All published articles of this journal are available on ScienceDirect.
Revascularization of an Immature Tooth with Apical Periodontitis Using Calcium Hydroxide: A 3-year Follow-up
Abstract
Root canal treatment of teeth presenting immature development is a great challenge for both the patient and the professional. The thinness of the root canal walls of immature teeth may lead to root fracture and thus the outcomes of such treatments are uncertain. Revascularization is based on root canal decontamination followed by the induction of blood migration from the periapical tissues and the development of new vascular tissue in the canal space. The principle of disinfection in regenerative endodontics is that it should be achieved with minimum root canal instrumentation; an intracanal medication is used to inhibit bacterial growth and appropriate sealing of the coronal portion is performed. The American Association of Endodontists (AAE) considerations for regenerative endodontics include calcium hydroxide as an alternative intracanal dressing. This material has also been claimed to diminish the possibility of dental staining during revascularization procedures. The relatively new treatment protocol has been widely reported in the last few years; however it should be performed only when other alternatives are not reasonable. This case report presents a 3-year follow-up of a case of revascularization of a maxillary central incisor using calcium hydroxide as a root canal disinfection dressing.
INTRODUCTION
Root canal treatment of teeth presenting immature development is a great challenge for both the patient and the professional. Use of appropriate technology can lead to successful cleaning and filling of a tooth with an open apex; however, the thinness of the root canal walls of immature teeth may lead to root fracture and thus the outcomes of such treatments are uncertain [1].
Revascularization of immature necrotic teeth aims to achieve the development of vital tissue in the root canal space, leading to lengthening of the root and thickening of the root canal walls. The growth of vascular tissue inside the root canal can be accomplished when proper disinfection is achieved. Revascularization is based on root canal decontamination followed by the induction of blood migration from the periapical tissues and the development of new vascular tissue [2].
The principle of disinfection in regenerative endodontics is that it should be achieved with minimum root canal instrumentation; an intracanal medication is used to inhibit bacterial growth and appropriate sealing of the coronal portion is performed. Different materials have been used as intracanal medications, such as triple antibiotic paste (TAP), double antibiotic paste (DAP), calcium hydroxide [Ca(OH)2], formocresol, and chlorhexidine [3-7].
Calcium hydroxide has been widely used as an intracanal medication in mature teeth because of its antibacterial properties. The high pH of Ca(OH)2 inhibits bacterial growth that may prevent the development of vital tissue [8]. The American Association of Endodontists (AAE) considerations for regenerative endodontics include calcium hydroxide as an alternative intracanal dressing [9]. This material has also been claimed to diminish the possibility of dental staining during revascularization procedures. On the other hand, remnants of calcium hydroxide might fill the space required for revascularization and create a hard tissue response instead of pulp-like growth [10].
The relatively new Ca(OH)2 treatment protocol has been widely reported in the last few years; however, it still presents a low evidence level and should be performed only when other alternatives are not reasonable [1, 11]. A successful case must present absence of radiolucency after six months, as well as development of both the length and width of the root canal walls [9]. A clinical exam should reveal an asymptomatic tooth and a positive response to a pulp sensitivity test. This case report presents a 3-year follow-up of a case of revascularization of a maxillary central incisor using calcium hydroxide as a root canal disinfection dressing.
MATERIALS AND METHOD
Case Report
A 6-year-old male patient was referred to an endodontist for evaluation and treatment of a maxillary right central incisor (tooth #8). The chief complaint of the patient was an uncomfortable sensation while biting. In spite of the situation, no medication was required at the time. The patient related a trauma to the front teeth four months ago. His medical history was reviewed and nothing relevant was found.
During clinical consultation, the tooth presented no color change when compared to the adjacent teeth. Periodontal probing was within the normal limits and no mobility was found. Swelling was present at the apical area of the tooth, which was symptomatic to percussion and palpation (Fig. 1). The tooth did not respond to cold and hot temperature testing, and electric pulp testing (EPT) also showed a negative response.
