All published articles of this journal are available on ScienceDirect.
Probability-Utility Model for Managing Evidence-based Central Database
Abstract
The Probability-Utility Model is dependent on the clinical practice guideline for its function. The Model functions to provide decision analyses that demonstrate to clinicians and patients how personal preferences change the character of best evidence. Initially, patients are provided a clinical practice guideline based on “average patient” best evidence. The Model works to demonstrate how decision, utility, and cost best evidence impact on decisions. It offers to patients an explanation of these impacts. Thus, patients may become more informed about the choices that go into making optimal clinical decisions for their own personal health care. The model also provides for visual images to be used in discussing their personal choices when considering different treatment options and clinical scenarios. The calculations accomplished through the Model provide trade-off analyses by which discussions may be facilitated between provider and patient in reaching informed consent and optimal clinical decisions in formulating treatment plans.
INTRODUCTION
Many advances have been made in reasoning best evidence, especially in the form of judgments, inferences, and conclusions. While the Translational Evidence Mechanism provides the compact between researcher, clinicians, and patients by which this reasoning is developed, validated, disseminated, and refined, little progress has been made in producing technology to advance its practical use in displaying and utilizing this reasoning. Using dentistry as the discipline, the purpose of this paper is to present a Probability-Utility Model (Model),1 firstly, for displaying and utilizing best evidence at chair side for shared decision-making. This shared decision-making occurs between dental provider and patient within the dental assessment, evaluation and treatment planning appointment. Secondly, this model structures the inputs and outputs needed for storing and managing information within the central database of the Translational Evidence Mechanism.
DECISION ALGORITHM
Decision algorithms are decision trees, developed as expert systems. These systems structure:
- Clinical problems
- Analyze decisions and options, and
- Chose and implement clinical protocols or clinical practice guidelines
For dentistry, the decision tree that we propose for the central database is the Clinical Decision Tree of Oral Health (CDTOH) [1]. The CDTOH is a systematic understanding of an entire decision process in rendering clinical decisions. It identifies the order of outcomes involved in diseases, treatments and their protocols, and therapies in impacting positively on the oral health of patients. The outcome is the terminal end of each of its branches. The best evidence that constitutes these terminal branches include decision, utility and cost data. These data variables vest the clinical practice guideline with best evidence for use in shared decision-making. Using the CDTOH, a structure of relationships is made in the central database. This structure consists of 9 levels of evidence domains. These levels are developed to coincide with the flow of the decision process used in the CDTOH. Thus, each level of the hierarchy progressively adds information to the decision process. Thus, the clinical inquiry can follow the information trail until it reaches the actual data needed to respond to the initial inquiry. This is important to understand because the information collected along with the clinical inquiry: patient demographics, assessments, and follow-ups, will impact on the data used to vest the CPG. For each level, information is managed to prioritize the evidence that most impacts on the quantitative and qualitative nature of the response to query. For information technologists, this means structuring at each level requires normalization of the evidence across multiple tables, creating tables for decomposition (evidence stored secondary to the primary field key) and derivation (query responses that require calculation of the evidence). Information technologists perform these structuring tasks to improve and prevent delayed or time-consuming look-up of evidence in responding to queries. Programming language is used to provide the evidence to the generic template that displays the results of the query.
NINE LEVELS OF EVIDENCE
The nine levels of evidence include decision maker, physical and mental well-being, oral conditions, dental conditions, oral functioning, prevention and maintenance, judgment, values, and relationships domains. Each level has sublevels of variables that associate best evidence respective to each branch termini or outcomes. Information technology uses a dynamic process to prioritize each sublevel of evidence such that best evidence is found to vest the CPG. This is a dynamic process because knowledge and relationships between outcomes change; in other words, the branches and their termini within an evidence domain develop new or eliminate previous known branches and termini. The new developments are in response to changes that are gathered from new clinical inquires, updates in decision analysis, and differences in the meaning of best evidence as analyzed from patient choices, lifestyles, and behaviors. Thus, these changes develop different relationships in response to new findings.
