“Evidence-Based Dentistry in Oral Surgery: Could We Do Better?”
Abstract
Evidence-based Dentistry (EBD), like Evidence-based Medicine (EBM), was born in order to seek the “best available research evidence” in the field of dentistry both in research and clinical routine.
But evidence is not clearly measurable in all fields of healthcare: in particular, while drug effect is rather independent from clinician’s characteristics, the effectiveness of surgical procedures is strictly related to surgeon’s expertise, which is difficult to quantify. The research problems of dentistry have a lot in common with other surgical fields, where at the moment the best therapeutic recommendations and guidelines originates from an integration of evidence-based medicine and data from consensus conferences.
To cope with these problems, new instruments have been developed, aimed at standardizing clinical procedures (CAD-CAM technology) and at integrating EBM achievements with the opinions of expert clinicians (GRADE System).
One thing we have to remember however: it is necessary to use the instruments developed by evidence-based medicine but is impossible to produce sound knowledge without considering clinical expertise and quality of surgical procedures simultaneously. Only in this way we will obtain an evidence-based dentistry both in dental research and clinical practice, which is up to third millennium standards.
1. INTRODUCTION
EBM was born in the early 1990s, and Evidence-Based Dentistry (EBD) developed a few years later. However, it should be acknowledged that improvements in Dental education and practice have taken place over the last 100 years.
The goal of evidence-based dentistry is to assess which is the best available care for the patient, by taking into account all available high-quality evidence. A resulting achievement is that both health care practitioner and patient are reassured that treatment options have been tested in a scientific way, so that they can more easily trust that specific cure. The more we will move toward broad-based use of evidence-based dentistry in clinical practice, the more physicians will benefit through better and standardized clinical guidelines that will help in decision-making and improve the quality of clinical results [1,2].
One of the most important issues in deciding what kind of therapy is more indicated, is to consider the balance between the potential risks and benefits of a treatment. A framework for evidence-based decision-making includes formulating the clinical question, retrieving and appraising available evidence, and then considering whether the evidence can be applied to that single case. It is mandatory for all health care providers to reduce treatment burden perceived by patients, by selecting appropriate therapies and explaining possible unavoidable risks.
The purpose of this article is to explain what we have done in EBD field, if what we have done is correct and if we can do better.
In particular we would like to stress your attention on the possible tools that we can use to improve EBD in the third millennium in particular in the field of oral surgery.
2. EBD NOWADAYS
a. “Best Evidence” and Limitations (and Available Evidence in Oral Surgery)
Evidence-based dentistry (EBD) is an approach to oral health care that requires the judicious integration of systematic assessments of clinically relevant scientific evidence, related to the patient's oral and medical condition and history, with the dentist's clinical expertise and the patient's treatment needs and preferences. Evidence-based care is now regarded as the "gold standard" in health care delivery worldwide [3].
The term best evidence means the evidence furnished by well designed studies. But is it always possible to have well designed studies, and what does it mean?
Dentistry is a special field where the best evidence cannot always be applied to the single patient. In our work we must align to protocols and guidelines for therapies and prognosis, but we have to also consider patient’s preferences and values, as well as costs and personal esthetic sense both for us and the patient.
Several studies are concordant to show that methodological issues such as the technique of randomization, unbiased assessment of endpoints, blinding, and prospective estimates of sample size were lacking in many trials [4-7]. Moreover surgical RCTs or meta-analyses remain scarce in our field.
The difficulties related to RCTs in surgery are mainly: the feasibility of randomization (ethical issues, emergency setting, palliative care), the learning curve, standardization of the procedures, poor surgical performances, and patients’ and surgeons’ equipoise [8].
Hence nowadays well designed non-randomized studies could still be considered a good alternative to RCTs in such areas where it is impossible to apply RCTs [9]. RCTs themselves must be improved, by promoting education in clinical epidemiology, by developing alternative methods of randomization and by encouraging whenever possible blinded observers, as the double blind is not feasible in the surgical field.