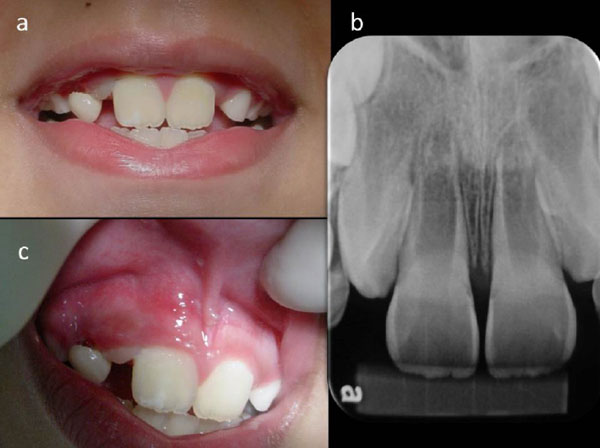
(a) Teeth presenting no sign of discoloration. (b) Baseline periapical radiograph of right maxillary incisor. (c) Swelling on apical area right maxillary incisor.
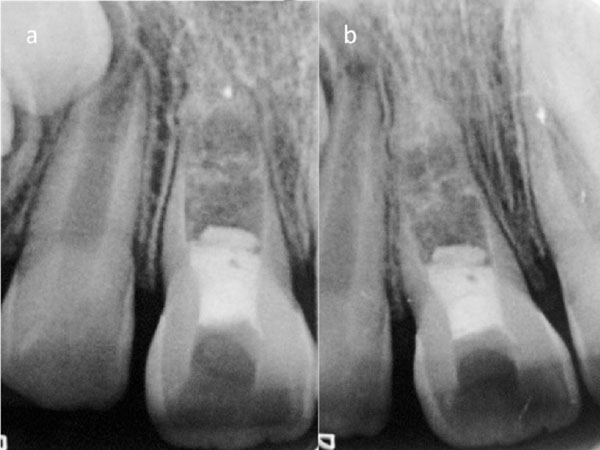
(a) Six-month follow-up periapical radiograph. (b) One-year follow-up periapical radiograph.

(a) Initial clinical aspect and (b) final clinical aspect.

Three-year follow-up periapical radiograph.
Periapical radiographs were taken and showed incomplete root formation, an open apex, and thin root canal walls in both teeth #8 and #9. A radiolucent area was observed in the apical third of the maxillary right incisor (Fig. 1). The initial diagnosis was symptomatic apical periodontitis.
Treatment options were discussed with the patient´s parents. Revascularization was chosen and an informed consent form was signed.
At the first visit, the tooth was anesthetized using 1.8 mL of 3% lidocaine 1:100,000 epinephrine and a rubber dam was placed for isolation. The pulp chamber was reached and copiously irrigated with 3% sodium hypochlorite (NaOCl). Working length (WL) was determined using an electronic apex locator (ROOT ZX; J Morita, Kyoto, Japan) and an x-ray was taken to confirm the position of the file. The root canal walls were carefully debrided with size 80 k-files (Dentsply-Maillefer, Ballaigues, Switzerland) and dried with the aid of paper points. A calcium hydroxide paste was obtained by mixing Ca(OH)2 (Fórmula & Ação, São Paulo, Brazil) with sterilized distilled water and a dressing was placed using a lentulo spiral root canal filler. The Ca(OH)2 dressing was placed so that it filled the root canal space up to the apical third. A double seal of Coltosol (Vigodent, Coltene, France) and Fuji IX (GC America, Alsip, USA) was used as a temporary restoration of the access cavity.
After 4 weeks, the patient returned for the second appointment. At this time, the patient was asymptomatic, and no pain was reported upon vertical percussion and palpation. The swelling had ceased and a periodontal probe remained within normal limits. The tooth was anesthetized using 1.8 mL 3% mepivacaine without a vasoconstrictor (Scandonest Plain; Septodont, Saint-Maur-des-Fossés, France). After rubber dam placement, the restoration was removed and the canal was irrigated with 3% NaOCl, allowing removal of the Ca(OH)2 dressing. A size 40 k-file with a bent tip was used to promote bleeding into the root canal space. After clot formation, a collagen matrix (Hemospon; Technew Ind. & Comercio, Rio de Janeiro, Brazil) and white mineral trioxide aggregate (MTA) (Angelus; Londrina, Paraná, Brazil) were placed 3 mm below the cement enamel junction (CEJ). Finally, the access cavity was closed with composite.
