All published articles of this journal are available on ScienceDirect.
Endodontic Surgery and Post-Treatment Apical Periodontitis: A Systematic Review
Abstract
Background
It has been demonstrated that using innovative root-end filling materials speeds up the success of Endodontic Microsurgery (EMS) on teeth having root filling but still suffering from posttreatment Apical Periodontitis (AP). However, this has reopened the discussion about the long-term effectiveness of EMS conducted on such teeth.
Objectives
This study aimsto assess the long-term clinical and radiographic outcomes of endodontic surgical procedures in molars with radiographic evidence of secondary AP.
Methodology
A literature review was undertaken utilizing different databases, including MEDLINE (through PubMed), EMBASE, and Web of Science. The terms used for the search were ‘endodontic microsurgery,’ ‘apical microsurgery,’ ‘periapical disorders,’ ‘root canal therapy,’ ‘apicoectomy,’ ‘retreatment,’ ‘treatment result,’ “retrograde obturation,” and ‘success rate.’ In order to choose the most reliable longitudinal data, specific inclusion and exclusion criteria were established in advance. Only studies that met inclusion criteria for clinical and radiographic outcomes were considered, including prospective clinical studies and randomized clinical trials with at least two-year follow-ups.
Results
The study of the databases yielded 561 articles in total. From the 115 articles with full texts available, unrelated articles (105) were removed. Our inclusion criteria were met by an overall of ten studies (six prospective clinical studies and four randomized clinical trials). With intervals for follow-up ranging from two to thirteen years, a pooled success rate of 91% from all 451 treated teeth included in the randomized clinical trials and a pooled success rate of 79% from a total of 839 encompassed teeth in the prospective clinical studies were observed. During the same length of time of observation, survival rates ranged from 78% to 100%. Smoking status, tooth position and type, the presence or absence of dentinal abnormalities, the thickness of the bone between the teeth (interproximal bone), and the substance used to fill the space at the end of the roots are the five predictive variables revealed.
Conclusion
When EMS is performed by skilled endodontists who can deliver high success rates and reliable results, teeth afflicted by secondary AP have a good prognosis and can be preserved.
1. INTRODUCTION
Root canal therapy is a procedure that aims to clean and shape the root canal system in all three dimensions, sealing it to prevent reinfection [1, 2]. The success rate of this therapy is high and generally predictable [3-6], although failures can still happen. Recent studies [3, 7] indicate that approximately 14-16% of initial root canal treatments may fail. The failure of endodontic treatment can be attributed to various factors, both intra-radicular and extra-radicular. Intra-radicular factors, such as persistent infection in the root canals, dentinal tubules, or complex abnormalities in the root canal system, are considered significant contributors to endodontic failure [8-11]. On the other hand, extra-radicular causes of endodontic failure include periapical actinomycosis resulting from extruded endodontic material [12, 13], the accumulation of endogenous cholesterol crystals in apical tissues [14, 15], and the presence of unresolved cystic lesions [16, 17]. Assuming the tooth is restorable, the gingiva is healthy, and the patient desires to save the tooth, non-surgical retreatment or endodontic surgery may be utilized to preserve teeth that have previously undergone treatment and have developed persistent periapical lesion(s). Following the decision to attempt to save the tooth, the dentist and patient are confronted with the challenging task of determining the optimal course of action to achieve the best possible long-term outcomes. It is the responsibility of the treating dentist to provide patients with the most current and accurate information regarding the potential outcomes of their treatment options. The recommendations of the dentist are often followed by the patient [18]. In spite of this, it appears that dental specialists are not always in agreement when making decisions about retreatment or endodontic surgery [19-22].
