All published articles of this journal are available on ScienceDirect.
Asymptomatic Thyroid Nodule Detection in a Referred Patient, A Case Report
Abstract
Introduction
Thyroid gland abnormalities or enlargement can be easily detected during a routine oral examination. Dental clinical examination involves inspecting and palpating different parts of the head and neck, including the thyroid gland. Referral of patients is crucial for proper patient care.
Case Presentation
In this report, we present the case of a 42-year-old female patient referred to the oral medicine clinic from an orthodontic clinic for the evaluation of tongue pigmentation, during which a thyroid nodule was incidentally detected. The patient was diagnosed with doxycycline-induced tongue pigmentation and was referred for further assessment and management of the thyroid nodule. The patient underwent total thyroidectomy, and the tissue was consistent with that of multiple goiters with no malignancy.
Conclusion
This case highlights the importance of the dentist’s role as a health care provider in detecting any abnormalities presented during the clinical examination and their responsibility to refer the patient to the appropriate medical specialists when needed.
1. INTRODUCTION
Optimal medical care relies strongly on a good doctor‒patient relationship [1]. For patients to express their needs and concerns openly to a physician, they need to trust them first [2]. According to Epstein et al., “Patient-centered communication involves focusing on the patient’s needs, values and wishes” [3]. It is related to improved patient trust and satisfaction [4]. There are many terms in the literature related to ‘concern’ [5]. Addressing patient concerns has been associated with increased patient satisfaction [6]. Physician‒patient communication was confirmed in a systematic review of randomized clinical trials, which analytically studied the positive influence of quality communication on health outcomes [7]. Improving dental treatment outcomes generally involves providing optimum dental care, including a detailed history, comprehensive screening, and proper referral to another specialty.
A study by Guan et al. in 2020 was conducted to examine awareness levels among general dental practitioners and medical practitioners about common oral mucosal diseases. The study investigated screening and referral practices. Fifty percent of the dentists referred patients to oral medicine specialists when they addressed relevant cases, while only 31.6% of the physicians did so. The study concluded that standardized national referral guidelines and continuing professional development courses in oral medicine would improve patient manage- ment [8].
This indicates that patient management will improve after referral to a specialist, particularly for patients with malignant or potentially malignant disease. It can also be helpful when there is a diagnosis in doubt or circum- stances where the clinician or the patient needs a second opinion from a specialist [9].
In an orthodontic treatment course, seeing the patient frequently is an opportunity to address any changes noticed by the patient or the orthodontist and to refer the patient to the proper specialty. Mucosal lesions or masses, tongue pigmentation, and thyroid enlargement are among the many incidents to be detected and referred to the oral medicine clinic.
Thyroid nodules are widespread in the general population, mostly benign [10] and have a prevalence of 70% according to imaging studies and 7% according to palpation [11]. However, studies suggest that approxi- mately 7–15% of thyroid nodules are malignant [12, 13]. Thyroid gland abnormalities or enlargement can be easily detected during a routine oral examination. Dental clinical examination involves inspection and palpation of different parts of the head and neck area. During dental screening, oral health care providers can play an essential role in detecting patients with undiagnosed thyroid disease by taking a detailed medical history, reviewing the body system, and performing thorough head and neck examinations.
Studies have shown that individuals with less frequent or irregular dental visits had more incidence of Head and neck cancers (HNC) and oral cancer than did those who had more regular dental visits [14]. This highlights the importance of dental visits in the early diagnosis of HNC, which can be applied to thyroid nodules detection. The dental practitioner should refer the patient for further evaluation, investigation, and management to avoid a delayed diagnosis of head and neck mass.
In this article, we present the case of a patient who was undergoing orthodontic treatment who expressed her concern about a pigmentation on her tongue that appeared concurrently with recent antibiotic use. The orthodontist referred the patient to an oral medicine specialist, and a large thyroid nodule was detected on head and neck examination. We also investigated the clinical inspection and palpation of the thyroid gland. The patient signed an informed consent as a routine measure in the dental teaching hospital.
2. CASE REPORT
A 42-year-old female patient was referred to the oral medicine clinic from an orthodontic clinic for the evaluation of tongue pigmentation. The patient had been in orthodontic treatment for three years to create space for dental implants. The orthodontist sent a photo and a referral letter explaining the extent and nature of the pigmentation.
Patient’s past medical history revealed gestational diabetes and anemia following bariatric surgery. Moreover, the patient was diagnosed with brucellosis and treated in a hospital setting with doxycycline and rifampicin for six weeks. Approximately one month after medication discontinuation, she started to notice pigmentation on her tongue. Additionally, she denied any concurrent symptoms, and her social and family history were noncontributory.
