All published articles of this journal are available on ScienceDirect.
Long-term Stability of Soft Tissue Esthetic Outcomes Following Conventional Single Implant Treatment in the Anterior Maxilla: 10-12 Year Results
Abstract
Purpose:
The present study aimed to evaluate the long-term stability of esthetic outcomes of soft tissue around maxillary anterior single-tooth implants after 10-to-12 years of loading.
Methods:
Patients who had been treated for single-tooth implants in the anterior maxilla between February 2000 and July 2002 were invited to participate in the study. All implants had been placed according to delayed implant placement and conventional loading protocols without any connective tissue graft or papilla preservation flaps. Pink Esthetic Score (PES) was rated using standardized clinical photographs to assess the esthetic outcomes of the implant treatment at the time of crown placement and at time of follow-up examination which was at least 10 years after the crown placement.
Results:
A total of 19 patients were included. The mean score of PES was 11.63 (SD 1.61; range 7-14) at baseline. After 10-to-12 years of function, a mean PES score of 11.05 (SD 2.09; range 6–14) was recorded. No significant differences were found in the esthetic outcomes, categorized based on clinically relevant levels, between the baseline and follow-up session (p>0.05).
Conclusion:
Within limitation of the present study, it can be concluded that the esthetic outcomes of soft tissue around the maxillary anterior single-tooth implants placed using conventional implant placement technique remained stable in the long-term.
INTRODUCTION
Single-tooth replacement in the anterior maxilla using implant-supported fixed prosthesis is a widely accepted treatment modality. Several studies have evaluated the success of implants placed in the esthetic zone based on the classical survival and success criteria and reported favorable outcomes [1, 2]. The classical success criteria of dental implants are mainly focused on osseointegration and radiographic bone loss. However, these classical criteria might not be sufficient when evaluating the success of implants placed in esthetically demanding areas, where adequate esthetic appearanceis considered to beof paramount importance for the overall treatment success.
One of the early attempts to address outcome assessment from an esthetic point of view was made in 1997 by Jemt who proposed Papilla Index, which simply assesses the size of interproximal papilla [3]. Although the size of interproximal papilla is a crucial factor in the overall esthetic assessment, several other parameters such as, but not limited to, color, form, and level of peri-implant soft tissue are responsible for an acceptable esthetic appearance. Therefore, since then, several attempts have been made to develop objective rating instruments in order to comprehensively assess the esthetic outcome of implant therapy in the anterior maxilla [4-8]. Pink esthetic score (PES), developed by Furhauser et al., is one of these instruments that has been widely used in the dental literature to assess the esthetic outcomes of implant therapy, and it has been shown to be a reproducible instrument to assess the esthetic outcomes of soft tissue around implant-supported restorations [6].
Several studies using objective esthetic scoring have shown that conventional implant placement in healed sites of the anterior maxilla yields acceptable esthetic outcomes [9-13]. Raes and colleagues compared the esthetic outcomes of single implants placed in the anterior maxilla based on the conventional implant placement protocol with that of implants inserted according to immediate implant placement protocol, and they found that PES was comparable in both implant placement techniques one year after implant placement (10.35 vs. 10.33, respectively) [12] Furthermore, Cosyn and colleagues in a cross-sectional study evaluated the esthetic outcome of single implant treatment in the anterior maxilla using conventional and early implant placement techniques, and they reported that both techniques result in comparable esthetic outcome (PES: 10.40 vs. 9.90, respectively) [14]. Although these studies showed that conventional, immediate, and early implant placement techniques result in similar acceptable esthetic outcomes, there are still some concerns regarding the stability of the esthetic outcome of single implant placement in the anterior maxilla [15-17]. Lai and colleagues demonstrated that the esthetic outcome of maxillary anterior single implants placed by conventional implant placement technique improved significantly 6 months after loading compared with the time of crown delivery [18]. Furthermore, Pieri and colleagues in a 5-year prospective study reported that the mean pink esthetic score of single implants placed in the anterior maxilla remained stable over 5-year follow-up [17]. Although these short- and medium-term studies showed stable esthetic outcomes for single-tooth implant treatment in the anterior maxilla, long-term follow-up studies arestill necessary to evaluate the long-term stability of esthetic outcomes of maxillary anterior single-tooth implants placed by conventional implant placement techniqueto further consolidate the esthetic success of this treatment modality.
