All published articles of this journal are available on ScienceDirect.
Orthodontic Management with Traction and Asymmetric Extraction for Multiple Impacted Permanent Maxillary Teeth – A Case Report
Abstract
Multiple impacted teeth are a rare eruption disturbance that increases the case complexity. In this article, we described a 13-year-old boy whose 5 permanent maxillary teeth were not erupted although their root formation was complete. The orthodontic treatment with traction and asymmetric extraction was performed to achieve a significantly improved functional and esthetic result.
INTRODUCTION
Tooth impaction can be defined as the infra-osseous position of the tooth after expected time of eruption. It occurs as much as 25% to 50% of the population [1]. According to a review by Bishara [2], the primary etiological causes of tooth impaction include space deficiency, disturbances in tooth eruption sequence, retention of deciduous teeth, trauma, premature root closure, rotation of tooth buds, thickened overlying osseous or mucosal tissues, cysts and odontomas. Multiple impacted teeth might be related to genetic syndromes such as cleidocranial dysplasia (CCD) or endocrine disorders.
A single impacted tooth can increase the difficulty of orthodontic treatment significantly, and multiple impactions certainly complicate the treatment and lengthen the overall treatment time considerably. It needs coordinated management to guide eruption of as many teeth as possible [3]. In such a case, open communication between the orthodontist and oral surgeon is essential, as it will allow for the appropriate surgical and orthodontic techniques to be used.
This case report shows a patient with multiple impacted teeth in the maxilla. Combined treatments, including extraction, orthodontic traction were performed to achieve functional and esthetic result.
CASE PRESENTATION
Clinical Examinations
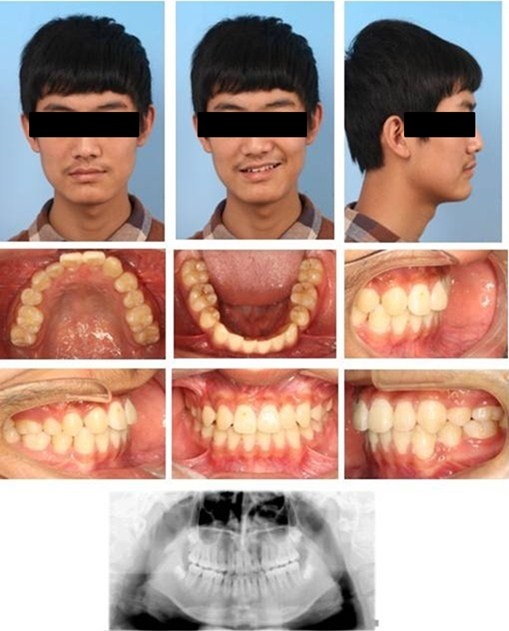
A 13-year-old boy was referred to our department for orthodontic consultation with respect to the failure eruption of some upper teeth. His facial profile was straight and no facial asymmetry was observed. The medical history was normal and traumatic history was not reported. There were no associated syndromes. No other family members were known to have the similar abnormalities. Intra-oral examination showed Class I molar relationships on both sides, associated with the remaining of maxillary deciduous canine and first molar on the right side and maxillary deciduous molars on the left side, missing maxillary central incisor and first premolar on the right side and canine and premolars on the left side, moderate crowding and a midline diastema. The oral soft tissues were unremarkable (Fig. 1).

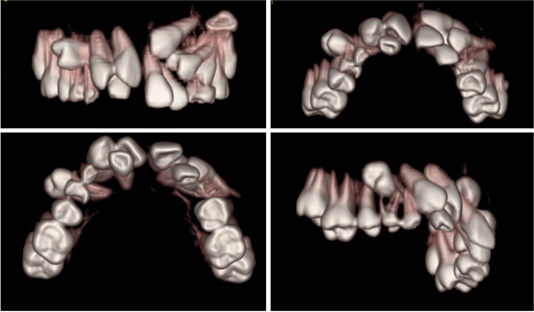
The panoramic radiography showed that no teeth missing congenitally and all permanent teeth were present. The maxillary left canine and bilateral first premolars had essentially full roots (closed apices) and were deeply impacted with a remarkable inclination. The maxillary left second premolar was impacted beneath the primary second molar. The right central incisor was impacted due to the space deficiency and can be touched in the labial mucosa of the lateral incisor. Although the maxillary right canine had erupted into the oral cavity, it was still submerged and classified as impacted. No obvious root resorption was found (Fig. 2).