The success of Endodontic Microsurgery (EMS) may depend on a variety of factors, including the surgical procedure, the instruments utilized, the surgeon's medical and radiographic evaluation, the patient's socioeconomic status and overall health, the number and location of the affected teeth, the results of any previous root canal therapy or retreatment, and the type of coronal restorations. Due to the differences in these characteristics and treatment success and failure rates between studies, it is difficult to make direct comparisons between the numerous studies on this topic [9, 17]. In order to reduce the considerable difference in reported results [1], it is crucial to overcome the diversity of data about the outlook of EMS [1] by categorizing the research according to the standard of their methods [18]. Additionally, this evaluation was developed with the goal of producing a more reliable outcome result by looking for examiners with a high level of outside validity of the information, particularly in relation to the follow-up period under consideration and the environments in which EMS was conducted. By doing this, we anticipate being able to overcome some of the weaknesses of earlier assessments of the short-term effects of EMS [19-21] and offer more reliable and useful information for use in a clinical context similar to private practice. According to a meta-analysis and systematic review conducted by Kang et al. [20], which compared the clinical and radiographic outcomes of non-surgical dental retreatment with Electronic Migration of Subgingival microorganisms (EMS), the overall pooled success rate for EMS was reported to be 92%. However, this evaluation included trials with as few as 20 teeth [20], which may not have been sufficient to produce clinically significant results [18]. Furthermore, Seltzer et al.'s thorough review and meta-analysis [21] revealed that ambulance services had a 94% success rate in managing apical periodontitis. However, this conclusion was based on studies with a minimum of a 6-month follow-up [22]. Although they only provided a short-term (2-year) follow-up, several studies from the previous 20 years [23-28] have reported on the outcome of EMS. Short-term monitoring may lead to inaccurate prognoses, as up to 25% of teeth believed to have healed in the short term have been found to reverse healing upon review 3 years or more after EMS [7, 29-31]. Additionally, a distinct portion of cases labeled as “uncertain recovery” at the 1-year follow-up are ultimately diagnosed as “full healing” when observed at the 5-year mark [7, 31, 32]. The shell-end filling material influences this. It is crucial to thoroughly assess the validity of the data pertaining to the long-term well-being and survival of molars treated with EMS in order to address the existing knowledge gap. Undertaking a comprehensive review of pertinent studies is necessary in order to provide treatment providers with reliable information and a solid justification when discussing various treatment options with patients. Evidence on the long-term outcomes of EMS is essential [7], as it will enable treatment providers to make informed decisions about the most effective course of action for their patients. Additionally, the inclusion of these additional clinical data will enhance the identification of prognostic markers and strengthen the link between these results and patient-centered outcomes. This extensive investigation and meta-analysis aims to evaluate the clinical and radiological long-term effects of endodontic surgical procedures in teeth diagnosed with secondary AP through radiographic assessment.
2. MATERIALS AND METHODS
Prior to conducting the literature search, the evidence-based PICO question framework was used. The problem was presented as a question in the following way: What are the long-term clinical and radiographic outcomes of endodontic surgical procedures in molars with radiographic evidence of secondary apical periodontitis using different root end-filling materials??
To preserve the study's codified organization, this review adheres to the Recommended Reporting Items over Systematic Reviews as well as Meta-analysis (PRISMA) 2020 Statement.
MEDLINE (through PubMed), EMBASE, and Web of Science were among the search databases used. The search phrases utilized were “retrograde obturation,” “treatment results,” “endodontic microsurgery,” “apical microsurgery,” “periapical disorders,” “root canal therapy,” and “apicoectomy.” Additional searches were conducted in the reference lists of pertinent studies as well as literature reviews addressing the interest-generating topic.
The inclusion criteria considered were: a) studies on living persons; b) articles published between January 2000 and December 2020; c) Randomized Controlled Trials (RCTs) focusing on emergency medical services; d) Prospective Clinical Studies (PCS); e) minimum of 2 years of follow-up; f) emergency-related dental care-indicating teeth (initial endodontic therapy, periapical lesion, subsequent apical periodontitis, or chronic extra-radicular infection can all cause the ejection of root canal filling material); g) magnification tools and ultrasonic root-end preparation was used in the treatment method to achieve a new approach; and h) indicators of clinical and radiological success that have been established, defined by Rud et al. [13] and Molven et al. [14].
The exclusion criteria considered were: a) studies involving patients younger than 18 years of age; b) retrospective clinical studies, case series, and review of EMS; c) studies using tooth samples with root resection, amputation, perforation, or fractures; d) incomplete or insufficient methodology; and e) no information on the success rate of EMS.
2.1. Study Selection
Mendeley Desktop 1.19.4 was used to import and sort through all research that was uncovered by the various search methods. Titles and abstracts were evaluated by two reviewers (first and second authors) to determine whether the papers were suitable for inclusion. A third impartial reviewer/author was consulted in the event of disagreement. All three reviewers are endodontic specialists with extensive experience in the field. Following this initial evaluation, the full-text versions of the chosen records were reviewed by two additional reviewers (4th and 5th authors) to determine whether or not they should be included in the review. Another writer was consulted in the event of disagreement. The same two reviewers also extracted the data into a standard data format.