The tooth was clinically and radiographically followed up for 6 months (Fig. 2). All clinical conditions presented were normal. Radiographic evaluation showed slight lengthening of the root, no enlargement of the root canal walls, and an absence of radiolucency. A 3-year review showed an asymptomatic tooth and a slight color change at the crown (Fig. 3). A closed apex could be visualized and the root had lengthened to the same size as that of tooth #9. Thickening of the root was not notable and radiopaque tissue partially filled the root canal space (Fig. 4).
DISCUSSION
The concept of regenerative endodontics was pioneered by Nygaard-Ostby [12]. Recently, Banchs & Trope [2] reintroduced regenerative endodontics to modern endodontics, and the publication of many case reports and case series has followed [13].
This case reports a successful 3-year outcome of regenerative endodontic therapy of a maxillary central incisor presenting necrotic pulp and symptomatic apical periodontitis due to trauma. Different procedures were considered, but the benefits of revascularization outweighed the disadvantages. In spite of the still controversial scientific evidence for this treatment protocol [1], the choice of revascularization for this case was reasonable. Conventional root canal treatment of an immature tooth would have been technically challenging; long term apexification therapy using Ca(OH)2 or MTA apexification might have induced apex closing fully, but clearly do not allow root development. Besides, using Ca(OH)2 as a long-term dressing has the potential to increase the risk of root fracture [14].
The American Association of Endodontists considerations for regenerative endodontics states that absence of symptomatology and bone healing are the first aims of these procedures [9]. In fact, after disinfection and a 4-week medication period, the patient was asymptomatic and the swelling had ceased. Moreover, a 6-month follow-up showed bone formation in the periapical area. A positive response to the EPT is a sign that the tissue which has developed is a vital tissue. However, in the present case, the patient’s response to the EPT was negative. In a prospective analysis of 16 consecutive cases of revascularization, Kahler et al. [13] found only 5 positive responses to the EPT. Other authors have also reported negative results for the EPT after regenerative endodontic procedures [4, 15].
Canal wall thickening and increased root length are the secondary goal of regenerative endodontic procedure (AAE). The present case showed evidence of an increase in root wall length as well as apical closing. However, by comparing the preoperative and postoperative radiographs, it was not possible to confirm that the root walls had increased in thickness. A retrospective study has shown that when compared to triple antibiotic paste (TAP) and formocresol, calcium hydroxide is also able to promote further development of the pulp-dentin complex, with the TAP producing greater differences in root wall thickness. Nevertheless, Ca(OH)2, especially when placed beyond the coronal half, was not as efficient as TAP in promoting root wall thickening [5].
Ca(OH)2 has the advantage of being compatible with the survival of the stem cells of the apical papilla (SCAP), thus allowing their proliferation. A recent study showed that TAP, double antibiotic paste (DAP), and modified TAP in different concentrations reduced the survival of stem cells. On the other hand, Ca(OH)2, even in high concentrations, maintained the viability of stem cells [16]. However, in the current case, the radiographic images showed spots of radiopaque tissue inside the root canal, suggesting that non-pulp-like tissue had been formed.
One benefit of using Ca(OH)2 is that it diminishes the risk of tooth staining. In the case presented here, a minor change in color was noticed after the treatment had been completed. Calcium hydroxide was proven to be removed effectively from the root canal with minimum residual presence [17]. A collagen matrix was placed between the blood clot and the MTA, so it is unlikely that blood or Ca(OH)2 were responsible for the staining observed. On the other hand, MTA cannot be ruled out as a cause of the staining, as previous studies have demonstrated the potential for white MTA to stain teeth [18]. A different approach to MTA manipulation involving the addition of propylene glycol has been tested with good results regarding tooth staining [19]. Biodentine also has the potential to be an alternative to MTA with desirable properties [20]. Further studies should be considered in order to find the most appropriate material to avoid tooth discoloration after revascularization procedures.
CONCLUSION
This case reports a 3-year follow-up of a revascularization procedure using calcium hydroxide as the disinfection medicament. The treatment was successful in resolving symptomatology and promoting bone formation and root lengthening. Root thickening and tooth discoloration presented questionable findings.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


