Pathological Mandible Fracture Resulting from Osteomyelitis after Third Molar Removal: A Case Study
Abstract
Objective
The study aimed to report a case of late mandibular fracture after osteomyelitis associated with post-extraction trauma of an impacted third molar.
Case Report
A male patient, 48 years old, sought oral and maxillofacial surgery service after 2 months of extraction with edema on the left side of the face, limited mouth opening, and spontaneous pain. The tomographic examination showed an area of bone resorption at a mandibular angle starting from the alveolus region of the tooth 38. Associating the clinical and imaging characteristics, the diagnosis of osteomyelitis was established. The patient became well due to the drug treatment and did not present any more complaints. Within 12 months after the extraction, the patient returned to the service with a new increase in volume, in the posterior region of the mandible, with mandibular mobility under manipulation, as well as signs of infection. A new CT showed the presence of a pathological fracture in the region, requiring a surgical approach for local debridement and fracture repair with the use of a reconstruction plate.
Conclusion
The case presented is an uncommon late postoperative complication after third molar extraction, which demonstrates the importance of monitoring the patient with osteomyelitis, in order to avoid worsening bone involvement and consequent pathological fracture.
1. INTRODUCTION
Osteomyelitis is characterized as being an infectious and inflammatory process associated with the bone structure; although it does not occur very frequently, especially with the advent of antibiotics, it can cause relevant complications, such as pathological fractures or septicemia [1]. Most cases arise following bone trauma, surgical procedures, or secondary to insufficient vascularization [2].
It is usually characterized by a single site of infection, which may appear as a complication of an infection that is not specific to the associated site. Among the microorganisms most frequently identified in osteomyelitis are Staphylococcus aureus, Streptococcus, Enterococci, pseudomonas, Enterobacteria, and some anaerobic bacteria (Peptoestreptococos, Clostridium,etc.) [3]. Therefore, infections often manifest in a mixed manner, prompting an empirical selection of antibiotics based on the most likely characteristics and microorganisms [2]. In the oral and maxillofacial regions, the presence of infections frequently involves a polymicrobial anaerobic bacterial microbiota, and not all are cultivable [4].
Pathologic mandibular fractures are rare, accounting for approximately less than 2% of all mandibular fractures. The bone structure weakened by the infectious process characteristic of osteomyelitis becomes susceptible to the occurrence of pathological fractures, depending on the degree of involvement. The fracture is a serious complication that needs to receive treatment for the functional restoration of the affected region, requiring bone reduction and fixation [5, 6].
This type of fracture associated with the removal of third molar teeth can occur during the transoperative period or in the following weeks in the postoperative period [6]. The technique of third molar extraction usually requires a greater application of force or more extensive osteotomies and ostectomies than those used in other teeth, which can cause bone fragility in the mandibular bone for a certain period [7].
Thus, this study aimed to present a case of osteomyelitis following the extraction of the lower third molar in the mandible, leading to a late pathological fracture. The main purpose was to reflect on the importance of diagnosis and patient monitoring in the face of this condition.
2. CASE REPORT
A male patient, 49 years old, approached the Maxillofacial Surgery and Traumatology Service at the Dom Luiz Gonzaga Fernandes Emergency and Trauma Hospital in Campina Grande/PB. He reported an extraction 2 months before, evolving with increased volume in the left submandibular region. He stated that in the first month, he was prescribed and instructed to use antibiotic therapy, but did not use the indicated medications. During the examination, in addition to swelling in the left submandibular region, the patient exhibited significant trismus, spontaneous pain, extraoral hardness upon palpation, and intraoral redness in the area of the extraction of tooth 38. However, there was no discharge or bone exposure.
His medical history did not reveal allergies; however, he reported being hypertensive and using propranolol hydrochloride as a medication for daily control of his condition. The patient provided a panoramic radiograph prior to the surgical procedure, revealing the mesioangular bony impaction of tooth 38 (Fig. 1).
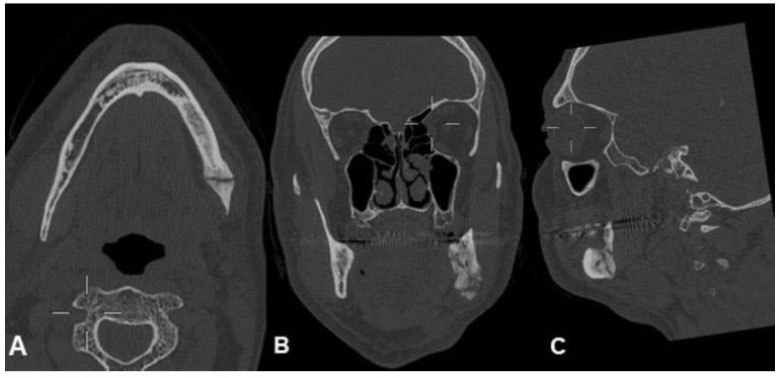
The initial tomographic examination revealed bone resorption with areas of bone sequestration in the region of the mandibular angle, associated with the alveolus of tooth 38, with a preserved marginal mandibular contour (Fig. 2). Correlating the clinical and imaging findings resulted in the final diagnosis of post-extraction acute osteomyelitis.