In addition, the process must respond to queries that have single or multiple layers of comparison of evidence outcomes. While complex in visage, the administration of these types of queries are well within the administration of a central database. Using the decision maker level, as an example, four fields define decision makers: Dentist, Patient, Legal Surrogate, and Family members. Each decision maker impacts on whether treatment is ordered or not ordered. Often, evidence at this level will determine the outcome of whether a treatment plan is offered, accepted, or not accepted. When treatment effectiveness and efficacy is uncertain, access and utilization of dental services by patients are uncertain. Often decision makers will rely on their personal utilities: previous dental experiences, health beliefs and behaviors, preferences, and health goals, in making decisions about access to dental care services. These lack the support from best evidence to clarify these utilities within the context of treatment outcomes. For example, evidence on functional status and accessing dental care services often affects how treatment options are communicated and decided upon by not only patients, but their dentists, legal surrogates, and family members who may weight their personal utilities in adverse to potentially positive effective and efficacious outcomes. Evidence on functional status provides estimates on life expectancy. Life expectancy is predicted by demographic variables such as age, gender, and race. Utility measures include quality-adjusted life years (Miyamoto, Wakker, Bleichrodt, & Peters, 1998), or other utility assessments (Lin, Hwang, Chung, Huang, & Chen, 2006; Miyamoto, 2003; Miyamoto & Eraker, 1989). Cost is a variable considered later in the decision-making process when trade-offs between treatment options are discussed; unfortunately, cost may impact at this level when older adults, their dependents or caregivers, impose preferences that rate higher estate interests over quality of life issues. Thus, the inclusion of multiple decision makers may make shared decision-making complex for access to dental care services, compliance in utilization, and improvements in health outcomes from potential dental care services.
INPUTS
Research
Research inputs vest the central database with data. These research inputs are utilized by the translational researcher's role in providing best evidence for the central database, evidence that will be used to respond to clinical queries of dental providers for their patient consultations. Thus, there are two separate databases within the central database: An evidence-based database and research-vested database. The research database is important because the data inputted, then subsequently retrieved, is used to systematically derive best evidence for use in structuring outcome evidence for deriving clinical practice guidelines (CPGs). The evidence-based database provides clinical queries with CPGs that conform to a specific organization of decision (outcome), utility (preferences and values), and cost best evidence. The Probability-Utility Model defines these inputs that are more directed (requesting input of data in strict formats) than reasoned (summary statements) in providing research data for peer review by translational evidence researchers. The data inputted may be derived from research findings, unpublished manuscripts, and published articles.
Clinical Practice
Clinical inputs are specific inputs requested of clinicians. Clinician input provides clinical significance rankings of translational evidence researcher developed:
- CPGs
- CPGs returned as a product of shared decision-making, or
- CPGs returned with follow-up assessments at patient periodic dental examinations.
Clinicians are provided a CPG with best evidence specific to a stated clinical question. The clinician assesses best evidence for its applicability to private practice or patient care. Combined intuitive knowledge, clinical expertise and long-term monitoring of patient care qualifies the clinician to make these judgments. Once this data has been acquired and evidence systematically reviewed, best evidence is inputted into the central, evidence-based database. From there, a CPG is derived and submitted for review of clinical significance by the clinician reviewer panel. A ranking is developed and inputted into the central, evidence-based database.
Other clinical inputs from private practice include CPGs in which patients have rejected the utilities and cost estimates based on "average patient" derived best evidence. In replacement of the "average patient" estimates, individual patients have stated estimates for their own. These estimates have been acquired from patient interaction and manipulation of the CPG during shared decision-making. Once the optimal clinical decision is made these are inputted back to the translational evidence researcher for updating best evidence from private practice. With a multitude of private practices, simulating research units, responding best evidence may be updated using Bayesian statistics. In this manner, the translational evidence researcher is alerted to derived CPG changes and acts accordingly to log, validate, and disseminated in various ways these changes. This dissemination may act as an alert, or flag to the patient electronic chart from which the clinical question arose, and email alerts to dentists and researchers who have subscribed for this service.
Likewise, at each patient periodic dental examination and when appropriate, updates to decision and utility best evidence are made. These outcomes of patient lifestyles and behaviors become new inputs to the database through the electronic chart and using the CPG. These inputs are based on observed differences from patient optimize decision and actual outcomes, behaviors, and compliance since the CPG implementation. Within the database, these changes are analyzed to update the CPG. These updates also serve to inform researchers and clinicians how the original accepted optimum clinical decision performed given the clinical scenario in which it was derived; in other words, the meaning in practice of the patient derived CPG.
OUTPUTS
Research
Research outputs are research questions posed to the TEM in responding to a clinical inquiry. In this scenario, best evidence does not exist to answer the clinical question. Therefore, a research question is postulated to acquire data from the research community. Research outputs must be flexible enough to aid in research project development.
Clinical Practice
Clinical outputs are in the form of a CPG. The character of the CPG input template is provided in response to the clinical question, an example of which is stated: In a population of female subjects, 85 years of age and older, functionally independent, will dental implants, compared to removable partial denture or no treatment, increase chewing function and chewing efficacy at a reasonable cost? Once the clinical question is submitted to the central, evidence-based database, a CPG is returned and attached to the patient's electronic chart.