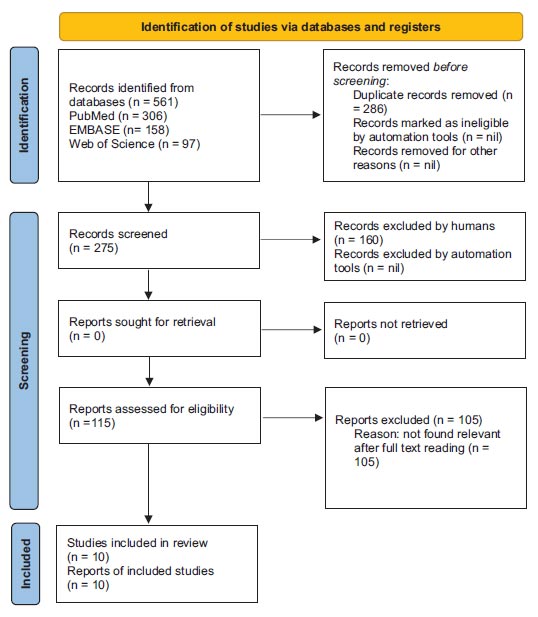
The PRISMA process diagram (Fig. 1) was employed to present the publications that met the eligibility requirements and those that were disqualified from consideration for the research.
2.2. Data Extraction
The following sections of an Excel table with the following headings were created during the data extraction process: research type, representative samples, number of true surgery or orthonormal processing cases, medical and imaging success criteria, recall rate, monitoring period, technique and substances used, main results, limitations, as well as conclusion.
2.3. Quality Assessment
Two instruments were utilized to assess the risk of bias, both obtained from the Cochrane database. The “Risk of bias tool for randomized trials” (RoB2) approach instrument (version 2 of the Randomized risk-of-bias tool for randomized experiments; web address.riskofbias.info) was used to evaluate RCTs [33], whereas the “Risk of bias in non-randomized studies - of Interventions” (ROBINS-I) instrument was used to evaluate non-RCTs [34]. Two separate authors conducted the evaluations (4th and 5th authors).
2.4. Meta-analysis
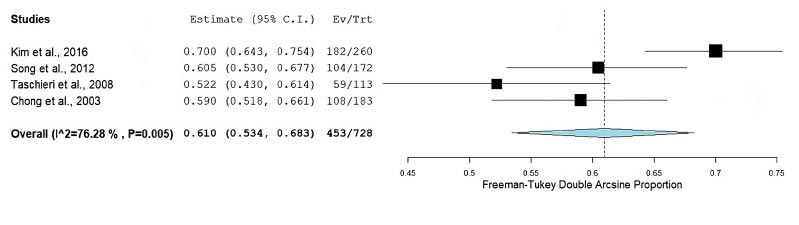
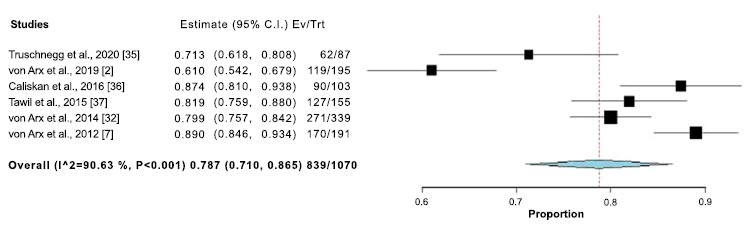
A quantitative meta-analysis of proportions across several papers was conducted using OpenMeta [analyst] and the Freeman-Tukey triple arcsine transformation [35]. To statistically examine the degree of heterogeneity present, the standard chi-square and I2 tests were utilized. Only when moderate to substantial heterogeneity (I2>50%) was present were statistical tests conducted with random-effects models; otherwise, fixed-effects models were used [36]. The results were given a narrative form when statistical pooling was not possible.
3. RESULTS
Using the search method outlined in the “Materials and Methods” section, 561 articles were found after the databases were analyzed. From the 115 articles with full text available, unrelated articles (105) were removed. The papers were excluded mostly due to a lack of a proper research design (34 articles) and a lack of sufficient follow-up time (71 articles).
Data extraction, methodological quality assessment, data synthesis, and analysis were conducted that met all inclusion criteria following full-text evaluation. Table 1 provides a summary of the studies that were considered for this review and their success rates.
