All published articles of this journal are available on ScienceDirect.
A 12-Year Retrospective Survey of Management of Patients with Malignant Neoplasms in the Orbital Cavity in a Brazilian Cancer Hospital
Abstract
Purpose:
The aim of this study was to investigate the distribution of different types of malignant tumors in the orbital cavity, surgical treatments, and subsequent prosthetic rehabilitation.
Materials and Methods:
A retrospective sample of 269 charts of patients attending a public reference cancer hospital in Goiania, Goias, Brazil, between 1998 and 2009 was selected. Study variables included demographic data, clinical and histopathological features, and patient rehabilitation. Frequency analysis, chi-square test and multiple logistic regression were used for data analysis.
Results:
Patients’ age ranged from 1 to 92 years and 50.2% were female. The most prevalent tumors were basal cell carcinoma (58%), retinoblastoma (17.1%), squamous cell carcinoma of the conjunctiva (7.1%), malignant melanoma (6.7%), and rhabdomyosarcoma (4.5%). Surgical treatment was performed in 250 patients (92.3%), but only 29 patients (10.8%) received ocular prosthetic rehabilitation. Lower age (p<0.001) and enucleation surgery (p<0.001) were significantly associated with prosthetic rehabilitation.
Conclusions:
Results revealed high occurrence of mutilating interventions and low provision of prosthetic care, limited to younger patients who had undergone enucleation surgery. The high unmet demand for rehabilitation emphasizes the need to incorporate appropriate care for ocular and orbital deformities into the Brazilian public health system.
INTRODUCTION
A variety of tumors can affect the eye, ocular cavity, or the orbital region and the partial or complete resection of the eyeball or eyeballs is a common treatment approach, which results in great difficulties for post-surgical rehabilitation, aesthetical recovery, and social integration of the patient [1-4].
The three surgical procedures used for resecting these tumors are evisceration, enucleation, and exenteration depending on the nature of the tumor and the anatomical structures involved. Once the tumor has been removed, there is a need for aesthetic rehabilitation and a maxillofacial prosthesis is used to replace the natural eye with an artificial one [5, 6]. Radiotherapy and chemotherapy can also be used as adjuvant treatment, depending on the tumor clinical stage [7].
Studies show that basal cell carcinoma (BCC), retinoblastoma (RB), malignant melanoma, squamous cell carcinoma of the conjunctiva, and rhabdomyosarcoma are the most common tumors of the ocular region [8-11]. In general, surgical exenteration — i.e., the complete resection of the ocular globe and eyelid — is the procedure normally used for basal cell carcinoma and malignant melanoma in the orbital region [12]. Exenteration surgery is also required for squamous cell carcinomas of the conjunctiva [13-16] and rhabdomyosarcomas [17, 18].
Retinoblastoma is an intraocular tumor that occurs during childhood and usually shows aggressive behavior initially involving the eye and with subsequent extension to the skull and central nervous system via the optic nerve involving the ocular cavity. It requires early diagnosis and prompt treatment through enucleation of the eye affected by the tumor [19-21].
Surveying data about the distribution of orbital tumors and post-surgical rehabilitation is essential for planning appropriate care for cancer patients. Hence, the aim of this study was to investigate the prevalence of malignant tumors in the orbital region, describe its clinical and pathological features and the frequency of post-surgical rehabilitation of patients in a public Brazilian cancer hospital.
MATERIAL AND METHODS
This is a retrospective study of 330 records from the Araujo Jorge Hospital, maintained by the Cancer Combat Association of Goias (Goiania, Goias, Brazil) of patients who attended between 1998 and 2009. This hospital is a regional reference centre for cancer treatment in the public health care system.
The inclusion criteria were charts of patients with microscopic diagnosis of malignant lesions in the ocular cavity and indication for surgery in the Head and Neck Department of the hospital, regardless of gender or age. Sixty-one patients who attended other institutions were excluded and the final study sample was 269.
Data collected from the patients’ records included demographic variables (age, gender, and geographical origin of the patient) and clinical-pathological variables (clinical stage, anatomical site and histopathology of the tumor, patient's decision to have surgery or not, type of surgery, provision of psychological support, advice for and/or provision of prosthetic treatment, type of rehabilitation, and clinical outcomes).
The study protocol was approved by the local Research Ethical Committee.
Descriptive statistics, chi-square and Mann-Whitney tests, and multiple logistic regression analysis were used for data analysis, using SPSS 17.0 software.