Probability-Utility Model
The Probability-Utility Model provides derived evidence in the form of decision analyses that facilitate shared decision-making. Thus, the model not only defines inputs and outputs, but also the basis for why the central database and CPG product exists. It also provides:
- Best evidence modified by implementation in private practice
- Decision analyses for use in updating central database evidence, and
- Analysis of best evidence performance, or its meaning in practice, to researchers and clinicians.
Decision Analysis
The decision analysis presents evidence in various ways for visualization and understanding of the CPG. Firstly, the CPG is offered with annotated descriptions of the evidence shown: Fig. (1) annotations describe the various chewing function effectiveness outcomes. Fig. (2) annotates the utilities, and Fig. (3) the costs associated with each treatment option.
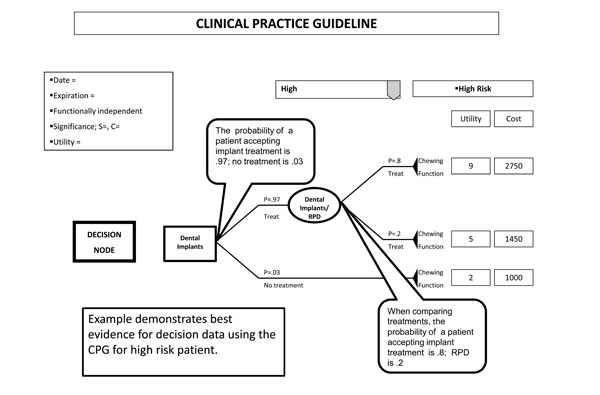
Example CPG for decision data.
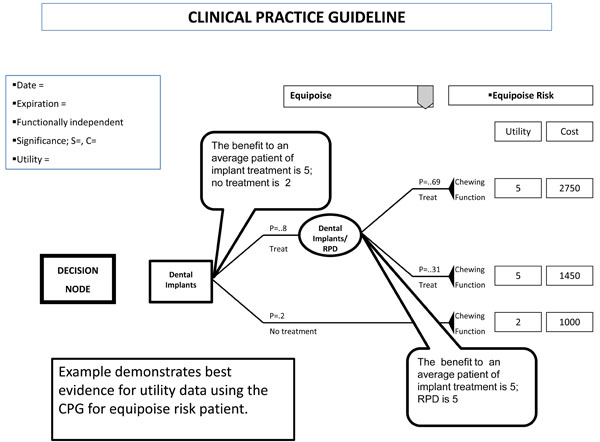
Example CPG for utility data.
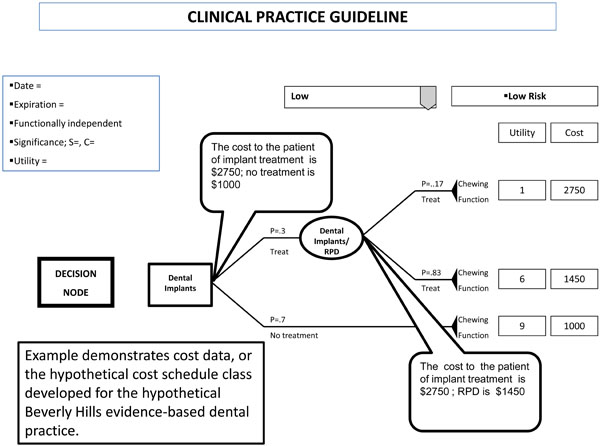
Example CPG for cost data.
The Probability-Utility Model, provides the trade-offs in considering which treatment option optimizes the clinical decision for the patient. This is done through roll-back calculations. Since the CPG is read from outcome to decision, so proceeds the calculations. To calculate the utility trade-offs between treatment options, the utility ranking is multiplied by the probability of the outcome. To calculate the cost trade-offs, the cost is multiplied by the probability of the outcome. Both provide dentist and patient with a description of the trade-off options for choosing the optimum clinical decision (Fig. 4).
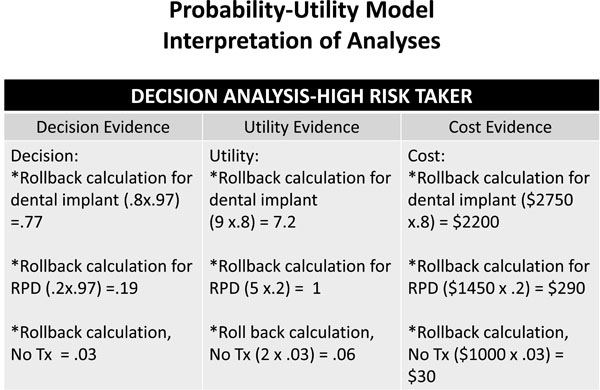
Decision-analysis for decision, utility, and cost data.