Therefore, the present study aimed to evaluate the long-term stability of esthetic outcomes of soft tissue around maxillary anterior single-tooth implants placed based on conventional implant placement technique after 10-to-12 years of prosthetic loading. The null hypothesis of this investigation was that no difference would be found in the mean pink esthetic score of maxillary anterior single-tooth implants placed using conventional implant placement technique between the baseline and after 10-to-12 years of loading.
MATERIALS AND METHODS
The present study included data on patients who had been treated for single-tooth implants in the anterior maxilla between February 2000 and July 2002 at Faculty of Dentistry, Tehran University of Medical Sciences, Tehran, Iran. Patients were invited to participate in the study on the basis of the following inclusion criteria: single implant treatment in the anterior maxilla (tooth number 6 to 11), presence of natural teeth adjacent to the implant site, delayed implant placement, no connective tissue graft or papilla preservation flaps at the implant site, conventional loading protocol, availability of baseline clinical photographs of the implant supported restoration, and a minimal follow up period of 10 years after implant loading.
The study was performed in accordance with the principles outlined in the Helsinki Declaration of 1975, revised in 2008 in Seoul, Korea on human experimentation. The study protocol was reviewed and approved by the Clinical Research Ethics Board at Tehran University of Medical Sciences. Informed consent was obtained from patients to use their data for research purposes.
A total of 19 patients (12 women and 7 men) with a mean age of 43.5 years (ranging from 19- 68 years) at the time of surgery were included in the present study. Two patients were smokers. All included patients were examined between January 2012 and December 2012.
All Patients had been treated by an experienced periodontist. The implant surgeries were planned based on clinical and radiographic examinations. Prior to the surgery, the gingival biotype of each patient had been recorded.
A single implant was placed for each patient at least 6 months following the tooth removal.Standard tissue level Straumann implants (Straumann AG, Waldenburg, Switzerlan) and Nobel Replace Select Tapered bone level implants (Nobel Biocare, Zurich, Switzerland) were used in the present study. In all surgeries, a crestal incision was made after achieving local anesthesia. After reflecting a standard mucoperosteal flap, the implant was placed according to standard implant systems’ surgical guidelines. All implants were inserted with an acceptable primary stability (30 to 40 Ncm insertion torque). Abutment connection was performed after at least three months of osseointegration using 35 N/cm torque, according to manufacturers’ recommendation. All implants resisted the applied torque. The classical prosthetic steps were conducted according to the standard procedure of the dental school for single crowns, and metal-ceramic restorations were prepared and cemented on all implants within 3-4 weeks.
Pink esthetic score [6] was used in the present study to assess the esthetic outcomes of the implant treatment. PES was calculated using standardized clinical photographs taken at the time of crown placement and at time of follow-up examination, at least 10 years after the crown placement. For implants placed in the position of central incisors, one photograph was taken centering at the midline that captured the implant and adjacent dentition. For implants placed in the position of lateral incisors or canines, two photographs of the implant crown and the contra-lateral tooth, the reference tooth, were taken.Baseline clinical images were digitized, and both baseline and final digital photographs were calibrated based on the clinical crown length of the implant-supported restoration that was measured clinically using a caliper.
The pink esthetic score (PES) is comprised of seven soft tissue parameters: shape of (a) mesial papilla and (b) distal papilla, (c) level of soft-tissue margin, (d) contour of soft-tissue, (e) alveolar process deficiency, (f) soft-tissue color, and (g) soft-tissue texture. Each parameter is scored using a 0- to 2-point scale, where 2 is considered as the best and 0 is considered as the poorest score, yielding a maximum possible score of 14. Interproximal papillae around the implant crown were assessed for completeness, and the five other variables were evaluated by comparison with the contra-lateral tooth which served as the reference tooth [6]. A score of ≥ 8 was considered as an esthetically acceptable outcome, and a score ≥ 12 was considered as an almost perfect outcome [19].
