All published articles of this journal are available on ScienceDirect.
Radiographic Evaluation of Fixed Prosthesis in the Ha’il Province of Saudi Arabia
Abstract
Background
This study aimed to assess the marginal adaptability of fixed partial dentures (FPDs) performed by private practitioners in the Ha’il district of Saudi Arabia. Furthermore, complications associated with the restorations were also recorded.
Methods
A comprehensive analysis was carried out on 1139 periapical digital radiographs to determine the type of material utilized for the prosthesis, as well as to observe and record various radiographic findings, including the presence of periapical lesions, marginal discrepancy, and the presence of calculus. In addition, the sheet documented the condition of the neighboring tooth, stating whether it was healthy, absent, or decayed. An analysis was performed to determine the frequency distribution and cross-tabulation of the variables. The chi-square and Fisher's exact tests were employed to assess the possible association between the several factors described in this study.
Results
The prevalence rate of dental caries in the mesial adjacent teeth to single or multiple-unit FPDs was 138 (15.4%), and in the distal adjacent teeth was 136 (15.2%). The likelihood of an apical lesion and bone loss in adjacent teeth both mesially and distally was found to be higher, whereas the absence of calculus was more frequent than its presence. There was no statistically significant correlation found between having more than one unit prosthesis or a single crown and the occurrence of periapical lesions, bone loss, or calculus buildup on teeth mesial to FPDs (p > 0.05). However, at the distal adjacent teeth, statistically significant differences were recorded (p < 0.05). A statistically significant correlation was observed between the type of prosthesis material and the marginal integrity in mesial abutments for FPDs (p < 0.05) as well as single crowns (p < 0.05).
Conclusion
The frequency of dental problems identified in this study was higher in comparison to other investigations on FPDs. Ensuring the long-term durability of any restoration relies heavily on achieving optimal marginal fit and exact interproximal contacts, which are critical technical considerations.
1. BACKGROUND/INTRODUCTION
Tooth-supported fixed partial dentures (FPDs) are used to replace missing tooth substances and missing teeth in partially edentulous patients to restore oral function and esthetics [1, 2]. Fixed restorations remain crucial components of prosthodontic restorations, particularly in underdeveloped countries, despite the increasing use of dental implants [3]. FPD fabrication necessitates multiple complicated clinical and laboratory steps that are carried out in phases. Nonetheless, automated production procedures with the use of computer-aided design and manufacturing have become popular due to their potential to enhance the fit and homogeneity of crown restorations, hence increasing the probability of clinical success [3].
FPDs have long been regarded as the benchmark in terms of their dependability and practical application in clinical settings [4]. FPDs are composed of several materials, of which ceramics and ceramic metals are the most common. Multiple reports have indicated a significant rate of success for traditional porcelain-fused-to-metal (PFM) restorations following a thorough long-term assessment [5, 6]. However, in order to overcome the limitations of metal-based FPDs, some researchers have looked into the usage of biocompatible materials, such as zirconium oxide and lithium disilicate ceramics [7, 8]. One of the primary drawbacks of metal-based FPDs is the inclusion of a grey metal framework, which hinders the creation of natural esthetics throughout the fabrication process [9]. In order to achieve this objective, a novel framework utilizing ceramic materials is devised with the aim of enhancing the visual appeal and biocompatibility of restorations [10]. Nevertheless, because of their inferior mechanical characteristics, glass ceramics are mostly suggested for the anterior region or as a material for single crown restorations instead of multi-unit FPDs [10, 11].