The patient underwent antibiotic therapy with intravenous Clindamycin 600mg every 8 hours, along with associated analgesics, in a hospital setting. After a 7-day period, the patient was discharged from the hospital with the continuation of the antibiotic regimen at home, administered orally, for an additional 30 days. After completing the medication, the patient exhibited signs of clinical improvement, indicating that, at that point, there was no need for surgical intervention or continued antibiotic use. It needs to be emphasized that subsequent follow-up appointments were scheduled; however, the patient did not attend the outpatient clinic, and attempts to establish contact were unsuccessful.


Approximately one year after the presented condition, the patient came to the service complaining of intense pain in the left submandibular region, associated with the increase in volume and presence of purulent secretion, denying that there had been any type of trauma episode in the region. During the clinical examination, mandibular mobility upon manipulation was observed. The patient denied experiencing or hearing any clicks from the region.
In a tomographic exam, the presence of a fracture in the region of tooth 38 was verified, as well as destruction of the buccal cortical bone, being replaced by a neoformed cortical bone (Fig. 3). For this reason, a surgical approach was planned for the patient's rehabilitation through the fixation of the pathological fracture. The surgical procedure involved curettage of the existing granulation tissue, regularization of the cortical plates with the removal of the bony callus, application of L-PRF, and installation of a titanium reconstruction plate with screws for the alignment and stabilization of the bone fracture.
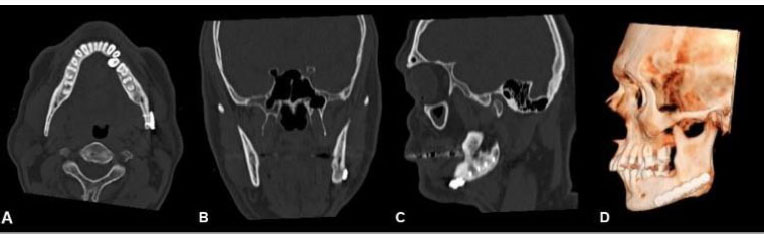
The patient was followed up and re-evaluated during 6 months, and no postoperative complications or signs of infection were observed. Occlusion and function were found to be recovered and preserved. Bone neoformation in the fragile area was observed on tomographic images (Fig. 4).
3. DISCUSSION
The extractions of impacted third molars are part of the clinical routine of dentistry and generally do not present major associated complications, in either the trans or postoperative period. However, complications can arise in about 4,6 to 30,9% of the cases [1, 8]. The trauma resulting from the intraoperative phase, especially in the presence of osteotomies and ostectomies, can lead to postoperative infection, resulting from its dissemination in the context of osteomyelitis [2].
Osteomyelitis is initially treated with antibiotics, and the drug of choice is clindamycin due to its effectiveness against the microorganisms commonly found in this pathology. Patients may require hospitalization for intravenous administration of this medication and monitoring of clinical progress [9]. This treatment is aimed at resolving the infectious process and maximizing patient function [10]. The recommended duration of antibiotic therapy is typically 4 to 8 weeks initially, and the duration may be based on patient adherence, clinical progress, and overall health status, along with an assessment of systemic inflammatory markers [11].
Several risk factors may be associated with pathological fractures, including the patient's gender and age, type of dental impaction, previous infection, associated bone lesions, surgical technique, associated comorbidities, as well as the patient’s cooperation in the post-operative phase (with regards to chewing harder foods or local traumas) [12-14].
Although the occurrence of the fracture in the reported case does not have a fully defined etiology, the literature describes excessive masticatory force as a fact that can cause considerable stress on the bone that is fragile due to the intraoperative process, as well as the presence of an infectious process, such as osteomyelitis [13, 15, 16].
Fractures associated with third molar removal in the mandibular bone region typically occur in the angle region due to its location and the fragile zone caused by the removal of the tooth [5, 17].
As in the case presented, studies in the literature [13, 14, 18] have shown clinical situations in which pathological fractures have occurred in a patient being 40 years old or more, implying age as a relevant risk factor. As a justification, there is a hypothesis that over the years, the mandible bone decreases its elasticity, becoming more corticalized and presenting a narrower periodontal ligament, which may require osteotomies that are more extensive in order to perform extractions [13, 18].