PES was recorded by an experienced examiner who was not involved in the treatment of the patients. The examiner had been calibrated prior to the study using photographs of 20 maxillary anterior single-tooth implants. Each evaluation was done two times by the same examiner with an interval of one month in order to ensure intra-examiner reliability. In the case of any inconsistent scores, a third evaluation was carried out on a different time with the participation of two other expert clinicians.
STATISTICAL ANALYSIS
The normal distribution of the data was tested with the Kolmogorov-Smirnov test. The changes in PES values between the baseline andfollow-up sessions were examined using the Wilcoxon signed ranks test. The same test was applied to compare interval-scaled PES values of baseline and follow-up sessions. Comparisons of PES valuesbetween the implant systems at the baseline and the follow-up sessions were performed using Mann-Whitney Test. A significance level of alpha = 0.05 was used for all comparisons.
RESULTS
The follow-up period was 120 to 154 months (mean 134.1;SD 10.04). Nineteen implant sites included 7 central incisors, 10 lateral incisors, and 2 canines. There were ten tissue level implants (Straumann) and nine bone level implants (Nobel). Guided bone regeneration was done for three implants at the time of implant placement. The gingival biotype of each site had been recorded prior to the implant placement, and a thick gingival biotype was observed at all sites (Table 1).
| Patient | Implant Site | Follow-up (mo) | Biotype | Implant type | GBR | PES baseline | PES follow up |
|---|---|---|---|---|---|---|---|
| 1 | 9 | 120 | Thick | Bone-level | Yes | 7 | 6 |
| 2 | 7 | 125 | Thick | Bone-level | Yes | 11 | 9 |
| 3 | 9 | 135 | Thick | Bone-level | Yes | 9 | 8 |
| 4 | 10 | 122 | Thick | Bone-level | No | 12 | 13 |
| 5 | 7 | 122 | Thick | Bone-level | No | 11 | 10 |
| 6 | 8 | 132 | Thick | Tissue-level | No | 13 | 13 |
| 7 | 11 | 125 | Thick | Bone-level | No | 12 | 13 |
| 8 | 6 | 125 | Thick | Bone-level | No | 12 | 11 |
| 9 | 10 | 141 | Thick | Tissue-level | No | 13 | 12 |
| 10 | 7 | 141 | Thick | Tissue-level | No | 12 | 12 |
| 11 | 10 | 141 | Thick | Tissue-level | No | 13 | 13 |
| 12 | 7 | 141 | Thick | Tissue-level | No | 13 | 14 |
| 13 | 10 | 144 | Thick | Tissue-level | No | 11 | 10 |
| 14 | 7 | 144 | Thick | Tissue-level | No | 11 | 9 |
| 15 | 8 | 154 | Thick | Tissue-level | No | 13 | 12 |
| 16 | 10 | 130 | Thick | Bone-level | No | 14 | 13 |
| 17 | 9 | 124 | Thick | Tissue-level | No | 12 | 10 |
| 18 | 9 | 147 | Thick | Tissue-level | No | 11 | 12 |
| 19 | 8 | 135 | Thick | Bone-level | No | 11 | 10 |
Pink esthetic scores at baseline and follow-up examinations are also presented in Table 1. The mean PES was 11.63 (SD 1.61; range 7-14) at baseline. After 10-to-12 years of function, evaluation of esthetic outcomes of the implant treatment showed a mean PES of 11.05 (SD 2.09; range 6-14).