Prosthodontic constructions require advanced technical skills and must be able to withstand the challenges of a biological environment in order to be successful. Such restorations are commonly evaluated in terms of their likelihood of survival and, to some degree, their level of success. Success and survival are frequently employed in literature to gauge the durability of a restoration. In general, success is determined by the demonstrable capability of a restoration to perform as anticipated, whereas survival implies that a restoration necessitates alterations or repairs in order to function. On the contrary, failure is defined as any circumstance that results in substitution. The fact that a patient considers a treatment successful may not align with the dentist's perspective. The failure of restoration efforts can be assessed using both technical and biological criteria. Biological factors contributing to the failure of restorative procedures include secondary caries, permanent pulpitis, necrosis, and parafunctions that lead to problems [12]. The interactions of dental prostheses, abutments, and supporting periodontal tissue are always changing. Both the clinical and histological documentation of these interactions is extensive, and the prosthodontist may face challenges in creating a seamless and healthy interface, which, if not optimal, could lead to prosthesis failure [13]. As an example, the extension of FPD retainer borders into the gingival sulcus should be seen as a compromise, yet it is often necessary to meet esthetic and/or retentive requirements. Furthermore, an optimal marginal fit is crucial for both the clinical and histological success of an FPD, as roughness caused by open margins or the type of material used can result in alterations in the bacterial ecology linked to periodontal disease [13, 14].
Periodontal degradation is a frequently occurring biological issue linked to FPDs [15-17]. Vergel de Dios examined the impact of crown margin location on the surrounding periodontium and found that supragingival margins were preferred. Moreover, there was no discernible difference in the effect of margin position on the periodontium [18]. Research conducted on the quality of FPDs in the Kingdom of Saudi Arabia has indicated that marginal discrepancy is a frequent complication that has a substantial impact on the survival rates of fixed prostheses [19]. Caries, a pathological problem, is also linked to the presence and quality of FPDs [15, 17]; the connection between the adaptability and position of dental prosthesis margins and the risk of caries has been well-documented. Nonetheless, caries susceptibility may be more affected by the marginal adaptation and quality of FPDs rather than the marginal position in relation to the gingival margin [20].
Previous studies have examined the technical quality and associated complications of FPDs in various regions of Saudi Arabia. However, there has only been one study conducted in the Ha’il region that examined the technical quality of crowns and FPDs [21]. This investigation found that the technical and biological problems observed were similar to those reported in previous studies on crowns and permanent dental prostheses, and the majority of patients expressed satisfaction with the restorations received [21]. Nevertheless, the study had a limited sample size. It is apparent that the Ha’il area in the northern region of Saudi Arabia has not been thoroughly investigated to examine the technical quality and issues related to crowns and FPDs; therefore, it is crucial to evaluate the technical excellence and potential complications of fixed prostheses and determine their consequences. This would allow dental professionals to implement preventive and restorative measures, ultimately leading to a significant improvement in the overall quality of life in terms of oral health. Thus, this study aimed to examine the marginal adaption of FPDs carried out by private practitioners in the Ha’il province of Saudi Arabia. Furthermore, complications associated with the restorations were recorded.
2. METHODS
This retrospective cross-sectional observational study was conducted in the Ha’il province of Saudi Arabia to analyse the marginal adaption and complications associated with abutment teeth for FPDs and teeth adjacent to those with fixed prosthodontic restorations. The present work was granted approval by the Research Ethics Committee (REC) at the University of Ha’il, with the reference number H-2023-170. Due to the retrospective design of the study, the ethics council of the College of Dentistry decided to waive the requirement for informed consent. This study was conducted in accordance with the guidelines set forth in the Helsinki Declaration of the World Medical Association (Fig. 1).