| Authors/Refs | Study Design | Number of Teeth | Follow Up (years) | Material Used for Root End Filling | Rate of Recall (%) | Percentage of Successful Root-end Fillings | Rate of Success | Rate of Survival |
|---|---|---|---|---|---|---|---|---|
| von Arx et al. 2019 [2] | PCS | 195 | 10 | ProRoot® MTA grey (n = 44)/ ProRoot® MTA white (n = 75) |
61% (119/ 195) |
ProRoot® MTA grey 84% (37/44)/ProRoot® MTA white 80% (60/75) |
82% (97/ 119) |
88% |
| Truschnegg et al. 2020 [37] | PCS | 87 | 10 | IRM | 70% (61/ 87) |
NA | 77% (47/61) |
79% |
| Caliskan et al. 2016 [38] | PCS | 103 | 11 – 12 | ProRoot® MTA grey (n =)/ ProRoot® MTA white (n = 59) |
87% (90/ 103 |
ProRoot® MTA grey 84% (37/44)/ProRoot® MTA white |
72% (65/ 90) |
82% |
| Tawil et al. 2015 [39] | PCS | 156 | 7 – 12 | ProRoot® MTA grey (n = 87)/ ProRoot® MTA white (n = 69) |
82% (127/ 156 |
NA | 88% (112/ 127) |
90% |
| von Arx et al. 2014 [32] | PCS | 339 | 5 – 10 | ProRoot® MTA grey (n = 103)/ ProRoot® MTA white (n = 69) |
80% (270/ 339) |
ProRoot® MTA grey 90% (69/103)/ProRoot® MTA white |
86% (232/ 270) |
98% |
| Taschieri et al. 2008 [9] | RCT | 193 | 6 – 8 | ProRoot® MTA grey (n = 26)/ ProRoot® MTA white (n = 97) |
89% (171/ 193) |
ProRoot® MTA grey 78% (26/97)/ProRoot® MTA white |
83% (141/ 171) |
76% |
| Chong et al. 2003 [40] | RCT | 113 | 5 – 9 | ProRoot® MTA grey (n = 64)/ ProRoot® MTA white (n = 49) |
95% (108/ 113) |
NA | 84% (90/ 108) |
80% |
| Kim et al. 2016 [11] | RCT | 259 | 2 – 6 | ProRoot® MTA grey (n = 133)/ ProRoot® MTA white (n = 126) |
69% (181/ 259) |
ProRoot® MTA grey 53% (96/181)/ProRoot® MTA white |
90% (163/ 181) |
82% |
| Song et al. 2012 [41] | RCT | 170 | 7 – 9 | ProRoot® MTA grey (n = 100)/ ProRoot® MTA white (n = 70) |
60% (101/ 170) |
NA | 92% (93/ 101) |
99% |
| von Arx et al. 2012 [7] | PCS | 189 | 6 | Pro Root® MTA (n = 90)/IRM (n = 99) | (85%161/ 189) |
ProRoot® MTA (48%)/IRM (51%) | 77% (124/ 161) |
90% |
Out of the ten studies considered, four studies regarding Randomized Clinical Trials (RCT) [9, 11, 40, 41] and six studies regarding Prospective clinical studies [2, 7, 32, 37-39] were chosen. The research examining treated teeth has reported sample sizes ranging from 87 to 339 [32, 37], with studies employing follow-up times of either two years [9, 38, 40] or ten to thirteen years [37]. Mineral Trioxide Aggregate (MTA) [2, 7, 11, 32, 38-40] and Super Ethoxybenzoic Acid (SuperEBA) cement [7, 32] are two examples of root-end filling materials that have been investigated in this context. The results of these studies have yielded recall rates that range from 59% [40] to 89% [9]. The research methodology devised by Rud et al. [13] and Molven et al. [14] was used in all studies [2, 7, 9, 11, 32, 37-40] to evaluate outcomes. The success rate varied from 69% [39] to 93% [41]. In each study, a comprehensive analysis was conducted to assess the impact of various factors on EMS outcomes (Table 2). The evaluation included patient-specific variables such as age, sex, smoking status, and drinking habits [2, 7, 32, 37-39, 41], as well as tooth-related variables including medical signs/symptoms [7], tooth location, type, prior nonsurgical or surgical endodontic treatments, size, and histopathology of periapical tissue [38]. Other factors evaluated included the presence or absence of a post and the existing root canal filling [11, 32, 37-39, 41]. Overall, these studies aimed to identify the factors that can influence a patient's treatment outcome and provide valuable insights for future research and clinical practice. Upon analyzing the outcomes of five clinical trials, it was discovered that five distinct predictive variables exhibited statistically significant disparities. Contrarily, the success rate among non-smokers was reported to be 78%, whereas the success rate for smokers was found to be 33.3%, as per Truschnegg et al.’s study in 2020 [37]. In one of the limited studies that assessed the influence of root dentinal anomalies on the efficacy of EMS, it was found that the success rate for teeth exhibiting dentinal irregularities was merely 31.5%, as opposed to 98% for teeth presenting with a complete set of dentition which was discovered in the by Tawil et al., in 2015 [39]. According to von Arx et al. (2019) [2], the success rate for maxillary molars was higher (95.2%) than that of maxillary premolars (66.7%) when the tooth component was evaluated, whereas no statistically significant difference in this respect was found in any of the other researches [7, 9, 11, 32, 37-40]. The success rates were greater when the bone levels were less than 3 mm beyond the junction of cement and enamel or the edge of the tooth being repaired, according to Von Arx et al. in 2012 [7], who reported a significant difference in the mesial and distant interproximal bone levels. According to Von Arx et al’s study in 2014 [32], MTA was more successful than dentine-bonded adhesive resins as a root-end filling material. The same researcher also discovered statistically significant variations between the SuperEBA group (67.3% effectiveness rate) and the MTA team (86.4% success rate) in a second experiment [7], with the MTR group having a greater success rate. According to the findings by Kim et al. (2016) [11] or Tawil et al. (2015) [39], the usage of MTA and SuperEBA had no discernible impact on the results.