A statistically significant difference was found in PES values between the two time points (p =0.027). An improved or stable PES was found in 7 sites (36.8%). The PES was slightly decreased in 12 sites compared to the baseline (63.2%) (Table 2).
| Number of sites | Percentage | |
|---|---|---|
| Improved | 4 | 21.05% |
| Stable | 3 | 15.79% |
| Worsened | 12 | 63.16% |
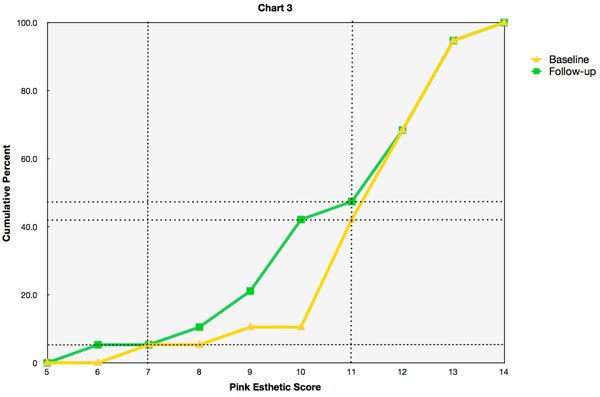
Overall PES values were categorized into the three clinically relevant levels: poor (0-7), acceptable (8-11), and almost perfect (12-14) esthetics outcomes (Table 3). Only one implant had a PES below the defined threshold of esthetically acceptable outcome at baseline. 36.8% and 57.9% of sites showed acceptable or almost perfect esthetic outcomes, respectively. After 10-to-12 years of function, pink esthetic scores of 12-14 were observed in more than half of sites (52.6%), and PES values of 8-11 were recorded 42.1% of sites. The Wilcoxon Signed Ranks Test showed that there is no significant difference in the esthetic outcomes between the baseline and follow-up sessions (p>0.05).
| Baseline | Follow-up | |||
|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | |
| Poor (0-7) | 1 | 5.3% | 1 | 5.3% |
| Acceptable (8-11) | 7 | 36.8% | 8 | 42.1% |
| Almost perfect (12-14) | 11 | 57.9% | 10 | 52.6% |
A further sub-analysis was done to test whether there are any differences between the two implant systems at each time point. Mann-Whitney Test showed that there were no significant differences in PES values between the two implant systems at baseline. Furthermore, no significant differences were found between the two implant systems at the follow-up session (p>0.05) (Table 4).
| Baseline | Follow-up | |||
|---|---|---|---|---|
| Tissue level | Bone level | Tissue level | Bone level | |
| Poor (0-7) | 0 | 1 | 0 | 1 |
| Acceptable (8-11) | 3 | 4 | 3 | 5 |
| Almost perfect (12-14) | 7 | 4 | 7 | 3 |
DISCUSSION
The present study was designed to evaluate the long-term stability of esthetic outcomes of soft tissue around single-tooth implants in the anterior maxilla after conventional implant placement. The results of this study demonstrated that although there was slight reduction in pink esthetic score for the majority of implants, clinically relevant esthetic outcomes of soft tissue around single-tooth implants remained stable over 10-to-12 years of function.
The present data showed that the overall esthetic outcomes of peri-implant mucosa were highly satisfactory at baseline with a mean pink esthetic score of 11.63. These esthetic outcomes can be considered remarkable since no connective tissue grafts or papilla preservation flaps were done at the implant sites. Comparable esthetic outcomes have been previously reported for single implants in the esthetic zone after conventional implant placement [12-14, 20]. On the other hand, some studies reported a lower mean of PES for conventional implant placement in the anterior maxilla compared to the present study [11, 18, 21, 22]. The higher pink esthetic scores in the present study could be attributable to the fact that all patient had thick tissue biotypes. This notion can be supported by studies reporting that the tissue biotype is the most importantdeterminant of the facial marginal mucosal level [23]. Furthermore, it has been reported that a thin gingival biotype is associated with incomplete distal papillae and advanced mid-facial recession [13, 24]. Another reason for high PES in the present study could be that most of the implants were placed in non-grafted bone (16/19). This argument can be supported by studies that showed pink esthetic scores were significantly higher when implant placed in the non-grafted bone compared to implant treatment in conjunction with guided bone regeneration or implant placement in the grafted bone [11, 13, 22, 25].