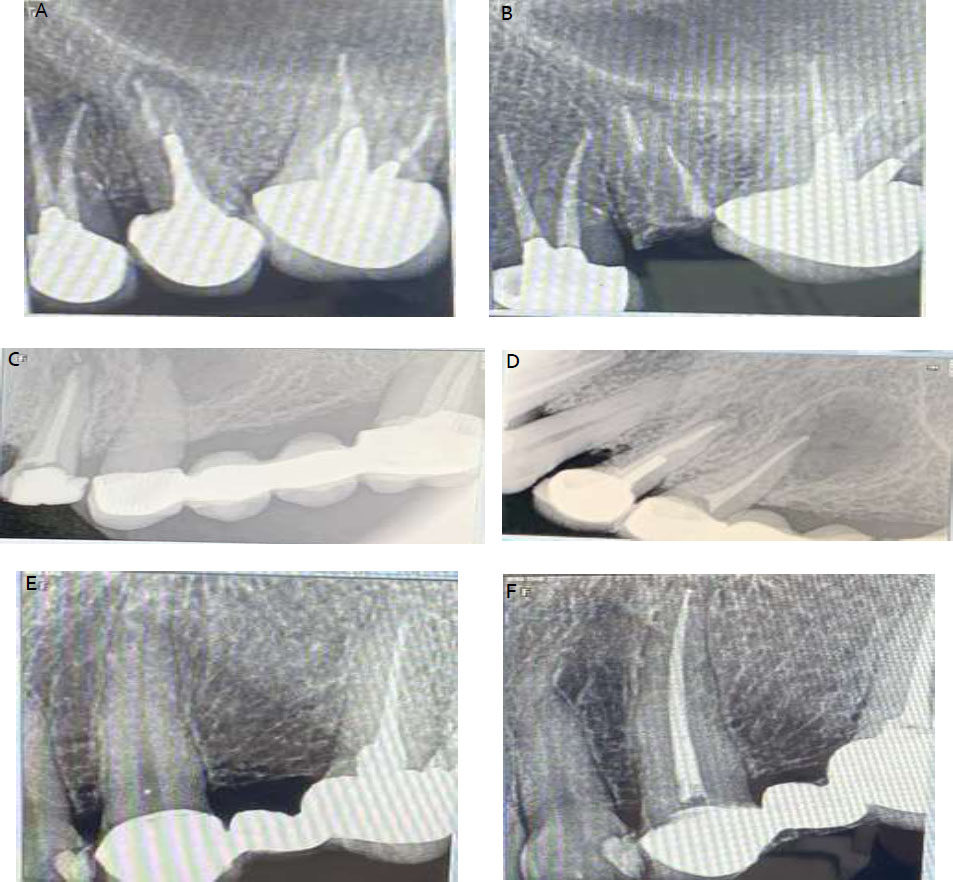
A, single unit FPDs in maxillary left quadrant; B, 5-year follow up showing fracture of the maxillary left second premolar; C, 4-unit FPD in maxillary left quadrant; D, 1-year follow up after root canal treatment of the mesial abutment with apical lesion still visible in the 4-unit FPD mesial abutment and the adjacent single crown with extruded sealer; E, 3-unit FPD; F, 1-year follow up after root canal treatment of the mesial abutment.
The dataset consisted of 1139 digital periapical radiographs acquired from patient records between 2012 and 2022. Inclusion criteria were patients older than 18 years who attended Ha’il Dental Center with full coverage single-unit or multiple-unit FPDs. Additionally, patients were required to possess a minimum of two radiographs, one taken after prosthesis cementation and the other taken at least one year after. Exclusion criteria were patients younger than 18 years old, partial coverage prostheses, and cases with incomplete records or without radiographs. No names, file numbers, or identifying patient data were collected. All information was stored safely with the authors. Out of the 1139 radiographs that were examined, 898 individuals (398 males and 500 females) met the criteria for inclusion.
The data collection procedure was dependent on information obtained from the patient's medical record and radiography software (CS-R4 software, Carestream Dental LLC, Atlanta, GA, USA). Each individual's data was recorded using a custom-designed form for the sole purpose of this study. The study employed the FOCUS™ Intraoral X-ray imaging system (KaVo™, Biberach, Germany). The radiographs were taken using an RVG-type sensor, which incorporates a film XCP holder to provide accurate positioning. The exposure settings consisted of a predetermined kilovoltage (kV) of either 60 or 70, accompanied by a customizable exposure duration spanning from 0.02 to 3.2 seconds. The period of exposure was contingent upon various elements, including the particular tooth under imaging, the patient's size, and the chosen mode of exposure. Three practitioners collected and documented the data in an Excel spreadsheet (Excel 2016, Microsoft®, Redmond, WA, USA).
A data collection sheet was created, which included information about the type of material used for the prosthesis and radiographic observations, such as the presence of periapical lesions, marginal discrepancy, bone loss, and the presence of calculus. Additionally, the sheet recorded the status of the adjacent tooth, indicating whether it was sound, missing, carious, or restored.
