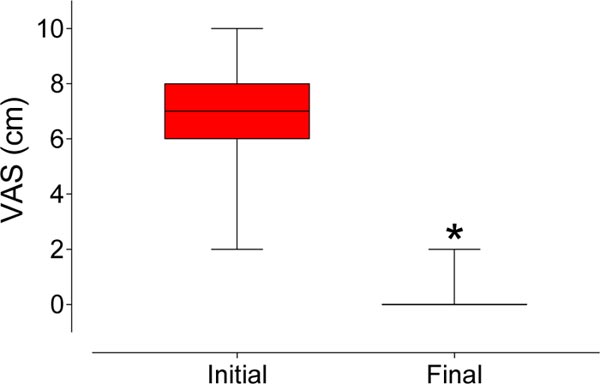
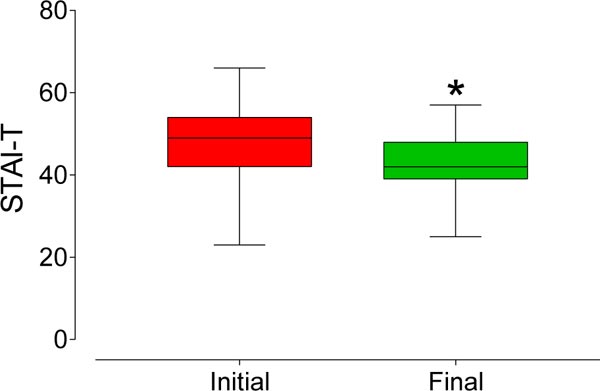
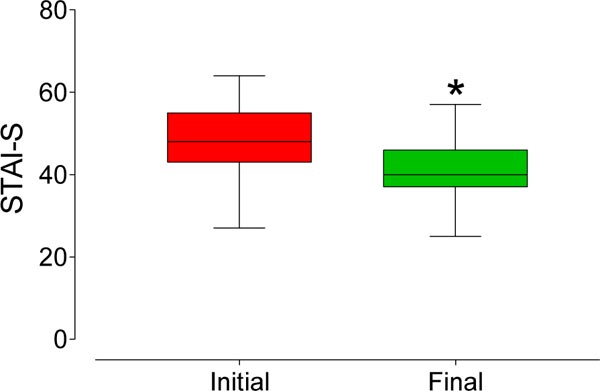
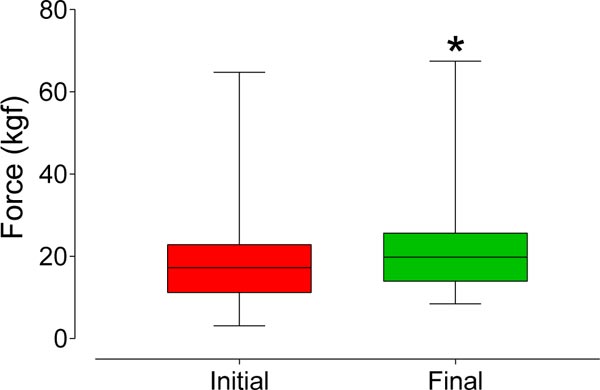
The values (interquartile range) observed for the STAI-trait were significantly reduced (p < 0.0001) from 49 [42-54] to 42 [39-48] after treatment. Additionally, the reduction observed in the STAI-state (median ± interquartile range) was significant (p < 0.0001), from 48 [43-55] to 40 [37-46] after treatment. The bite strength (median [interquartile range]) increased significantly (p < 0.0001) from 17.2 [11.2-22.9] kgf to 19.8 [13.9-25.7] kgf after treatment, as shown in Fig. (5).
A moderate and significant correlation was observed between the initial VAS values with both the STAI-trait (rS = 0.53, p < 0.0001) and the STAI-state (rS = 0.50, p < 0.0001). However, there was no correlation (p > 0.05) between any of these and the bite force.
Interestingly, after treatment, no correlation (p > 0.05) was observed between the VAS score and any of the other measures as well as among these measures themselves. These data may indicate that there is a close connection between the VAS and STAI in pain states such as myalgia.
4. DISCUSSION
Pain is a complex sensory and emotional experience that varies widely between people, depending on the context and meaning of the person's pain and psychological state. Cognitive and emotional factors have a surprisingly important influence on pain perception, and these relationships are in the brain regions that control pain perception, attention, or expectation and emotional states [2, 17].
Published studies suggest that there is a close relationship between TMD and the psychological factors selected in this study, such as personality traits, stress, depression, anxiety, and catastrophic thoughts [18]. It is noteworthy that anxiety disorders, somatization, and catastrophe contribute to chronic TMD, especially in the form of myofascial pain. Thus, knowledge of the influence of psychological factors affecting TMD may allow for the identification of patients with an increased risk of painful, chronic TMD [7]. Although anxiety and pain are associated with TMD, there are, nevertheless, few studies that have evaluated parameters related to anxiety in patients with muscle TMD at various times of treatment, which led to this study.
The participants studied herein showed a higher prevalence of TMD in females (77%), compared to males (23%), which corroborates published data that indicate a significantly higher prevalence of TMD in women [19].