Stability of peri-implant soft tissue is of paramount importance within the anterior maxilla.The present data showed that pink esthetic score improved or remained stable only in 37% of the cases after 10-to-12 years follow up. However, considering the clinically relevant thresholds for poor, acceptable, and almost perfect esthetic outcomes, present results demonstrated that 18 out of 19 implants had acceptable or almost perfect esthetic outcomes after 10-to-12 years of loading, which is statistically similar to the baseline esthetic outcomes. Therefore, the present results indicate that clinically relevant esthetic outcomes of peri-implant soft tissue remained stable over 10-to-12 years of loading. These present finding is in line with that of Dierens and colleagues who found that soft tissue levels around single implants remained stable over a 16-22 year follow-up period [21]. The difference between the present study and Dierens’ study is that, in addition to implants placed in the maxillary esthetic zone, they included mandibular implants as well as implants placed in the first and second premolar positions which could be considered less challenging sites in terms of esthetic outcomes.
Although the long-term data onperi-implant soft tissue stability is limited, several studies have reported short and medium-term data on soft tissue alternations around dental implants [17, 18, 26, 27]. Small and Tarnow found that the majority of peri-implant soft tissue alterations occurred within the first three months [26]. Another short-term study by Lai and colleagues reported that esthetic outcomes of peri-implant soft tissue improved significantly six months after crown placement [18]. This improved esthetic outcome could be explained by the study of Priest who found that papilla levels tend to increase in height and sulcular levels tend to remain stable over the long-term [27].
The present results also demonstrated that there were no significant differences in esthetic outcomes of peri-implant soft tissue between the bone level and tissue level implants, and both implant systems had stable esthetic outcomes in the long-term. This finding is interesting because there were some concerns expressed regarding unfavorable soft tissue alteration around tissue level implants after completion of restorative therapy, [28] but the present data showed that esthetic outcomes of single tissue level implants in esthetic zone is similar to that of bone level implants. While this finding is promising, it should be interpreted with caution because the present sample size can be considered relatively small for additional analysis with subdivided groups. Therefore, future studies with larger sample size is recommended in order to compare the long-term esthetic outcomes of bone level and tissue level implant systems.
Pink esthetic score was used in the present study in order to evaluate the esthetic outcomes of soft tissue around single implants. This instrument has been widely used in the clinical studies and has been shown to be a suitable tool for reproducibly assessing peri-implant soft tissue [6]. However, it should be noted that this assessment tool has some limitations. One of the limitations is that all seven soft tissue parameters, which are scored in PES, are given the same weight; however, it is questionable whether these parameters are equality important from the perspective of soft tissue esthetics. Furthermore, the clinical relevance of small differences in pink esthetic score is questionable. In order to address this issue, thresholds for clinically relevant esthetic outcomes, which had been previously proposed [12, 14, 19], were employed in the present study. It is also important to mention that the parameters that are assessed in this professional esthetic assessment tool might not be of decisive importance for patients, and it has been shown that the pink esthetic score does not reflect patients' satisfaction with the esthetic outcomes [9]. Therefore, there is a need for further studies to develop a patient-center esthetic assessment tool.
Within the limitations of the present study, it can be concluded the esthetic outcomes of soft tissue around the maxillary anterior single-tooth implants placed using conventional implant placement technique remained stable after 10-to-12 years of loading. Furthermore, it was found that favorable esthetic outcomes can be achieved and maintained with both tissue level and bone level implant systems; however, randomized clinical trials with larger sample size are still needed to confirm this observation.
DISCLOSURE
This is an extended version of the poster published in “Long term prognosis of implants in esthetic zone”, Clinical Oral Implants Research, Volume 25, Issue s10 September 2014 Pages 357–359”.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
This study has been funded and supported by Tehran University of Medical Sciences (TUMS) the grant no. is 15724.