Prior to conducting the evaluation, the examiners engaged in calibration training. Three observers (LTA, FFA, and FZA) were supervised by SAA and RKA to evaluate the quality of the FPD radiographs in order to improve inter-evaluator reliability. If there was a disagreement, the examiners participated in a collective assessment and discussion of arguments, ultimately reaching a final conclusion. In order to determine the consistency of evaluations within individuals, an additional measurement of 20% of the patients was conducted after a time interval of 2 weeks. Calculations were performed to ascertain the values of the intra-individual Cohen’s kappa, both in its basic and weighted variations. The evaluation of agreement between examiners for both inter- and intra-examiner assessments was performed using Cohen's Kappa statistics, resulting in respective values of 0.89 and 0.93.
The data analysis in this study was conducted using the Statistical Package for Social Sciences version 27 (SPSS, IBM Corp, Armonk, NY, USA). Descriptive statistics was carried out by reporting the number and percent of variables found in teeth adjacent to FPDs. The Chi-Square and Fisher's exact tests were utilized to evaluate the potential correlation between the type of prosthesis and the presence or absence of apical lesions, bone loss, or calculus in adjacent teeth and between type of prosthesis and marginal discrepancy in both single and multi-unit FPDs. The significance level was set at 5% (α= 0.05).
3. RESULTS
The condition of the teeth mesially and distally adjacent to the FPDs is reported in Table 1. Dental caries were found in 138 (15.4%) of the mesial and 136 (15.2%) of the distal neighboring teeth. On the mesial side, there were 228 (25.4%) and 479 (53.3%) sound and restored teeth, respectively, while on the distal side, there were 136 (15.2%) and 408 (45.4%), respectively.
The incidences of calculus, bone loss, and periapical lesions in the teeth adjacent to FPDs are presented in Table 2. While the lack of calculus was more common than its presence, the likelihood of a periapical lesion and bone loss in adjacent teeth was more common both mesially and distally. It is also noteworthy that the distal side had a significantly higher frequency of missing teeth than the mesial side (29.5% and 7.3%, respectively), as reported in Table 2.
| Variables | Frequency | Percent | |
|---|---|---|---|
| Status of mesial adjacent tooth | Carious | 138 | 15.4 |
| Missing | 66 | 7.3 | |
| Restored | 479 | 53.4 | |
| Sound | 215 | 23.9 | |
| Status of distal adjacent tooth | Carious | 100 | 11.1 |
| Missing | 265 | 29.5 | |
| Restored | 408 | 45.5 | |
| Sound | 125 | 13.9 | |
Table 2.
| Variables | Present (N, %)* | Absent (N, %)* | |
|---|---|---|---|
| Status of mesial adjacent tooth | Periapical lesions | 440 (49.0) | 405 (45.1) |
| Bone Loss | 526 (58.6) | 319 (35.5) | |
| Calculus | 261 (29.1) | 581 (64.7) | |
| Status of distal adjacent tooth | Periapical lesions | 348 (38.8) | 296 (33.0) |
| Bone Loss | 399 (44.4) | 245 (27.3) | |
| Calculus | 225 (25.1) | 419 (46.7) | |
The relationship between the type of prosthesis and the occurrence of calculus, bone loss, and periapical lesions in teeth adjacent to FPDs is presented in Table 3. The incidence rate of periapical lesions in single crown restorations was 285 (48.3%) in the mesial neighboring teeth, while in multi-unit FPDs, the incidence rate was 155 (50.3%). For this metric, there were no significant differences between multi-unit FPDs and crowns (p > 0.05). Conversely, for multi-unit FPDs and crowns, the incidence rate of periapical lesions in distal neighboring teeth was 89 (28.9%) and 259 (43.9%), respectively. There was an obvious significant difference in the incidence of periapical lesions according to the type of restorations (p < 0.05). Bone loss in the mesial adjacent teeth of the crowns was reported in 346 teeth (58.6%), whereas the incidence of bone loss was found in 180 teeth (58.4%) for multi-unit FPDs; no significant differences were identified between the two types of prosthesis (p > 0.05). In the distal adjacent teeth, the incidence of bone loss was more common for crowns (294, 49.8%) than multi-unit FPDs (105, 34.1%), which was statically significant (p < 0.05). Calculus accumulation in single and multi-unit FPDs in the mesial neighboring teeth was found in 171 (29.0%) and 90 (29.2%) samples, respectively. There were no significant differences between FPDs and crowns according to prosthesis type (p > 0.05). On the other hand, compared to multi-unit FPDs (54, 17.5%), calculus deposit was more common with crowns (171, 29.0%) in the distal neighboring teeth. The overall increase in calculus accumulation in the distal adjacent teeth was statistically significant (p < 0.05).