The Evidence-based approach has increasingly shaped medical practice and education, so much so that in January 2007 Evidence-Based Practice was voted as one of the most important medical advances in the last 166 years [10]. Nevertheless, some researchers still do not agree to consider this scientific movement as entirely positive. For instance, 96% of the articles do not satisfy the inclusion criteria of the evidence-based research [11]. What is the meaning of this datum? Does it imply that only 4% of articles are valuable because they were the only correctly executed? That 96% of studies conducted in medical research are not reliable?
Surgery (and dentistry), which has always been considered a qualitatively lower branch compared to medicine for its humble origins, allows us to better understand this methodological problem.
In 1996 Horton compared surgical research to comic opera [12]. Experimental studies (RCTs or quasi-RCTs) which constitute the core of EBM, are still scarce in surgery although their number has recently increased [13]. In the early 90s surgical RCTs were the 7% of published articles, which were mostly retrospective studies or case series [14]. A more recent review showed that only 3.4% of all publications in leading surgical journals are RCTs [15].
Most available evidence in the field of surgery comes from ‘‘non-experimental’’ studies (i.e. non-randomized studies, case-control or cohort studies, and qualitative or narrative reviews), leading obviously to a lower level of evidence on the scale established by EBM [9].
b. “The Superdentist” in the era of EBD
Although EBD is fine, it is important to understand that dental practitioner is not so commonly involved in evidence matters. Usually it remains a marginal part of health care; indeed private practice constitutes the major part of dental practice, and the dentists remain imprisoned in such a huge operative workload, that there is often no time to refresh the past knowledge or to update about new procedures.
In general medicine, it has been stated that reading 19 articles per day 362 days a year is necessary to keep abreast of medical advances [16]. Of course, it is impossible to read such bulk of material and thereby it is very difficult to administer to every single patient the best therapy he needs in terms of EBD. Indeed some studies, performed in the United States and The Netherlands, suggest that up to 40% of patients do not get evidence-based therapy [17,18]. There is no reason to believe that dentistry performs better.
Dentists, such as surgeons in general, are at least as busy as general clinicians; they have to face with increasing operative volume, clinical visits, hospitalization care, growing administrative formalities, marketing about materials and tools, and also evidence-based dentistry (Fig. 1).
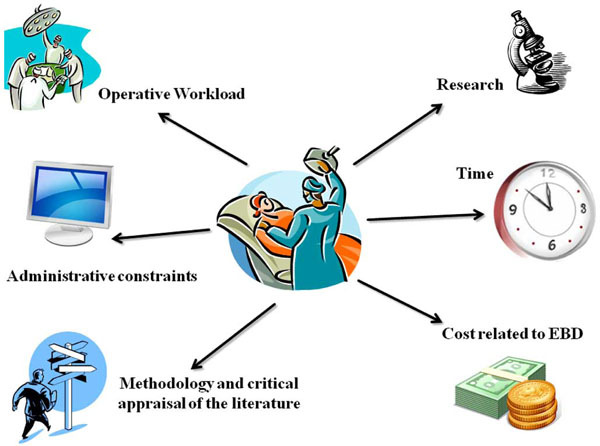
Superdentist in the world of evidence-based dentistry (adapted from Slim K [22]).
Furthermore, it is well known that surgeons are not willing to endorse all evidences because of their own personalities (self confidence, lack of patience, important and quick clinical decisions, decisive actions during operations). An Australian survey on the management of colorectal cancer patients showed that only 61% of surgeons were aware of the evidence. Higher scores were observed in surgeons who had practiced in capital cities for at least a few years, or had been involved in research or in guideline development [19].
Young surgeons (residents) are probably more willing to incorporate the principles of EBD than senior surgeons. A recent study, evaluating the effectiveness of an EBM teaching program in neurosurgery, clearly showed that by dedicating some specific time and resources it is possible to incorporate the EBM principles into the education of residents in a busy surgical unit [20]. Whether these principles are to be implemented daily remains to be demonstrated [9].
Again there is no reason to believe that in the field of dentistry it should be any different. Probably the best way to handle these problems is to re-start with the new generations of dentists and oral surgeons: in a world where we are bombed by several advertisements from industries and companies promoting new materials and tools, young practitioners should be helped to develop a critical appraisal of circulating knowledge. This is the purpose of EBD and his role in the third millennium challenge.
c. Limitations of EBD in Dentistry and Oral Surgery
Because surgical intervention is not like administering a pill, surgical field has some peculiar difficulties. Even though these problems could be overcome and more RCTs performed, 60% of surgical questions could not be answered by any RCT [21].