In this clinical scenario, comparisons of the stated treatment options in an average women, 85 years and older, functionally independent, and interested in state-of-the art treatment, dental implants offer this patient better chewing effectiveness far exceeding that provided by a RPD or No treatment. With no treatment, there are still costs. If no treatment is selected, than the patient may experience costs in other or potential treatments due to not replacing teeth. These treatments may include orthodontics, extraction of teeth, or periodontal conditions that may arise due to malocclusions. Using satisfaction rankings that an "average patient" with the same characteristics as this patient, dental implants far exceed that of wearing and eating with an RPD or no treatment. The cost of a dental implant compared to a RPD far exceeds that for a RPD or no treatment. With the options and their trade-offs, the dentist may discuss with the patient the option that best serves the patient’s needs, desires, and wants by comparing effectiveness, satisfaction levels, and cost. Thus, the optimal clinical decision is one that either accepts the option with the lowest costs or the largest expected value. If the patient, on the other hand, does not agree with the utility rankings, then the patient's rankings may replace those of the "average patient" with immediate revisions all trade-offs of each option having been recalculated. The interpretation of the analyses append the CPG so that viewing of CPG along with the interpretation may be seen simultaneously. Fig. (5) provides optimal clinical decisions based on risk level of the patient.
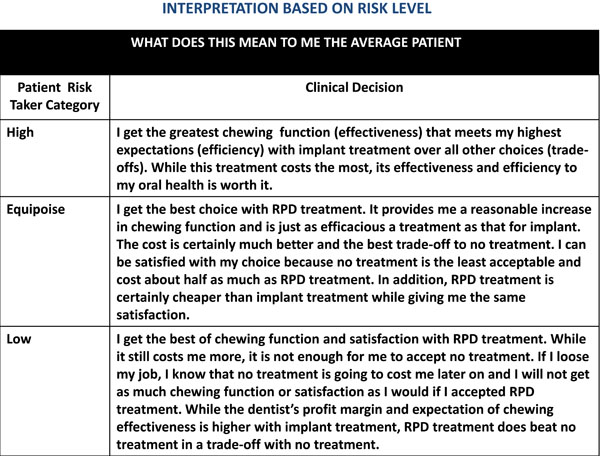
Interpretation of the decision-analysis using various risk levels.
Revision of Best Evidence
Modification of, best evidence within the central, evidence-based database may be performed simultaneously by updating the decision analysis. This revision of best evidence is done using Bayesian statistics. Updating best evidence determines if the prior probabilities of treatment options are mitigated by probabilities or revised probabilities of other events. In other words, the prior probabilities of treatment outcomes are conditional on the probabilities of the evidence witnessed in private practice and updated through the electronic chart using the CPG. This analysis is performed using Baye's theorem. Bayes’s theorem is a formula for calculating the conditional probability of one event from the conditional probability of the other event.
Aside from updating probabilities, patient decision-making and new knowledge changes the understanding of evidence. With sensitivity analysis, the translational researcher evaluates for clinicians and researchers ways decisions change as a function of changing probabilities, utilities, and costs. Sensitivity analysis also predicts the type of evidence that was most relevant to patients when considering trade-offs between two or more presenting treatment options. This information serves to enlighten understanding regarding patient preferences and values, behaviors, and compliance.
SUMMARY
The Probability-Utility Model is a way of understanding how optimize clinical decisions are derived through the use of a clinical practice guideline. The Model demonstrates how decision analysis is accomplished in explaining to clinicians and patients the use of best evidence in decision-making. Decision-making is comprised of decision, utility and cost data. These data variables are needed to make optimum decisions that take into account patient needs, desires and wants. The model sets forth the structure of these components within the clinical practice guideline. The Model, then, operates on each component to demonstrate what best evidence means to a decision. Then progresses to demonstrate the values a patient holds in assessing different treatment outcomes and cost/benefit trade-offs. By changing the values provided in an initial rendering of data, the patient may express their choices and visualize how personal preferences change best evidence, conform best evidence to their self-interests, and provide data to be used in updating current best evidence.
NOTES
1 Process of Evidence-Based Dental Decision-Making, US Patent Application No. 60/757,647, For: Methods of producing evidence-based decision, Filed: January 9, 2006, UC Case No.: 2006-296, File No. (Townsend and Townsend and Crew): 02307K-16300US).