| Variables | Type of the Fixed Prosthesis | P-value | |||
|---|---|---|---|---|---|
| Single Crown (N, %) | Multi-unit FPDs (N, %) | ||||
| Mesial adjacent teeth | Periapical lesions | Present | 285 (48.3) | 155 (50.3) | 0.461 |
| Absent | 305 (51.7) | 153 (49.7) | |||
| Bone loss | Present | 346 (58.6) | 180 (58.4) | 0.186 | |
| Absent | 244 (41.4) | 128 (41.6) | |||
| Calculus | Present | 171 (29.0) | 90 (29.2) | 0.358 | |
| Absent | 419 (71.0) | 218 (70.8) | |||
| Distal adjacent teeth | Periapical lesions | Present | 259 (43.9) | 89 (28.9) | <0.001 |
| Absent | 331 (56.1) | 219 (71.1) | |||
| Bone loss | Present | 294 (49.8) | 105 (34.1) | <0.001 | |
| Absent | 296 (50.2) | 203 (65.9) | |||
| Calculus | Present | 171 (29.0) | 54 (17.5) | <0.001 | |
| Absent | 419 (71.0) | 254 (82.5) | |||
| Variables | Ceramic (N, %) | PFM (N, %) | Zirconia (N, %) | P-value | |
|---|---|---|---|---|---|
| Marginal integrity in mesial abutment tooth | Fit margin | 14 (31.1) | 53 (20.7) | 1 (14.3) | 0.012 |
| Open margin | 31 (68.9) | 203 (79.3) | 6 (85.7) | ||
| Marginal integrity in distal abutment tooth | Fit margin | 14 (31.1) | 57 (22.3) | 3 (42.9) | 0.086 |
| Open margin | 31 (68.9) | 119 (77.7) | 4 (57.1) | ||
| Marginal integrity in single crown | Fit margin | 33 (35.9) | 53 (10.8) | 5 (83.3) | < 0.001 |
| Open margin | 59 (64.1) | 438 (89.2) | 1 (16.7) | ||
Table 4 indicates a statistically significant association between the type of prosthetic material and the marginal integrity of mesial abutments for FPDs. For the marginal integrity of mesial abutment teeth, the marginal discrepancy was more common for PFM prostheses (203, 79.3%). The types of prosthetic restoration had a statistically significant correlation with the marginal integrity of mesial abutment teeth (p < 0.05). Similarly, the marginal discrepancy in distal abutment teeth was mainly associated with PFM prostheses (119, 77.7%) and ceramics (31, 68.9%). However, these data were not statistically significant (p > 0.05). In single crowns, the marginal discrepancy was mainly associated with PFM (438, 89.2%) and ceramic-based prostheses (59, 64.1%), and the difference was statistically significant (p < 0.05), as reported in Table 4.
4. DISCUSSION
Studies evaluating treatment outcomes are crucial for obtaining scientific knowledge that guides treatment planning and helps dentists make informed decisions. Thus, the objective of this study was to investigate the marginal quality of FPDs performed by private practitioners in the Ha’il region of Saudi Arabia. Moreover, some complications related to the restorations were considered.
Intraoral radiography has proven to be the most trustworthy technique for confirming the quality of a prosthetic abutment. To obtain correct images, the radiograph must be correctly angled, especially in relation to the film's parallel position. The restoration quality is then evaluated using a two-dimensional picture of a three-dimensional structure. If the X-ray film is positioned in a convex position, anatomical factors specific to each patient, such as the breadth of the dental crest or the curvature of the palate, may result in extra distortion. Notwithstanding these limitations, intraoral radiography is still a useful diagnostic technique in dentistry, especially if a paralleling device is employed to standardize the X-ray device [22].