The results of five separate studies indicated 100% survival rates for the duration of 2-10 years of follow-up, as opposed to a study that recorded a 79% survival rate after thirteen years of monitoring. This finding was backed by data from one research study [9, 37-41]. The RoB2 method, recommended by Cochrane [33], was used to evaluate the risk of bias in each of the four RCTs. Although concerns were raised in the research conducted by Song et al. [41], the overall risk of bias was found to be relatively low in all three studies [9, 11, 40].
| Authors/Refs | Design of Study | Methods | Evaluated Parameters | Followup Years(Years) | No. Teeth | No of Healed Teeth | No of Non-healed Teeth | Rate of Recall (%) |
|---|---|---|---|---|---|---|---|---|
| von Arx et al. 2019 [2] | PCS | ProRoot® MTA Grey or ProRoot® MTA White | 1. Age 2. Sex 3. Use of alcohol and tobacco 4. Location of the tooth; 5. Previous endodontic treatment 6. The size of the lesion before and after surgery 7. Antibiotics used during surgery |
10 | 195 | 97 | 22 | 82% |
| Truschnegg et al. 2020 [35] |
PCS | IRM | 1. Age 2. Sex 3. Alcohol and tobacco use 4. The position of the tooth 5. Previous endodontic treatment 6. Lesion size before and after surgery 7. Antibiotics given before surgery |
10 | 87 | 47 | 14 | 77% |
| Caliskan et al. 2016 [36] | PCS | ProRoot® MTA | 1. Sex 2. Age 3. The kind and position of teeth 4. The capping quality of the root canal 5. Whether there is a post or not 6. Previous root canal therapy or retreatment 7. Previous endodontic surgery or non-surgical therapy 8. The dimensions and histology of periapical lesions 9. Antibiotic treatment 10. Heal |
11-12 | 103 | 65 | 25 | 86% |
| Tawil et al. 2015 [37] | PCS | Grey ProRoot MTA or SuperEBA | 1. Age 2. Gender 3. Location of the tooth 4. Dentinal defect present versus absent 5. Super EBA vs. MTA: Root-end Filling Material |
7-12 | 156 | 112 | 15 | 82% |
| von Arx et al. 2014 [32] | PCS | Composite of dentin-bonded adhesive resin | 1. Material type 2. Sex 3. Age 4. Type of tooth (mandibular anterior, premolar, and molar versus maxillary anterior, premolar, and molar) 5. The presence or lack of a screw or post 6. The nature of the procedure (original or follow-up). |
5-10 | 339 | 232 | 38 | 78% |
| Taschieri et al. 2008 [9] | RCT | EBA Super | 1. The type of magnifying instrument 2. Location of tooth |
6-8 | 193 | 141 | 30 | 73% |
| Chong et al. 2003 [39] | RCT | MTA and IRM | 1. Material type | 5-9 | 113 | 90 | 18 | 72% |
| Kim et al. 2016 [11] |
RCT | Super EBA, ProRoot® MTA | 1. Material type | 2-6 | 259 | 163 | 18 | 84% |
| Song et al. 2012 [38] | RCT | Super EBA, IRM, and ProRoot® MTA | 1. Age 2. Sex 3. Type of tooth 4. Location of tooth 5. Type of lesion 6. Material kind |
7-9 | 170 | 93 | 8 | 78% |
| von Arx et al. 2012 [7] | PCS | Pro Root® MTA and IRM | 1. Sex 2. Age 3. Smoking 4. Pain 5. Signs and symptoms 6. Root canal filling 7. Root canal filling material |
6 | 189 | 124 | 37 | 85% |
| Authors/Refs. | Bias Brought Induced by Confusing | Bias in the Study's Participant Selection Process | Classification of Interventions with Bias | Bias Brought Induced by Deviations from the Anticipated Course of Action | Data Missing Bias | Bias in Outcome Measurement | Bias in the Stated Result's Selection |
|---|---|---|---|---|---|---|---|
| Truschnegg et al. 2020 [35] | Average | Minimum | Minimum | Minimum | Minimum | Minimum | Minimum |
| von Arx et al. 2019 [2] | Minimum | Minimum | Minimum | Minimum | Minimum | Minimum | Minimum |
| Caliskan et al. 2016 [36] | Average | Minimum | Minimum | Minimum | Minimum | Average | Minimum |
| Tawil et al., 2015 [37] | Minimum | Minimum | Minimum | Minimum | Minimum | Average | Average |
| von Arx et al., 2014 [32] | Minimum | Minimum | Minimum | Minimum | Minimum | Average | Minimum |
| von Arx et al., 2012 [7] | Minimum | Minimum | Minimum | Minimum | Minimum | Minimum | Minimum |
ROBINS-I instrument, as proposed by Cochrane [34], was used to assess the quality of the remaining six PCSs. An overview of the results is shown in Table 3. The studies discovered that the likelihood of bias prior to the intervention was negligible. Throughout each of the trials, there existed a scant risk of bias during the execution of the interventions. After the intervention, the research demonstrated a variable degree of bias, especially with regard to evaluating the success of the interventions discovered.
4. RESULTS AND DISCUSSION