The patient reported allergy to ibuprofen, during which she developed itching and skin rash and reported food allergies associated with shellfish. The review of the system was unremarkable. She was not on any medication.
Extraoral examination revealed an overweight, well-developed woman with no evidence of lymphadenopathy or salivary gland enlargement; however, thyromegaly was detected on the larger right side than on the left side (Fig. 1). On intraoral examination, Patient had fair to poor oral hygiene with mild gingival recession. She was partially dentate with orthodontic wires. Clinically evident generalized diffuse grayish discoloration of the dorsum of the tongue with normal papillae was observed; no erythema or ulceration was noted (Fig. 2). A more detailed history was taken focused on the presence of thyroid nodules; however, the patient denied noticing thyroid swelling prior to this dental visit and denied any concurrent symptoms. The patient was encouraged to seek immediate medical consultation regarding thyroid gland enlargement.
After ruling out all other causes of pigmentation, she was diagnosed with doxycycline-induced tongue pigmen- tation and subsequently placed on a close follow-up regimen for further evaluation.
The patient underwent ultrasonography (US) with Doppler imaging and computed tomography (CT) of the neck with contrast agent to evaluate the thyroid gland nodule. US revealed heterogeneous nodules containing cystic and solid components in the right thyroidal lobe measuring 4.7 × 3 cm. A small hypoechoic solid nodule abutting the inferior posterior border of the left thyroidal lobe measuring 2.8 × 1.6 cm was observed. A similar nodular zone on the right side measuring 1.1x0.8 cm was observed (Fig. 3). A CT scan showed that the thyroid gland was significantly enlarged bilaterally, with more significant enlargement in the right lobe; additionally, the thyroid gland was occupied by a large nodule composed of dense solid components and well-defined cystic components. Up to 1.1 cm of enlarged lymph nodes were found bilaterally in the upper jugular region level II. The mass caused mild deviation and stenosis of the trachea without signs of invasion. CT of the brain without contrast agent was also performed without evidence of acute brain insult. Final needle aspiration (FNA) was recommended for correlation. FNA revealed a follicular lesion of undetermined significance (Bethesda III) according to the Bethesda System for Reporting Thyroid Cytopathology (TBSRTC). During the investigation, the thyroid tumor increased greatly in size and started to cause breathing difficulty, especially during sleep. Therefore, the patient underwent urgent total thyroidectomy, and surgical histopathology confirmed multiple goiters and was negative for malignancy. The patient is currently receiving thyroid replacement therapy (Levothyroxine 150 micro- grams taken once a day) without complications. The patient is scheduled for follow ups with the endo- crinologist. Ethical approval was waived by the institution as this is a case report. A written informed consent was obtained from the patient before proceeding with the publication of this case report. This paper agrees with the Helsinki declaration principles.

Right thyroid enlargement.
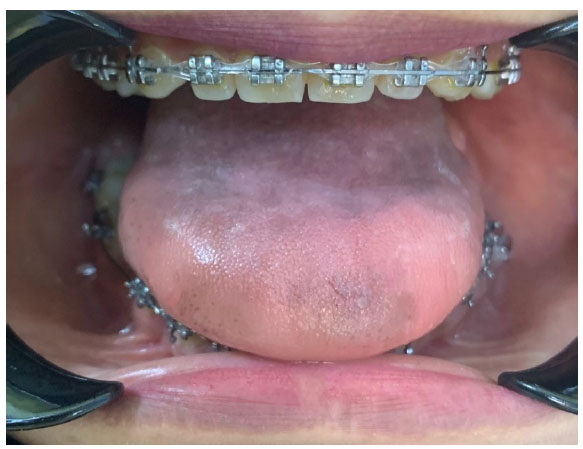
Diffuse greyish pigmentation of the tongue.
3. DISCUSSION
The main aim of this paper is to highlight the importance of an efficient referral system and performing comprehensive clinical examinations during dental screening and how this can affect the early detection of head and mass or tumors. In general, masses in the head and neck area are mostly overlooked, and studies have shown that delays in diagnosis are common [15]. A study by Aslam et al. revealed that providing photographs along with a referral letter can help prioritize new patients for initial consultation, especially in patients with oral cancer [16].