RESULTS
From the 269 patients with orbital tumors and indication for orbital surgery for treatment of malignant neoplasms, 135 patients (50.2%) were female. The patients’ age at the first medical appointment ranged from 1 to 92 years and age distribution is shown in Fig. (1). Approximately half of the patients (n=139; 51.7%) originated from the State of Goias and the others were from other States of Brazil.
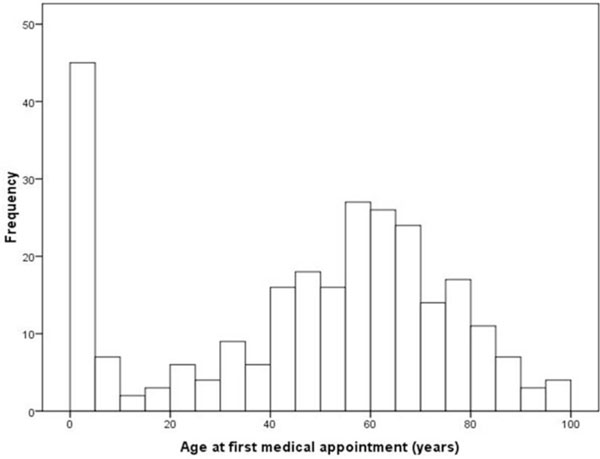
Age distribution of the patients.
Table 1 shows the frequency distribution of malignant lesions in descending order. The most common was basal cell carcinoma (58.0%), and another nine types of lesion presented frequencies ranging from 17.1% (retinoblastoma) to 0.4% (adenoid cystic carcinoma). The overall frequencies were separated by the type of surgery for which patients were submitted. Exenteration surgery was performed in 195 patients (72.5%), and in all patients with basal cell carcinoma. Enucleation was performed in 20.1%, mainly in patients with retinoblastoma (40 out of 46 patients). No surgery was observed in 19 patients (7.1%).
Frequency of Surgical Procedure According to the Type of Orbital Tumor
| Type of Tumor | Exenteration | Enucleation | Evisceration | No surgery | Total |
|---|---|---|---|---|---|
| Basal cell carcinoma | 156 | - | - | - | 156 |
| Retinoblastoma | 5 | 40 | - | 1 | 46 |
| Squamous cell carcinoma of the conjunctiva | 11 | 4 | - | 5 | 20 |
| Melanoma | 6 | 10 | - | 2 | 18 |
| Rhabdomyosarcoma | 8 | - | - | 4 | 12 |
| Lymphoma | 2 | - | - | 5 | 7 |
| Carcinoma in situ | 3 | - | 1 | 1 | 5 |
| Carcinoma of the lachrymal gland | 2 | - | - | - | 2 |
| Neuroendocrine carcinoma | 1 | - | - | 1 | 2 |
| Adenoid cystic carcinoma | 1 | - | - | - | 1 |
| Total | 195 | 54 | 1 | 19 | 269 |
It was observed that only 29 patients (10.7%) received prosthetic rehabilitation, of whom 13 were female (44.8%) and 16 male (55.2%). Table 2 shows that rehabilitation occurred mainly in patients with retinoblastoma (79.3%), lesions located within the orbit (42.2%) and lower eyelid (42.6%), bilateral lesions (82.8%), clinical stage II (51.7%), and enucleation surgery (89.7%). Age of rehabilitated patients was lower than non-rehabilitated patients (p<0.001) and all patients received advice on rehabilitation and were alive at the time of data collection.