The primary objective of evaluating the outcome of endodontic therapy is to monitor the healing or improvement of apical periodontitis [42]. According to the results of this study, EMS had a pooled success rate of 78% in PCS [2, 7, 32, 37-39] and 91% in the included RCTs [9, 11, 40, 41] between 2 and 13 years following the intervention. In the studies that were included in the analysis, there was a 24% difference in the rates of EMS success between the highest and lowest levels of clinical and radiographic recovery. The objective pursued by Tawil et al. in 2015 [39] was to evaluate the outcomes of surgical periapical healing in roots with dentinal irregularities in comparison to roots without such imperfections by employing transillumination as a diagnostic method. Given the lower success rates observed in this set of teeth compared to others, we opted to include them in our study of root dentinal abnormalities. Unfortunately, the authors classified instances of only partial healing as non-recovered cases, which had a negative impact on the overall success rate. This decision led to a significant decrease in the overall success rate, as confirmed by our findings. The study by Song et al. in 2011 [41] may have underestimated results due to the fact that they only provided data for teeth that had been deemed healed at the initial visit, which ranged from slightly over one to five years of follow-up [43]. This accounts for 39.5% of the overall true recall rate instead of the initially reported 60.5%. In this research, the combined recall rate for RCTs was 61%, which suggests that a substantial portion of the initial cohort was unable to be contacted for further evaluation. As a result, the outcomes may be subject to bias. The following variables were examined as potential prognostic factors: smoking history [37], tooth type and location [2], the presence or absence of a dentinal hole [39], interproximal bone thickness [7], and root-end filling material [7, 32]. These were the only variables that exhibited statistically significant variations in relation to the EMS outcome. The impact of the root-end filling material was the primary focus of the majority of the studies conducted, making it a common intraoperative variable to examine. It is worth noting that no research utilized amalgam, as it is no longer used in contemporary endodontic practice due to its potential drawbacks [44].
The reports reviewed did not mention gutta-percha or glass ionomer cement as potential treatment options for EMS. Zinc Oxide Eugenol (ZOE), Intermediate Restorative Cement (IRM) [37, 40, 41], SuperEBA [7, 9, 11, 39, 41], resin-based cements [7, 32], and MTA [2, 7, 11, 32, 38-41] were the root-end filling materials utilized to evaluate the treatment outcomes in the current review. To create ZOE, powdered zinc oxide is combined with liquid eugenol. The development of IRM and SuperEBA, which are ZOE-based materials with improved mechanical properties and do not contain eugenol, serves as an example of modifications made to enhance their characteristics. Certain issues have emerged with these cements, including tissue irritation, vulnerability to moisture [41], elevated solubility, and problematic handling characteristics [44]. If the filling powder-to-liquid ratio is inadequate, the presence of air bubbles may result, leading to a reduction in size and, conceivably, microleakage [41]. Resin-based Composite root-end fillings have been employed by Truschnegg et al. in 2020 [37], Chong et al. in 2003 [40], and Song et al. in2012 [41]. The success rate was greater in the MTA group, but there was no statistically significant difference between the groups in the sole research comparing resin-based composite material and other materials for EMS outcomes. SuperEBA was utilized as a retrograde filling material in a number of researches published between 2008 and 2016; examples include those by Von Arx et al. [7], Taschieri et al. [9], Kim et al. [11], Tawil et al. [39], and Song et al. [41]. It was only by comparing the MTA group to the SuperEBA group that a statistically significant difference was seen (86.4% vs. 67.3%) [7]. In this study, a dentine bonding agent was used in two different ways to assess the efficacy of EMS [7, 32]. For the root-end filling, this material is statistically inferior to MTA. However, a single study [32] discovered a much smaller difference. Moisture management of such materials is necessary for the EMS method [44], while proper isolation of the operating field is required for the use of dentin bonding agents [21].