It has been suggested that 7–15% of thyroid nodules are malignant [12, 13]. FNA is the most accurate test used to diagnose thyroid nodules when suspected [17]. The Bethesda System for Reporting Thyroid Cytopathology (TBSRTC) has been used to classify thyroid nodules into six categories based on malignancy (I- IV) using FNA findings [12]. The medical management of lesions in category III usually ranges from observation to surgery, and lobectomy or total thyroidectomy is used [12]. In this case, the surgical team elected to perform total thyroidectomy and place the patient on thyroid replacement therapy. A progressive enlargement of the nodule led to partial airway obstruction, and the patient started to complain of more significant breathing difficulties. Although the rapid growth of a thyroid nodule may indicate aggressive cancer or malignancy [13], the nodule was benign according to histopathology. Generally, thyroid US is indicated when nodules are found. Furthermore, multiple nodule characteristics, such as solid or predominantly solid nodules, taller-than-wide dimensions, hypoechogenicity, irregular margins, micro- calcifications, absent halo, and increased vascularity, can indicate the presence of malignancy and warrant further investigation [13, 18]. In this case, US showed signs of hypoechoic solid nodularity along with a rapid increase in size, for which CT of the neck was performed with a contrast agent to confirm the diagnosis which was benign in this case.
Overall, we emphasize the importance of performing a thorough, comprehensive head and neck examination during dental screening, which greatly helped in the early detection of thyroid nodules in this patient. There are useful data in the literature focusing on the evaluation of head and neck masses, including thyroid tumors, and advocating for early diagnosis [15]. The limitation of this case report was noted in that the patient was treated in a different hospital facility which hindered the oral medicine specialist access to diagnostic data and patient follow up with the treating team.
The following section will elaborate more on the basic steps in thyroid gland examination performed during dental and head and neck screening.
3.1. Thyroid Gland Examination
The thyroid gland is examined through inspection first and then palpation while the patient is standing in front of or behind the parotid gland.
Inspection: while the patient’s head was tilted to the side, the neck was exposed. The gland should be viewed from the front and side of the patient. Any change in thyroid shape, size, or texture and the presence of visible nodularity should be evaluated and recorded [11].
For palpation, the thyroid isthmus was located with the palms of the fingers. However, sometimes it is impalpable unless enlarged. To do so, the laryngeal prominence of the thyroid cartilage should be identified first. Fingers should slide inferiorly to find the cricoid cartilage, marking the location of the superior border of the thyroid isthmus. Asking the patient to swallow will cause the isthmus to move under the fingers, confirming the structure. Once identified, the fingers should slide laterally along the isthmus and along the contour of the trachea. The thyroid gland should now be trapped between the fingers and the trachea. Swallowing will cause the thyroid gland to move in an upward direction, which will confirm that this moving structure is the thyroid gland. If the structure noted does not move, it may represent a lymph node, a fixed thyroid malignancy, a prominent neck muscle, or some other neck structure [11]. Any symmetry, size change, or mass should be noted and documented for both lobes of the thyroid. In cases of surgical resection, gland atrophy from levothyroxine therapy, or a naturally small gland, the thyroid glands may not be palpable [11].
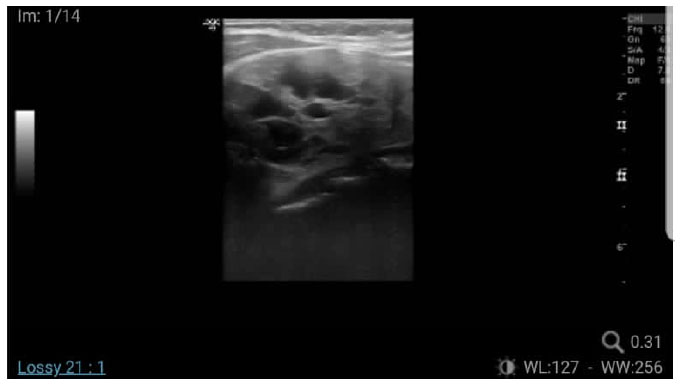
Right gland ultrasound showing heterogenous nodules contain cystic and solid component at the right thyroidal lobe.
CONCLUSION
Head and neck tumors and masses are common in the general population. Dentists play a crucial role as health care providers in detecting any abnormalities present during the examination and should take responsibility for referring the patient to the appropriate medical specialty. This can be achieved by implementing curricula in the field of oral medicine among dentistry and medical students and supporting continuing education among healthcare providers to reduce diagnostic delay for oral diseases [19, 20].
AUTHOR'S CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| HNC | = Head and Neck Cancers |
| CT | = Computed Tomography |
| US | = Ultrasonography |
CONSENT FOR PUBLICATION
A written informed consent was obtained from the patient before proceeding with the publication of this case report.