Factors Associated with Rehabilitation with Prosthetic Eye
| Variable | Categories | Frequency (n/%) | p* | |
|---|---|---|---|---|
| Rehabilitated | Not Rehabilitated | |||
| Kind of tumor | Squamous cell carcinoma of the conjunctiva | 1 (3.4) | 19 (7.1) | <0.001 |
| Basal cell carcinoma | 0 (0) | 156 (65.0) | ||
| Retinoblastoma | 23 (79.3) | 23 (9.6) | ||
| Malignant Melanoma | 4 (13.8) | 14 (5.8) | ||
| Rhabdomyosarcoma | 1 (3.4) | 11 (4.6) | ||
| Other | 0 (0) | 17 (7.0) | ||
| Gender | Male | 16 (55.2) | 118 (49.2) | 0.541 |
| Female | 13 (44.8) | 122 (50.8) | ||
| Anatomical site | Orbit | 114 (42.2) | 155 (28.9) | <0.001 |
| Upper eyelid | 41 (15.2) | 228 (42.5) | ||
| Lower eyelid | 115 (42.6) | 154 (28.7) | ||
| Bilateral | Yes | 24 (82.8) | 8 (3.3) | <0.001 |
| No | 5 (17.2) | 232 (96.7) | ||
| Clinical stage | I | 11 (37.9) | 158 (65.8) | 0.006 |
| II | 15 (51.7) | 53 (22.1) | ||
| III | 0 (0) | 2 (0.8) | ||
| IV | 3 (10.3) | 27 (11.2) | ||
| Type of surgery | Enucleation | 26 (89.7) | 28 (11.7) | <0.001 |
| Exenteration | 3 (10.3) | 192 (80.0) | ||
| Evisceration | 0 (0) | 1 (0.4) | ||
| Without surgery | 0 (0) | 19 (7.9) | ||
| Psychological support | Yes | 7 (28.0) | 18 (72.0) | 0.004 |
| No | 22 (9.0) | 222 (91.0) | ||
| Age** | 11.6 (18.5) | 50.7 (23.7) | <0.001 | |
| Advice on rehabilitation | Yes | 29 (100) | 19 (7.9) | <0.001 |
| No | 0 (0) | 221 (92.1) | ||
| Death | Yes | 0 (0) | 18 (7.5) | 0.127 |
| No | 29 (100) | 222 (92.5) | ||
* Chi-square test
** Mean and standard deviation (Mann-Whitney test p-value)
Multiple logistic regression analysis (Table 3) showed significant association of rehabilitation with enucleation surgery and lower age (R2=0.47; p<0.001).
Results of Multiple Logistic Regression Analysis of Factors Associated with Rehabilitation with Artificial Eyes of Patients Attending the Araújo Jorge Hospital (n=29)
| Variable | Regression Coefficient | Wald | p-value | Odds Ratio (95% Confidence Interval) |
|---|---|---|---|---|
| Enucleation surgery | 2.291 | 10.43 | 0.001 | 9.9 (2.5 – 39.7) |
| Age | -0.040 | 11.14 | 0.001 | 0.11 (0.94 – 0.98) |
Nagelkerke R2 = 0.47
DISCUSSION
This study showed that the most prevalent tumor in the orbital region was BCC (58.0%), a neoplasm of epithelial origin caused mainly by ultraviolet radiation. Another prevalent tumor was RB (17.1%), an intraocular tumor of genetic origin. Exenteration was the most common surgical treatment (92.9%) of the patients underwent surgical procedure, but just 11.6% of them were rehabilitated. The factors influencing rehabilitation of surgical resection were the lower age of the patient and enucleation surgery as the treatment approach.
Malignant tumors of the orbit and the orbitomaxillary region constitute 4-8% of head and neck malignancies. The lesions can be primary orbital malignant tumors or can invade the orbit from the eyelids, the eyeball or the paranasal sinuses, especially the maxillary sinus and ethmoids [22].
Few studies focuses on the prevalence and incidence of malignant tumors in the orbital region. A study from Seccia et al. [23] analysed retrospectively 154 orbital tumors and found that BCC and scamous cell carcinoma were the most common malignant tumors of the orbital region. The anatomical characteristics of the are and the aggressive behavior of some BCCs of this site make the tumoral propagation quickly infiltrating [23].
The high prevalence of BCC as the main neoplasm was not surprising because there is a lack of available information in our region with regard to the side effects of actinic radiation on the skin. As this kind of tumor develops silently, in general its diagnosis is delayed. In the same way, the presence of RB as the second-most prevalent tumor was to be expected, due to the specificity of the sample under investigation, taken from an oncological treatment center. This tumor represented 17.1% of cases in our sample of which 86.9% were treated by enucleation of the ocular globe.
The third most prevalent tumor was the squamous cell carcinoma of the conjunctiva. According to Basti and Macsai [24] squamous lesions of the cornea and conjunctiva are uncommon but important because of their potential for causing ocular and even systemic morbidity and mortality. Their clinical presentation extends across a wide spectrum and differs based on the degree of pathologic involvement. The latter can range from mild to severe dysplasia to full-thickness epithelial dysplasia (carcinoma in situ) and invasive squamous cell carcinoma. Squamous neoplasms can involve the conjunctiva or the cornea individually but more commonly start in the conjunctiva and extend across the limbus to involve the adjacent cornea [24].