The quality of RCTs and PCSs is evaluated using the risk of bias. Across the board, the risk of bias was minimal or absent except for the study conducted by Song et al. [41]. We are particularly concerned about the potential for bias introduced by missing data. In certain studies, missing teeth were taken into account in the statistical analysis [2, 9, 38]. Although some publications do not consider having teeth extracted during the follow-up period for reasons unrelated to EMS (such as fracture or prosthetics) as a drop-out [7, 11, 32], others do. Given the significance of avoiding tooth loss, it would be irresponsible to conceal this information as it could lead to an overestimation of the likelihood of a successful outcome in EMS treatments, regardless of the reason for the extraction. Furthermore, it is crucial to consider the potential for error when evaluating the results. Several research projects [2, 7, 9, 11, 32, 37-41] have utilized the technique of employing independent observers. Some of these studies [7, 9] withheld information from one or both of the observers, while others [2, 7, 9, 11, 38-41] compared the findings of the researchers. The radiographic results were classified based on the criteria established by Rud et al. [13] and Molven et al. [14]. It is worth noting that the categorization of incompletely healed patients as non-healed in a single study [39] raises questions about the validity of this aspect of the risk of bias assessment. This, coupled with the potential for an incorrect EMS result, suggests that further investigation is warranted.
The first calcium-silicate reinforced materials used in dental were produced in the late twentieth century [44]. After experiencing difficulties with the first generation, including the induction of discoloration [45, 46], extended setting time, and delayed hydration [47, 48], zirconium oxide was utilized in place of bismuth oxide in the second generation's biodentine. The exceptional biocompatibility [49] of these materials has garnered significant attention. In the majority of the studies reviewed [2, 7, 11, 32, 38-41], calcium silicate-based materials were used for root-end fillings. Success rates reported by MTA were higher than those reported by SuperEBA [7] or dentine-bonded adhesive resin-based material [32]. The s consistency of MTA after being combined with sterile water might make it difficult to handle and effectively place as a root-end filling material; its extended setting time (2 hours and 45 minutes) can lead to dislodgement [44].
The time frame for evaluating the success of endodontic microsurgery remains a topic of ongoing debate [1]. Establishing an informed therapeutic decision and predicting the long-term health of treated teeth requires resolving this issue [41]. It is recommended by the European Society of Endodontology that patients be clinically and radiographically monitored at regular intervals for at least a year following treatment.
In certain instances, a longer period of time may be necessary to achieve full recovery, such as when a radiolucent area, commonly referred to as a “surgical defect” or “scar,” persists beyond one year following a surgical endodontic procedure [42]. To ensure accurate and reliable outcomes, it is advised to wait at least one year after treatment completion before conducting outcome analyses, as recommended by the American Association of Endodontists [50].
Certain investigations [7, 38] indicate that setbacks that have been resolved over an extended period of time can serve to prevent regressions. It is recommended that individuals who exhibit questionable healing after one year continue to be closely monitored, and the type of material used at the root end should be taken into account, even though previous discussions suggest that a year of monitoring may be sufficient to assess the long-term outcome. In contrast to cross-sectional studies, longitudinal studies offer more dependable, patient-focused outcomes through the provision of survival rate data and a more comprehensive understanding of long-term failure causes, including root fractures [2], factors related to prosthodontics [7], endodontics [37], and fractures or dental caries [11]. In this review, we utilized stringent criteria for selection and elimination to minimize variations between studies and generate the most dependable results possible. In contrast to Tsesis et al. [19], we excluded studies that involved surgery conducted without the assistance of an endoscope or microscope. Additionally, we did not consider RCTs as a study design, unlike prior assessments [20, 21]. It is important to note that the results of this study can be compared to those of other research, as they all utilize the same radiographic outcome classification [13, 14].