Among the minimally invasive management therapies available [14, 15], thermotherapy was used in this study, in addition to guidance exercises, guidance for detaching the teeth, and TENS, with therapy performed once per week. As previously mentioned, after the 8-week period, a statistically significant reduction in pain on the VAS and increased bite force were observed, confirming the findings of previous studies [14, 20]. Additionally, the results showed a significant increase (p < 0.0001) in bite force after the 8-week period of conservative TMD treatment, corroborating the findings of Goiato et al. (2017) [20], who reported that increased bite force could be perceived when there is a reduction in pain originating from the masticatory muscles.
When comparing the levels of anxiety-state and the conservative treatment of TMD, a statistically significant reduction in the level of anxiety-state was observed after treatment in T2 (p < 0.0001), in addition to a moderate and significant correlation between the initial VAS values and state anxiety. Few studies with similar methodology have been performed, and some studies show a relationship between increased levels of anxiety when there is an increase in the intensity of pain in a patient with chronic pain [21].
Additionally, these studies report a significant relationship between the presence of anxiety in patients with chronic pain and with TMD itself [3, 8, 11, 21-23]. The high level of state- anxiety in patients with chronic pain can be related to the clinical conditions of the patient since state anxiety, as described by Spielberger (1983) [24] is characterized by subjective feelings of tension, anxiety, nervousness, and concern by the activation or awakening of the autonomous nervous system.
With regard to levels of trait anxiety and the minimally invasive management of TMD, a statistically significant reduction in the level of trait-anxiety was observed after treatment (T2), showing a moderate and significant correlation between the initial VAS values and trait-anxiety. Some studies suggest a relationship between anxiety and TMD [11, 25], but the variation in the level of trait-anxiety observed in this study was unexpected because the personality traits described by Spielberger (1983) [24] are relatively stable differences between people, with respect to specific trends to understand the world in some way and the inclination to react or behave in a specific way with predictable regularity. However, Leal et al. (2017) [26] evaluated the correlation between trait and state anxiety in healthy volunteers exposed to different anxiogenic situations, and they concluded that trait-anxiety correlates positively with state anxiety in interpersonal threat situations. Within this context, the significant clinical improvement observed in the parameters evaluated in the study may have contributed to the improvement of trait anxiety, even though this parameter is related to behavioral characteristics [27].
Thus, the cognitive model of anxiety describes fear as an automatic evaluation of stimuli as imminent or dangerous threats. In contrast, anxiety is described as a lasting subjective response to experienced fear. The mode of orientation is preconscious and automatic, identifying stimuli as negative, positive, or neutral, comparing stimuli to those known in memory, and then redirecting attention based on personal relevance [27]. Thus, the findings of this study indicate that minimally invasive management may influence anxiety levels in patients with TMD, which is in agreement with the findings of Reissman et al. (2014) [11], who observed a trend of predisposition towards anxiety in patients with TMD.
This study has some limitations. One of the exclusion criteria (use of medication such as NSAIDs) was based on the patients' responses, with the risk of memory or omission in the response. A recent study [28] concluded that mental health is an important predictor of painkiller and sedative misuse, while pain can play a role in painkiller misuse. The authors also suggest that increased pain may be more critical than mental health in increasing the overuse of painkillers, which could interfere with the results of the present study.
However, considering the clinical improvement of patients with reduced pain perception and increased bite force, the results obtained in the present study suggest an improvement in pain levels and levels of trait anxiety and state anxiety in patients with muscle TMD undergoing minimally invasive management. This indicates a possible relationship between levels of pain and trait anxiety and state anxiety with myofascial pain.
CONCLUSION
The clinical improvement offered by minimally invasive treatment of myofascial pain can reduce the levels of state and trait anxiety, suggesting a possible association of these factors with chronic myofascial pain.
AUTHORS' CONTRIBUTIONS
Conceptualization: Livio Portela de Deus Lages, Rogério Heládio Lopes Motta. Data curation: Tiago Lima Monte. Formal analysis: Cristiane de Cássia Bergamaschi. Investigation: Livio Portela de Deus Lages.
Methodology: Livio Portela de Deus Lages, Antonio Sérgio Guimarães, Juliana Cama Ramacciato. Project administration: Rogério Heládio Lopes Motta. Resources: Livio Portela de Deus Lages, Rogério Heládio Lopes Motta. Supervision: Antonio Sérgio Guimarães
Validation: Livio Portela de Deus Lages, Tiago Lima Monte, Cristiane de Cássia Bergamaschi, Rogério Heládio Lopes Motta. Writing - original draft: Livio Portela de Deus Lages.Writing - review & editing: Cristiane de Cássia Bergamaschi, Juliana Cama Ramacciato, Rogério Heládio Lopes Motta.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Ethics Committee of Faculdade São Leopoldo Mandic, Brazil(#CAAE:57079616.2.0000.5374).
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures were followed in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
All participants signed an informed consent form prior to participation in this research.
AVAILABILITY OF DATA AND MATERIALS
The datasets generated during and/or analyzed during the current study are available from the corresponding author [R.H.L.M.] on reasonable request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