In the literature, similar cases can be found to the one presented, in which osteomyelitis may occur in the mandible after third molar extraction [19, 20]. Boffano et al. (2013) highlighted the presence of a periodontal infection related to the lower second molar with bacterial dissemination to adjacent areas or direct bacterial contamination during the trans-operative period as possible causes of post-extraction osteomyelitis.
In a literature review carried out by Boffano et al. (2013), it was highlighted that the occurrence of pathological mandibular fracture associated with third molar extraction is a rare event with an incidence of 0,0034% to 0,0075%, taking into account 17 previous studies. Furthermore, it was observed that most of these fractures (74%) occur in the first three weeks after surgery, and the others take place during the surgical procedure. In the presented case, the pathological fracture occurred late, which may be related to the chronic condition of osteomyelitis with slow evolution, i.e., an approximate period of one year after the extraction.
Most fractures associated with tooth extraction occur in the postoperative period, especially between the second and fourth weeks [15, 21, 22]. However, initial radiographs may not be able to reveal the fracture, especially since most patients may initially not have an occlusal change [5, 21]. Therefore, Pires et al. emphasized the importance of performing computed tomography if the suspicion continues even after performing control radiographs.
In the study by Wagner et al., 17 patients with mandibular fractures after third molar extractions were presented. In about 82% of the cases, the fracture occurred a few days after the surgical procedure, and in 6 of these cases, the fracture was not visualized on radiographic examination in the first postoperative review.
Clinical situations similar to the case reported in this study can be found in the literature with a late pathological fracture after the extraction of an impacted third molar tooth [1, 5, 7, 18].
The treatment of pathological mandibular fractures can be difficult due to their etiology, which can often be non-specific, as well as the general and local conditions that can be limiting; in most cases, an open approach may be required with a more rigid fixation of the affected region [6]. The treatment options that can be applied include conservative treatment with dietary guidance (liquid/pastry food in the first months), closed treatment (with maxillomandibular block), and open treatment (with plates and screws for bone fixation) [5, 17].
Furthermore, the medical conditions that may affect the chosen conduct should be investigated in order to define the options that are more favorable for the patient. The lack of continuity created by the defect can be re-established by installing 2,4 mm or smaller diameter system plates, with primary or secondary reconstruction as initial interventions, depending on the local and systemic conditions of each patient [6].
With respect to the clinical and imaging conditions presented in the case, and the associated late characteristics, an open approach for local curettage was necessary involving the reduction and fixation of the fracture with the 2,4 mm system, which provided stability and recovered the patient’s masticatory functionality and occlusion. That conduct was performed according to recent studies [1, 5, 6, 13] and with satisfactory clinical applicability.
It is known that Leucocyte-rich and Platelet-rich Fibrin (L-PRF) has important properties that stimulate healing and promote tissue regeneration, which is why it is frequently used in oral and maxillofacial surgery [23]. Taking into account this existing potential, the L-PRF was used in the region to cover the fixed bone. A study by Crisci et al. recommended the application of L-PRF in skin lesions up to the bone affected by osteomyelitis after surgical debridement. This achieved favorable results without evidence of infection in the long-term follow-up.
As a limitation of this case report, it is not possible to state precisely in which specific period of time the fracture occurred, as well as the exact etiology. It is, however, known that there was an initial existence of a clinical picture of acute osteomyelitis, which was initially solved by antibiotic therapy. Also, it is unclear whether the new episode of osteomyelitis was a consequence of the primary condition presented. Clinical follow-up and patient collaboration may be of great importance in situations like these [24].
CONCLUSION
In the present case, the clinically suggestive condition of osteomyelitis following the extraction of the third molar, initially managed with antibiotic therapy, exhibited a chronicity pattern with a probable slow progression. The advancement of the pathology led to bone fragility, resulting in a mandible fracture, deemed unusual in a later period. Therefore, post-surgical follow-up with close patient monitoring, both clinically and radiographically, is essential in the face of the initial signs of infection. Additionally, the early diagnosis of osteomyelitis and the determination of the most appropriate therapeutic approach are of great importance for preventing pathological mandible fractures.
CONSENT FOR PUBLICATION
Informed consent was obtained from the patient for publication of the findings.
AVAILABILITY OF DATA AND MATERIALS
All the data and supporting information are provided within the article.
CONFLICT OF INTEREST
Dr. Emanuel Savio de Souza Andrade is on the editorial advisory board of The Open Dentistry Journal.
ACKNOWLEDGEMENTS
Declared none.