Exenteration of the orbit or enucleation of the ocular globe is a radical and disfiguring surgical procedure. Exenteration in malignant orbital tumors is the last option in treating these lethal diseases [4]. For the patient, in particular, the decision to accept this treatment approach is excruciating, because part of their face will be left disfigured [8]. Nobody can doubt the importance of knowledge about the prevalence of these malignant lesions in the orbital cavity and ocular globe, and about rehabilitation alternatives for the patient [1]. The techniques of excision and reconstruction are similar for every kind of neoplam. The reconstuction presents many solutions that are chosen based on the extent of the exeresis to reach a good functional and aesthetic result [23].
An epidemiological study with a cross-sectional design was conducted, based on analysis of medical records of patients who underwent enucleation or evisceration of the eyeball assisted in the Department of Ocular Plastic and Orbit of the HRSJ from December 1999 to December 2009.
The majority of these patients did not receive any kind of post-surgical rehabilitation. Those patients who did receive rehabilitation had special features in common, such as the occurrence of the condition at an early age and having the ocular globe enucleated. Our results would indicate that young people whose ocular globe had been removed sought rehabilitation, although this percentage was low. We also investigated if psychological support was important when deciding on both surgical treatment and the rehabilitation process. We observed that few patients (n=25) received help in their decision-making and just seven received post-surgical rehabilitation. Therefore, this aspect would not have influenced the rehabilitation process.
With regard to the high prevalence of cases of BCC in the orbital region with ocular involvement and which were submitted to exenteration, our results are in agreement with those of the literature. In a study referring to the frequency of BCC in the facial region, 12.6% were located in the orbital region [8]. In another study, BCC was also the most prevalent malignant tumor accounting for 40.5% of cases [6]. Based on this evidence, it is necessary to develop preventive actions in order to protect people from the adverse effects of ultraviolet radiation.
RB was the second-most prevalent tumor. In this research, it occurred in the majority of the young patients, and from a total of 29 patients who had undergone rehabilitation, 23 were RB cases. This data is very important, because, as the patients affected by this disease are young, they tend to look for aesthetic rehabilitation independent of receiving psychological support. Although this tumor is relatively frequent in pediatric oncological centers, there are few studies on post-surgical rehabilitation procedures published in the literature.
Exenteration was the main modality of treatment employed in our research and its use depends on the nature of the tumor. In general, it is indicated for patients with malignant neoplasm of the orbital contents. Although it can be classified as total, subtotal, or supertotal, in our study this classification was not considered. Studies have been published reporting the features of the surgical techniques used, such as enucleation, exenteration, and evisceration [4,6-7] and, as was seen, the choice depends on the characteristics of the lesion.
One disappointing result was the low percentage of patients who were rehabilitated with aesthetic orbital or ocular prosthesis. Only 29 patients underwent this post-surgical procedure, even though it is known that prosthetic rehabilitation is important, especially in children who need a normal development of their orbital region. However, there are few studies in the literature reporting the real causes for not undergoing a rehabilitation process [1,20,25].
In our study we also investigated how fundamental psychological support was to this process. We noted that only 25 out of 269 patients received psychological assistance, a low percentage. In the same way, only 48 out of the total number of patients received guidance with regard to receiving aesthetic prosthesis rehabilitation. The reason for this low rates of rehabilitation could be due to the lack of dental surgeons qualified to carry out this procedure in our region. Furthermore, it is very important to have specialized professionals working in a multidisciplinary team to treat malignant tumors [4,26]. Unfortunately, this is not always possible in this region.
In patients with facial deformities, surgical resection can frequently be extremely mutilating and disfiguring, presenting exceptional challenges for both the surgeon and the maxillofacial prosthodontist to achieve acceptable aesthetic and functional solutions. However clinical conditions frequently limit the possibilities for satisfactory treatment. In addition, the poor access to appropriate care in the public health system is a serious limitation for most patients and, consequently, patients may still experience lifelong disfigurement and dysfunction [27].
This research was carried out based on data from the archives of a public hospital that is highly respected for its cancer treatment in Goiás State and funded by the Brazilian Public Health System. The Brazilian public healthcare system is responsible for 75 percent of the cancertreatment made in the country. Mapping indicators for use of services in cancer care - hospitalizations, chemotherapy, and radiotherapy financed by the public health system - showed evidence of inequality in access, due to the small number of treatments in Brazil's poorer regions. Our results suggest an urgent need to improve the overall assistance given to patients with malignant orbital tumors.
CONFLICT OF INTEREST:
The authors confirm that this article content has no conflicts of interest.
ACKNOWLEDGEMENTS
None declared.