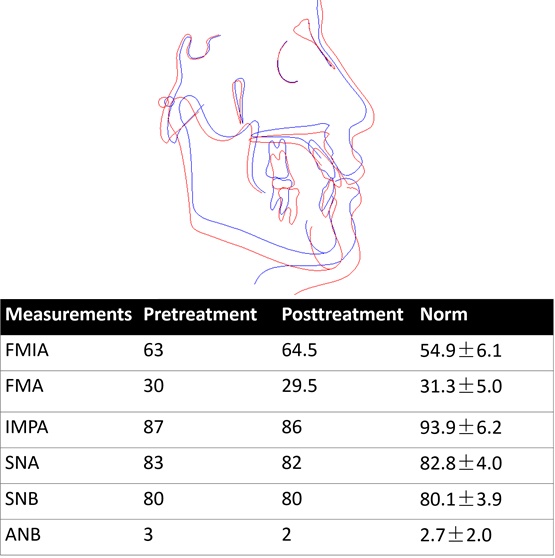
Analysis of the lateral cephalometric radiograph showed a Class I skeletal type (SNA=82°, SNB=80°, ANB=2°) with a reference to Chinese standards. The inclination of the maxillary and mandibular incisors was slightly bigger (U1-L1 angle= 129°). Other relative indexes in the cephalometric tracing were within normal range.
He denied ever having any temporomandibular joint (TMJ) dysfunction signs or symptoms, and maximal opening and lateral and anterior movements were within normal limits.
Treatment Objectives
The principal objectives were to create spaces for the impacted teeth to a functional, esthetic and stable occlusion, relieve the crowding, level and align the arches, obtain an ideal overjet and overbite, and achieve a bilateral Class I canine and molar relationship.
The treatment started with the extraction of retained deciduous teeth, then full fixed orthodontic therapy was proposed with surgical exposure and orthodontic traction of the impacted teeth. In order to relieve the crowding, the mandible first premolars and maxillary right lateral incisor and left first premolar were extracted.
Treatment Progress and Results
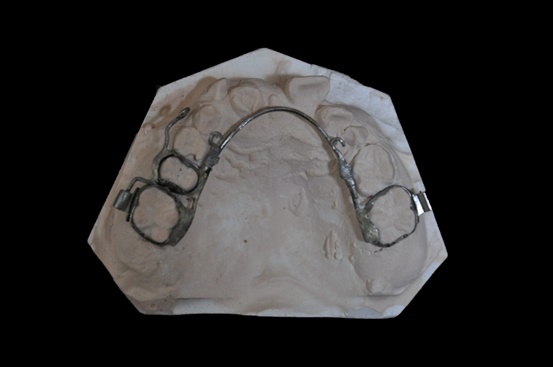
After extraction of the retained deciduous teeth, a specially designed labial and palatal arch appliance was made (Fig. 3). Three cantilevers were welded on the labial and palatal arch (0.039-in) separately, which integrated the upper first molars and right second premolar as a unit to strengthen the anchorage. This anchorage system facilitated the distal movement of the right canine and forced eruption of the impacted teeth. In light of dental crowding, we extracted four permanent teeth including upper right lateral incisor, left first premolar and lower first premolars. The surgical exposure was first carried out for the maxillary right first premolar. The button was bonded intraoperatively to crown as coronally as possible. Elastic chains were utilized between the bonded button and the cantilevers. The flaps were then sutured back to their original places. The chains passed transmucosally to facilitate closed eruption. Four months later, the maxillary right first premolars erupted into the oral cavity. Then 0.022Х0.028 inch slot straight-wire appliance was bonded to the available teeth and light continuous arch wires were placed for initial leveling (Fig. 4). At the same time, enough space was created for the impacted central incisor by the nitinol spring, the labial surface of the maxillary central incisor was surgically exposed. A bracket was then bonded to the incisor surface. Later, forced eruption of the impacted upper left canine was performed. During the canine traction procedure, a 0.017×0.025 inch continuous stainless steel archwire was placed in the lower arch with 3/16 inch vertical triangle elastics from the lower left canine to the upper left lateral incisor and canine for three months. The elastic was only to wear at night time. Six months after exposure and ligation, upper left canine was properly positioned (Fig. 5). All the teeth (include the second molars) were aligned with nickel-titanium archwires. Then 0.019×0.025 inch stainless steel archwires were placed for detailing. After removing the fixed appliance, the maxillary and mandibular teeth were stabilized with clear retainers. The retainers were maintained all day for 6 months, subsequently, were worn only during the night for another 1.5 year.