In this view we have to consider the difficulty to base clinical decision on RCT, above all in the field of surgery. Most clinical decisions in the ‘‘real world’’ remain based on clinical judgment and expertise, on the results of non-randomized studies, and even on the influence of opinion leaders [22]. Randomized trials often include ‘‘reliable’’ hard data that can be used to interpret the results in a homogeneous population. In contrast, a ‘‘good clinician’’ uses other ‘‘soft’’ data that can be omitted in RCTs (severity of symptoms, severity of co-morbidities, socioeconomic conditions) for clinical decisions about prognosis, diagnosis, or treatment. Such data are not always taken into account in evidence-based practice guidelines [23].
As a consequence, nowadays well-designed non-randomized studies could still be a good alternative to RCTs in such areas where it is impossible to apply RCTs [9].
It is also important to bear in mind that dentistry seldom reproduces the ideal environment found in scientific studies, as it deals with everyday practice and the immediate patients’ needs. Moreover surgical and dental methodology can scarcely be adapted to randomized clinical researches.
But what are the main difficulties in applying EBM to the surgical field?
First of all we have to assert that randomized, double-blinded and placebo-controlled trials are the only way not only to control investigator bias but also placebo effects. Indeed an important source of bias in surgical trials is the lack of blinding, as regards both patients and surgeons. Unfortunately, it is not always possible to blind all participants, as effectively shown in the trial by Majeed et al. [24], where the same wound dressing was used for patients who underwent laparoscopic and small incision cholecystectomy.
Especially if the primary outcome criteria are not recurrence of disease or even death, but subjective symptoms or quality of life measurements, a lack of blinding procedures may bias the results of these trials. This bias can be minimized by assessing the procedure outcome by independent investigators. Furthermore, it remains difficult to standardize the tested surgical procedures: the latter continuously evolve and the complications decrease with the surgeons’ improving skills. As regards, the results vary across individual surgeons because the participating operators vary in their surgical skill and experience. All participating surgeons should undergo appropriate training before the start of a randomized controlled trial to reach a certain minimum of standardization [25].
As a consequence, in all surgical fields it is very hard to base knowledge only on data obtained through the Internet and databases (EBD methods) because of the complexity of this field, where the result is usually related with some emotional, individual, and uncountable aspects (such as experience, anxiety, technique preferences) that could anyway affect clinical outcome.
In such a specific field, both the surgeon’s training and way of teaching are important. We think that a strict collaboration between old surgeons and young surgeons could be useful. Richards’ study brings support to this concept: he thought that the learning process must be considered separately for knowledge, critical appraisal skills, attitudes and behavior. He considered two types of teaching models for assessing learning achievement: stand-alone teaching and clinical integrated teaching. His study showed that stand-alone teaching improved knowledge but not skills, attitudes or behavior while clinically integrated teaching improved knowledge, skills, attitudes and behavior [26]. This study confirms that teaching of EBD should be moved from classrooms to clinical practice to achieve improvements in research and clinical outcomes.
3. TOOLS TO IMPROVE DIAGNOSIS, PROGNOSIS AND TREATMENTS IN THE THIRD MILLENNIUM
a. The GRADE System
The limits of EBM in medical and surgical fields have led in the last few years to a new methodological approach in assessing evidence and developing guidelines.
Indeed the results derived from published RCTs are not anymore sufficient to produce knowledge especially in the field of surgery, where it is not possible to fully standardize results which largely depends on single surgeon’s skill.
Statisticians and researchers have tried to overcome this issue by constructing new methods, which could allow to integrate expert’s opinion, based on their long lasting experience, with the accumulating data coming from RCTs.
A group was created in the year 2000 as an informal collaboration of experts with the aim of addressing the shortcomings of present grading system in healthcare [27]. It was acknowledged that RCTs were not able to create new knowledge in all fields of medicine.