Establishing an important relationship between dental restorations and the periodontium is crucial for achieving clinical success in terms of both functionality and aesthetics [23, 24]. Plaque deposits, the formation of calculus, and poor oral hygiene are among the variables that contribute to changes in periodontal health. Numerous studies have detailed the role of FPDs in promoting dental plaque accumulation, which poses significant risks for dental caries, apical lesions, bone loss, and periodontitis [25, 26]. Nevertheless, some research has reported that there is no notable disparity in plaque index levels between teeth with FPDs and control teeth [20, 27]. The current investigation found that the occurrence of periapical lesions and bone loss was more prevalent in the majority of the samples examined. According to Padbury et al. [13], the health of periodontal tissue relies on well-developed restorative materials, and Moimaz et al. [28] established a correlation between FPDs and periodontal disorders. According to the study conducted by Ortolan et al. [29], using effective motivational and educational strategies might enhance oral hygiene and maintain the health of the periodontium, even after the insertion of FPDs.
The interdental region is the main location where periodontal disease and caries occur [29]. Regrettably, the interproximal surfaces of the restoration are often overlooked throughout the fabrication process. Food impaction occurs in the interproximal region when there is an inadequate proximal relationship or when the occlusal surface is shaped poorly [30, 31]. Research has also documented irritation of the gum tissue next to teeth restored with FPDs due to the buildup of food on the surface of the artificial teeth [30-32].
Plaque is considered the primary cause of caries and periodontitis [33]. The patient may experience challenges in maintaining proper oral hygiene in an area of a dental prosthesis with or without defective margins or contact points. The initial consequence of food impaction is the experience of indistinct discomfort and pressure, accompanied by inflammation of the gingiva and, eventually, recession. This could then be followed by loss of bone, periapical lesions, and/or caries at the margins of the FPD and adjacent teeth [34]. Research has indicated a substantial correlation between defective contact areas between natural teeth and FPDs and between the presence of caries in neighboring teeth [30, 31]. The findings of the present study confirmed that the presence of an apical lesion, bone loss, and calculus development are more frequently observed in teeth adjacent to FPDs. It is thus imperative to ensure convenient access to the interdental area for effective plaque reduction by instructing patients about dental hygiene practices, with a specific focus on the gingival surface of the pontic replacing a missing tooth, as it is not as accessible for cleaning with a toothbrush [35, 36].
Prior to manufacturing the prosthesis, it is necessary to conduct a comprehensive assessment of the periodontal condition [37]. It is not possible to have a standardized shape for the contact and contour of every tooth. Thus, an examination should take into account the clinical crown length, tissue architecture, contour of adjacent teeth, and the character of the opposing occlusion. To ensure the successful construction of a well-contoured restoration, it is crucial to perform proper tooth preparation, regardless of the restoration plan [38]. Gordon proposed that the reduction in tooth structure along the axis should adhere to the original shape of the tooth, ensuring that the final restoration closely resembles the natural architecture of the unprepared tooth [39].
The current findings corroborate a previous study that demonstrated bone loss in many cases with FPDs [40]. The study conducted by Jernberg et al. examined the effects of open contacts on the periodontium. They found that sites with open contacts had a higher occurrence of food impaction, especially in cases where there were deep pockets and clinical attachment loss. However, there was no significant difference in the gingival index, bleeding, or calculus index between different types of contacts [41]. In a separate cross-sectional study conducted by Koral et al., it was found that patients with an open contact between their prosthesis and neighboring tooth experienced a 2.4% increase in bone loss, which subsequently led to the development of periodontitis [42]. Although there is an indirect correlation between open contacts and periodontal inflammation, these studies suggest that food impaction and improper prosthesis contour have a role in increasing pocket depth and decreasing clinical attachment levels.