Recent studies have examined the effects of EMS treatment at various time points to determine if there are any statistically significant differences. The results demonstrated that the success rates after 1 year (91.6%) and 5 years (91.4%) were significantly higher than those after 10 years (81.5%). According to the research by von Arx et al. [2], these differences were not found to be statistically significant during the one-year or five-year follow-up periods.
Although Kim et al. [11] did not detect a statistically significant difference between the 1- and 4-year follow-up periods, they observed a minor decrease (4.8% overall) in the latter. The researchers found that this pattern arose due to a decline in the memory rate of the successful group from the initial 1-year follow-up to the subsequent 4-year follow-up. EMS was followed by two trials, which provided valuable data for researchers one year later [39, 40]. In terms of predictive value, the MTA group (96.7%) outperformed the dentine-bonded adhesive resin group (90.7%). Additionally, 93.9% of patients who were classified as healed after 1 year remained so after 5 years, according to a study by von Arx et al. [32]. However, the long-term predictability of the questionable healing categorization appears to be the lowest when evaluated at short follow-up intervals, as reported in studies by Arx and others [36, 51].
This study has some limitations that should be considered. To begin with, only long-term follow-up studies were included, which may have reduced the quality of some studies due to the higher dropout rate that is commonly associated with longer follow-up periods [4, 41]. Additionally, there is a need for standardized reporting guidelines for outcomes specific to EMS investigations, as the research criteria varied, making it difficult to evaluate the data objectively. Several prior efforts [52-54] aimed at comparing the outcomes of 2D and 3D assessments have been unsuccessful due to methodological shortcomings such as insufficient follow-up, retrospective study design, or varying clinical and radiographic criteria. In order to gain a better comprehension of the characteristics of periapical lesions detected through 2D and 3D radiography, Kruse et al. [18] conducted a study to evaluate their diagnostic accuracy. In comparison to 3D assessments, 2D radiographs have been demonstrated to overemphasize the process of healing [23, 52]. The results of the histological examination revealed that approximately 40% of individuals who were misdiagnosed by CBCT showed no signs of periapical inflammation. It is essential to exercise caution when using CBCT, as it may misinterpret the presence of disease as “scar tissue healing” (incomplete healing). The European Society of Endodontology recommends that CBCT should only be used in place of traditional imaging when the benefits of CBCT outweigh those of traditional imaging [55]. Currently, there is no established healing evaluation system based on CBCT, and thus, it is advisable to follow the ALARA principle (as low as reasonably achievable) and restrict the clinical use of CBCT to individual cases for follow-up purposes [55]. The primary reason for this is that a conclusive diagnosis of the nature of the lesions cannot be rendered without first conducting a CBCT study. Secondly, the numerous issues identified may render the results incapable of being generalized. The findings of the studies incorporated in the analysis [2, 7, 9, 11, 32, 37-41] may have been exaggerated, given that they were carried out by professionals in a clinical or academic setting. To obtain a more accurate understanding of the effectiveness of EMS, multicenter studies are necessary to assess its performance in various contexts, as is customary in clinical practice. This is because prior research has shown that the dentist's involvement can significantly impact the outcome [51]. Some authors did not include teeth with probing depths greater than 4 mm [40], teeth that had not received non-surgical endodontic retreatment [9], or teeth with traumatic lesions in their analyses. While these factors are taken into account to enhance the effectiveness of the intervention, they may result in an overestimation of the EMS outcome, which would undermine both the study's credibility and its relevance to actual clinical practice. No study considered the cost-effectiveness of the root-end filling material. The dentist and patient could benefit from using this ratio to determine the most appropriate treatment.
CONCLUSION
Employing contemporary surgical methods in conjunction with bioactive and suitable root-end filling materials may lead to a tooth survival rate of approximately 79 to 100%. A number of factors may impact the outcome of the surgical procedure, such as smoking history, tooth type and location, the presence or absence of dentinal error, interproximal cartilage level, and the type of root-end filling material used. It is worth noting that the clinical results of Pro Root MTA as a root end-filling material were superior to those of other materials. Based on this, the authors suggest that these materials should be the material of choice.
AUTHORS' CONTRIBUTIONS
A.I., M.A.A., H.A.A., O.K., and H.A.A. conceived and designed the study, did the review of the literature, provided research materials, and wrote the initial drafts of the article.
I.T.A, G.R.A.A., K.H.A.A and A.M.A did the systematic analysis with a quality check.
M.K.A. and S.V. wrote the final drafts of the article for important intellectual content and R.I., M.M., F.A.C., M.R.M, and N.P. approved the final version to be published.
All authors critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.