Therefore, in the last decade a new system to derive clinical recommendations from available scientific literature has been developed, by taking into account both scientific evidence and experts’ opinion. This system is named GRADE, an acronym for Grading of Recommendations, Assessment, Development and Evaluation, and involves guideline developers, methodologists and clinicians all over the world.
So the GRADE System utilizes both EBM and “experts”’ opinion. This System is mainly aimed to overcome the classical limits of evidence-based movement by integrating the information derived from studies with optimal statistical quality with experts’ opinions that can add new experiences.
The pyramid of EBM modified according to the GRADE System is slightly different from EBM classical pyramid: even if the general superiority of experimental studies over observational studies is recognized, it is possible that an observational study is assigned a higher score while on the contrary that an experimental study is downgraded to a lower level.
Experts are encouraged to share their opinions through the Delphi “method”, which helps to find solutions to complex problems, by increasing the communication inside a group (or Panel) and at the same time by limiting the power of each single individual. Participants to the Delphi panel are stimulated to produce new ideas which they consider more suitable to solve a given problem and these ideas are subsequently diffused among participants to the panel, so that they can individually reconsider their ideas, without being obliged to discuss them in front of the group.
The reproposal of strategies that were suggested by the panelists continues until shared opinions are reached. So it is easier to reach a form of consensus on one or more issues to a given problem, and more importantly this technique avoids the possibility that someone prevails simply because of its personality. Furthermore, this Delphi “process” helps to find solutions to difficult questions, also increasing the communication inside a group while contemporary limiting the influence power of single researchers.
The ultimate aim of this technique is to obtain and summarize the opinions of several experts on a given debatable question. Therefore, the GRADE system utilizes both the EBM approach and the opinion of experts given by a “democratic approach”. The data accrued by this methodology can be synthesized with a recommendation, graded as “Strong” if shared by more than 70% of participants or “Weak” otherwise.
The merit of GRADE is that it does not eliminate judgments or disagreements about evidence and recommendations, but rather it makes them transparent. Moreover, it combines methodological rigor with interdisciplinary participation.
This practice is not yet widespread in the dental field, according to our experience: the limited number of these studies in the current literature is the perfect demonstration. A common effort to bring this useful method in the field of dentistry and oral surgery will certainly be needed in the future.
b. CAD-CAM Technology Applied to Implantology
In the field of EBD a special attention has been given to technological innovations that could improve the reproducibility, standardization and safety of treatment, both from the standpoint of the physician and the patient's. We think that the Third Millennium’s Dentistry cannot adequately perform without this approach: this is only the beginning, but who knows what innovations will we face in the coming years.
The technology of CAD-CAM (computer aided design-computer aided manufacturing) applied to surgery led to the creation of a software (Nobel Biocare, Procera System, Gotheborg) capable of running the so-called computer assisted surgery.
Jaw bone images transferred from DICOM data filmed by CT scanner were fed to the software and manipulated and converted to a virtual three-dimensional (3D) model of the treated jaw (Fig. 2).
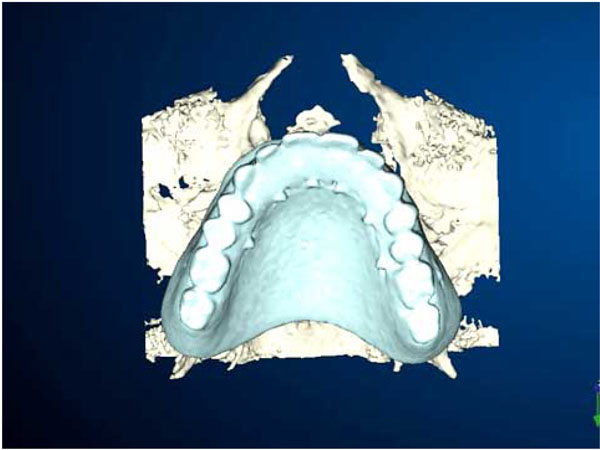
3D images derived from CAD-CAM software applied to computer assisted surgery, notice the virtual surgical template.
The virtual 3D model gives the surgeon a realistic view of the anatomic bony morphology of the patient allowing the surgeon to virtually execute the surgery in an ideal and precise manner. The surgeon can visualize important anatomical structures and create a virtual surgical template, which will guide the insertion of implants, providing information on angle, direction, depth of insertion and distance from important structures.