After orthodontic treatment, all treatment objectives were fully achieved including an ideal overjet and overbite with well-interdigitated class I molar relationship. There was no remarkable change of the patient profile. The gingival contour of the central incisor was acceptable. Upper right canine was reshaped to instead of the lateral incisor. Occlusal adjustment on the upper right first premolar was performed to prevent traumatic occlusion and achieve acceptable canine protected occlusion (Fig. 6).

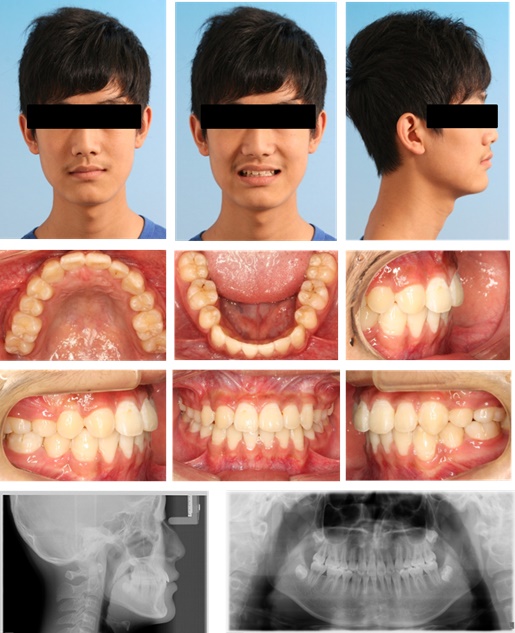
The posttreatment panoramic radiograph showed good root parallelism and no marked apical root resorption. Also, no marginal or vertical bone loss of the periodontal tissues was detected. Cephalometric analysis revealed a maintained Class I skeletal type (SNA=81°, SNB=80°, ANB=1°), which indicated normal growth pattern of the maxilla and mandible during orthodontic treatment (Fig. 7). After 10 months retention, this patient still had a stable occlusion (Fig. 8).
DISCUSSION
The impaction of multiple teeth occurs infrequently, the etiologic factors differ, including genetic syndrome, metabolic disorders and various local causes. Ishihara reported a 13-year-old boy showing nonsyndromic bilateral multiple impacted premolars with dentigerous cysts [4]. However, the arrested eruption of multiple teeth in the case presented here, reported no traumatic and medical history but retained primary teeth. So, the exact etiologic factor of this case is unclear and requires further investigation.