Achieving long-term success necessitates the precise marginal fit of indirect restorations. Poorly fitting margins increase the tooth's susceptibility to cement dissolving. When this happens, leakage occurs at the margins, which often leads to secondary caries [43]. Both single and multi-unit FPDs may experience issues with porcelain fractures and marginal discrepancy. Marginal discrepancy may arise due to failure in either clinical- or laboratory-related factors. Clinical failure may result due to inadequately prepared margins or insufficient gingival retraction during the process of recording impressions [43]. Air bubbles present in the impression's periphery or saliva, obscuring proper scanning of a prepared tooth, may also contribute to these inaccuracies. The dental technician must then communicate clearly and concisely regarding the intended contact, contour, and design information. Subsequently, the technician must integrate the essential design requirements to get a favourable restoration. Zahra et al. [44] surveyed dental laboratories to investigate the communication between dentists and dental laboratories regarding FPDs. The findings indicated that technicians frequently expressed dissatisfaction with the information supplied on work authorization forms. All these factors may result in improperly fabricated prostheses at risk of failure.
Inadequate fit of dental restorations, placement of borders sub-gingivally, and over- or under-contoured prostheses can exacerbate periodontal inflammation. In this study, a high frequency of marginal discrepancy was detected in ceramic, PFM, and zirconia single and multi-unit prostheses (Table 4). Vaulderhaug et al. [45] performed a longitudinal study to evaluate the periodontal status of patients with FPDs. It was found that the gingival tissue around teeth with prostheses was frequently inflamed.
There were particular limitations in this study. Evaluating the quality of fixed prosthodontic restorations using two-dimensional images of three-dimensional structures is a difficult task. Due to the cross-sectional design of this study, it was not possible to determine the disease activity or healing, which is a potential restriction. Another constraint is that radiographs were solely evaluated over a defined timeframe, without any subsequent data provided following the completion of fixed prosthodontic restorations. Hence, it was not possible to determine the status of the periapical lesion, whether it was healing or persistent. As a result, these types of research are regarded as having a lower position in the hierarchy of evidence levels compared to longitudinal studies. However, cross-sectional exami- nations are crucial for gathering data as they allow for the examination of the overall health condition, as well as the occurrence of diseases, within a specific population at a given moment. Although the majority of continuous studies investigating the outcomes of endodontic therapy are carried out in academic institutions or teaching hospitals, cross-sectional studies frequently use samples drawn from general practice or community settings. Longitudinal studies provide valuable insights into the potential for a positive outcome, whereas cross-sectional research reveals the current position within the larger community. Analysing data on the current status of a certain disease or the efficacy of treatment in a particular population can serve as a basis for developing intervention strategies and improving healthcare delivery. In addition, employing a cross-sectional design enables the incorporation of a significant number of patients, a task that is difficult to achieve and control in longitudinal studies. Increasing the sample size in studies may help mitigate the influence of interpretation bias. This study was conducted at a single center. However, future research conducted at several centers using sophisticated techniques, such as CBCT, may be able to address the limitations of the current study. Moreover, the resolution of the conventional radiographs employed in this investigation is inferior to that of CBCTs, potentially impacting the outcomes. Additional research on categorizing the predominant factors contributing to complications in fixed restorations would facilitate the identification of patterns that could enhance future educational practices in prosthodontics.
CONCLUSION
Based on the limitations of this investigation, it can be concluded that the complications observed in this study were more frequent compared to previous studies on FPDs. The findings of this research suggest the need for continuous education programs for private practitioners to enhance their knowledge and skills and keep them up-to-date, expectantly improving the technical quality of the restorations provided.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
ABBREVIATION
| FPDs | = Fixed Partial Dentures |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The present work was granted approval by the Research Ethics Committee (REC) at the University of Ha’il, Saudia Arabia with the reference number H-2023-170.
HUMAN AND ANIMAL RIGHTS
This study was conducted in accordance with the guidelines set forth in the Helsinki Declaration of the World Medical Association.
CONSENT FOR PUBLICATION
Due to the retrospective design of the study, the ethics council of the College of Dentistry decided to waive the requirement for informed consent.