This method, in addition to stereolithography, has been used to develop a new generation of precise surgical templates (Fig. 3).

Stereolithography that creates the surgical template. Notice the directional cylinders that drive the implant positioning phase
Stereolithography is a new technology that can create physical models by selectively solidifying an ultraviolet-sensitive liquid acrylic resin, using a laser beam accurately reproducing, for instance, actual maxillary and mandibular anatomic dimensions. With these models it is possible to produce surgical guides that can be used in vivo to place implant in the same sites and directions as in a planned computer simulations (Fig. 4) [28, 29].

3D images derived from CAD-CAM software. Notice the implants and the virtual bone.
With the planning software, the practitioner determines the implant position according to both ideal position dictated by the definitive prosthesis and the available bone volume. The template can be used not only in critical anatomy but also to place the implant in an ideal position in the bone because it eliminates possible manual placement errors and match planning to prosthetic requirements in a precise manner [30].
Regarding the precision of the drilling supported by a surgical template, a somewhat sophisticated drilling experiment was performed on the bone model using a surgical template, and the displacements of the directional cylinders from those of a simulation were measured. They were nearly 0.1 mm, and would be satisfactorily precise when applied clinically. However, in the real clinical situation, the surgery must be performed in a narrow oral cavity, where the motion of the turbine handpiece is inevitably restricted. Although the precision of drilling supported by a surgical template might decrease, certain precision might still exist [31].
Also in the field of restoration CAD-CAM technology will bring great advantages. It is claimed that dental CAD–CAM restorations not only simplify the production of restorations but also match the quality of conventionally cast restorations. In addition it is only through the introduction of CAD–CAM technologies that milled titanium and zirconia ceramic restoration have been made available in dentistry [32].
In conclusion this technology enables to better standardize surgical quality and to level surgical skills, for the first time, among skilled and novice operators.
Although this technique is not yet widespread, we think that in the future it will help research in oral surgery from a methodological point of view by providing objectivity, which still lacks in this field. This is just an example but it can make us understand the methodological backwardness of the surgical part in the field of research, for reasons that are intrinsic to the same subject; however, huge efforts have been made to improve the objectivity of the reading of the clinical results.
4. “THE PENDULUM OF KNOWLEDGE”: A TRANSITIONING ERA
The last 30 years have witnessed large oscillations in the methods to produce and convey clinical knowledge that we have called “The Pendulum of Knowledge” (Fig. 5).
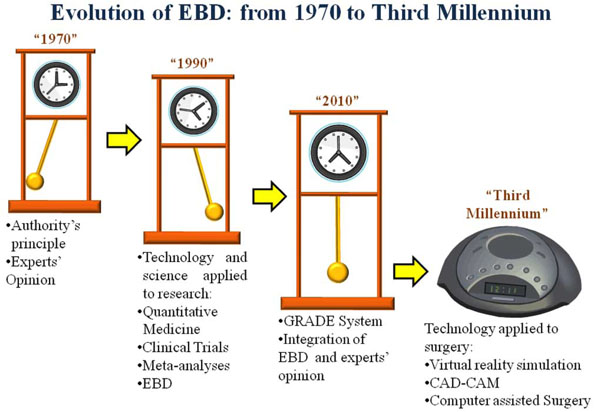
The pendulum of knowledgeâ€: from grandfather clock to digital clock as a metaphor for the evolution of methodology research.
We have gone from the era of Experts’ opinion / Authority’s Principle to the era of evidence-based medicine and we are now entering a new age where the two approaches are substantially mixed up through the GRADE system. Furthermore another tool is emerging in the last few years: Computer-assisted surgery.
In the 70s clinical knowledge mainly resided in the brain of clinical experts, who had devoted their life to the care of individual patients. They had mainly learnt from their bedside experience under the guidance of their teachers, and likewise passed their knowledge to their pupils using both verbal and non-verbal communications. In that period exchanges between clinicians and researchers were limited, clinical knowledge was condensed in large textbooks, and there were linguistic barriers between countries. The progress in disease diagnosis and treatment was rather slow: we would like to represent this archaic situation pointing the pendulum of our grandfather clock completely to the left side.