Management for the impaction of multiple permanent teeth is a challenge to the orthodontists. Before treatment, the impacted teeth require an early diagnosis and interception of potential impaction [5]. Factors that must be judged acceptable prior to the initiation of forced eruption are esthetics, clinical root length, root proximity, root morphology, individual tooth position, collective tooth position, and the ability to restore teeth [6]. For this case, the combination of conventional radiographic techniques including panoramic, and lateral cephalometric radiographs was used to evaluate the labiolingual position, root development and the adjacent structures. However, the two-dimensional radiographs can sometimes unjustifiably suggest a bad prognosis of an impacted tooth. Cone-beam CT scanning, which gives a three-dimensional image, can provide important additional diagnostic information. With cone-beam CT’s help, the exact positions of impacted teeth and the adjacent teeth’s root development can be seen directly. Orthodontists also can use CBCT to evaluate the relationship between the impacted teeth and the surrounding structures. Therefore, an optimal traction plan can be made. A combination of surgical exposure and orthodontic traction is optimum to deal with multiple impactions. Impacted teeth could be moved into occlusion through many mechanical techniques. For some partially impacted teeth, only orthodontic technique may be available and effective without surgery. Orthodontists have recommended that the first thing to do with impacted teeth is to create adequate space and then surgically expose the tooth to give orthodontists access so that they can apply mechanical force to erupt the tooth [7]. Surgical transplantation may be another choice, but it has a high risk of complication, such as pulp necrosis, root resorption, and ankylosis [8]. Based on these considerations, we chose surgical exposure combine with orthodontic traction. The maxillary right canine had erupted out of the mucosa. So the attachment was bonded directly. The maxillary right incisor was impacted due to the space deficiency and covered by thin and mobile oral mucosa. We exposed the crown surface by opening a really small semilunar window for button bonding. The upper right first premolar was labially impacted and situated deeply. Surgical exposure was carried out from the palatal side. The attachment was bonded in lingual surface and the flaps were then sutured back to their original places. The root of maxillary left canine had almost accomplished its development and was deeply impacted with a remarkable inclination. Closed exposure was chosen, too. Closed exposure is beneficial to the gingival level, alveolar crest height and periodontal parameters. After that, orthodontic treatment with a specially designed labial and palatal arch appliance with two auxiliary cantilevers was used. The upper first molars and right second premolar were used effectively as anchorage for extrusion of the impacted first premolars. Elastic chain was widely used in our treatment. It could provide light force. The force level produced by the elastic chain decayed quite quickly. This characteristic is of great importance in the extrusion procedure of impacted teeth. The intermittent force provided a more mild eruption progress and a more stable micro-environment for the impacted teeth. It decreased the possibility of root resorption to a certain extent. Vertical triangle elastics was used by 3/16-inch involving left canine and lateral incisor in the upper arch and left canine in the lower arch to facilitate the occlusal movement of the upper canine. With compliant and knowledgeable patients this system can be particularly effective because they know the amount of movement is directly proportional to the amount of time the elastic is worn [9].
Another important factor of a successful treatment outcome is the appearance of the gingival contour. It can be a perceived difference in the amount of attached gingiva, when compared with the contralateral tooth or a difference in the relative heights of the gingival margins [10]. The treatment teeth with open-eruption were usually recognizable by the presence of a rolled band of gingival tissue around their crown. Vermette [11] referred to this as “gingival scarring”, and reported its presence in 90 percent of their open-exposure cases. To the contrary, closed-eruption is capable of achieving a superior outcome regarding on the aesthetics and periodontal health [12]. In order to improve the eruption prognosis of the tooth as well as its periodontal health and esthetic, the surgeon should keep in mind certain details regarding surgical technique. This patient’s first premolars were treated with a closed-eruption surgical exposure technique and had good gingival contour. The central incisor also had a good gingival condition around, which was exposed by open-eruption. It might be attributed to the light force and a more stable tooth movement.
Furthermore, due to the dental crowding of this case, some teeth should be extracted to provide enough space for leveling. Considering the right lateral incisor with abnormal crown shape, placed lingually, overlapped with central incisor, we chose the asymmetric extraction mode by extracting right lateral incisor instead of first premolar. Therefore, the clinicians should pay attention to the situations when the canine replaces the lateral incisor and the first premolar takes the place of canine. The canine needs to be reshaped by stripping the cusp and marginal ridge according to the shape of lateral incisor. The cingulum of canine and lingual cusp of first premolar need to be grinded to prevent traumatic occlusion and achieve acceptable canine protected occlusion. The bracket placement of the canine and first premolar is equally important to properly transfer the built-in torque, tip and in/out.
CONCLUSION
To achieve optimum aesthetic and functional results, a multidisciplinary cooperation with comprehensive diagnosis and reasonable treatment plan should be performed for the effective management of multiple impacted teeth. In the meanwhile, periodontal health consideration should be taken into account to acquire desirable outcomes.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
We thank the patient who agreed to have his photos taken and Yucong Liu for help with the preparation of the data collection.