With the advent of English as an international “Esperanto” and World Wide Web, international communications have been magnified and the speed of clinical progress has incredibly increased, as witnessed by the sprout of thousands of specialized medical journals.
In the 90s there has been a useful reaction to the overpower of experts’ opinion. Evidence-based medicine tried to base clinical practice on clear-cut evidence coming from clinical experiments (randomized clinical trials) and systematic observations.
Personal impressions should be replaced by rigorous measurements, sparse observations by systematic collection of series, observational studies by randomized clinical trials whenever feasible. This approach has further magnified the progress in medicine. This innovation in health research was represented by moving the pendulum of our grandfather clock completely to the opposite side, to underline how EBD has unhinged the methodology of medical research within a few years (in our ideal model just the seconds the pendulum needs to move from one side to the other).
Now a new approach is gradually taking over, the GRADE system. Evidence-based medicine is still fundamental, but experts’ opinion has been re-evaluated. It is necessary to take advantage of the rigorous methods produced by evidence-based medicine, especially when planning and evaluating research studies; however, it is impossible to produce sound knowledge without simultaneously considering clinical expertise and quality of surgical procedures. This compromise is represented by our pendulum stopped just in the centre of our grandfather clock, balancing the two opposite operative philosophies.
In the last years in the field of oral surgery we have seen, perhaps for the first time in dental research, a new method to optimize the design and execution of implantology surgery.
We think that this could be the future of the Third Millennium: we will pass from an analogical grandfather clock to a digital clock, where all the qualities of the old methods will condense into a more functional, efficient and safe system. We are aware of the little fascination that the “digital system” has compared to the ancient “analogical system”, where the physician was the only expert able to create health through his knowledge, experience and intuition, but we are also aware that just this fascination was the cause of some mistakes.
This is a simple metaphor to explain how the advent of computerized systems, applied to clinical practice, can improve dental practice and EBD.
There are a lot of examples of this trend driven by lots of articles encouraging the use of digital systems in many branches of dentistry and oral surgery.
In addition to CAD-CAM technology and computer assisted surgery previously described, there are other possible applications of computer technology.
For example the virtual reality (VR) simulators have been introduced into the dental curriculum as training devices for manual dexterity acquisition in tooth preparation tasks. A computerized simulator allows practicing tooth preparations in the presence of augmented visual feedback, resulting in enhanced performance under particular conditions, at least in novice students [33].
There is another study indeed, conducted in Toronto, where virtual reality simulator-enhanced training with laboratory-only practice was compared on the development of dental technical skills. The results of this study indicate that students, who had trained with the virtual reality simulator between 6 and 10 hours, improved significantly more than did the students in the control group [34].
These studies are all confirming how this technology should be exploited in the clinical context to bridge the gap between EBM in research methodology and EBD in the clinic where the surgeon's manual dexterity really makes a difference in treatments outcomes. Virtual reality, computer assisted surgery and CAD-CAM technology could really enable the achievement of a higher standardization of surgical quality criteria. Indeed while in normal surgical trials where a surgical technique is tested, the hand of the operator remains a critical factor that can greatly influence the outcome, in computer-assisted surgery we will face for the first time a technology that levels various manual skills, making them more similar, and allows the assessment of the same techniques eliminating peculiar factors such as the single operator’s manual skill, which is one of the biggest gaps of EBD applied to surgery.
5. CONCLUSION
In conclusion we can say that while criteria aimed to evaluate the quality of the study design (selection criteria, randomization, blindness, etc.) are well established, indexes of surgical quality have not been agreed upon.
It would be extremely useful to establish, at an international level, quality criteria for any kind of surgery but also for dentistry and oral surgery. Such indexes are urgently needed at every level of clinical practice: from restorative dentistry to oral surgery passing through orthodontics.
The application of computer-assisted surgery will surely improve dental practice by making oral surgery less dependent on surgeon’s expertise, skills and preference.
Computer-assisted surgery and the GRADE system will also facilitate the application of EBM in dentistry and oral surgery and will help to fulfill the gap between clinical research and routine practice, between researchers and clinicians.


