All published articles of this journal are available on ScienceDirect.
Preventive Habits in University Workers during SARS-CoV-2 Pandemic
Abstract
Background
SARS-CoV-2 and the consequent public health measures changed our habits, including prevention in oral health.
Objectives
The aim was to investigate the relationship between the perceived risk for SARS-CoV-2 infection and preventive habits, including COVID-19 preventive measures, general health preventive attitudes and oral-hygiene habits.
Materials and Methods
Data were collected via a web-based questionnaire, matched with medical history data obtained by the Occupational Medicine Service. Descriptive statistics were used to analyze the results of this observational cross-sectional study. Potential and investigated associations were studied through multivariate logistic regression.
Results
The perceived risk increases with age and decreases with a diabetes family history. The percentage of those with a dentist visit in the past three months is about three times higher among people who tested negative for COVID-19 than the positives. The percentage of those who had a dentist visit in more than six months is higher among the positives. Gingival bleeding was more frequent among people who tested positive for COVID-19, while it was a less frequent symptom in the negative group.
Conclusion
Results highlight a relation between the risk of testing positive for COVID-19 and oral health preventive habits. There is a relationship between oral health and risk perception for SARS-CoV-2.
1. INTRODUCTION
The COVID-19 pandemic represented a worldwide challenge for communities and health authorities.
In Italy, after a strict lockdown lasting two months and a half, non-essential public and private economic activities reopened gradually, while travel restrictions were still in place. During this period, the University of L’Aquila (Italy) reorganized its institutional activities and set up a COVID-19 Committee composed of the University Executive Officers, the Health and Safety Office, the Workers' Health and Safety Representatives, and the Occupational physicians. Countermeasures to reduce COVID-19 risk were implemented, including remote learning, teleworking, reduced capacity within the offices and the laboratories, social distancing, use of personal protective masks, and the spread of information about correct hygiene measures with many consequences for both workers and users of the service [1-4].
Subsequently, in compliance with the new provisions, all non-practical and non-manual activities were organized and performed only remotely, using Video Conference programs. These new organizational strategies lasted until the second semester of the 2020-2021 Academic Year, and they were also extended to traineeships that could be organized remotely. Only a few traineeships in the health area were held in person by following strict infection control precautions. In this context, considering the evolution of the pandemic, which was characterized by peaks and drops in the number of cases, researchers, full and associate professors, administrative and technical staff, and research fellows continued to attend the premises alternatively. In addition, workers could be in contact with the public, especially technicians and administrative staff.
On-site working was strongly limited to urgent and non-deferrable activities, even access to laboratories was tightened due to space limitations.
Many reports have demonstrated that COVID-19 restriction measures, especially lockdown and social distancing, can cause mild to severe negative effects on workers’ mental wellness [5].
As the economy and unemployment raise concerns, active measures of healthy habit promotion could play an important role in improving both psychological and physical health in the general population [6].
Nonetheless, the distress linked to the pandemic scenario represented a relevant disturbing factor for compliance with preventive behaviors, as psychological well-being is key to establishing and maintaining healthy habits and strengthening behavior consistency [7].
Dental care was also affected. Regular dental checkups were mostly discontinued [8], and despite the increase in oral and dental health complaints, fear of COVID-19 outdid the intent of visiting the dentist [9], limiting the visits only to urgent treatments [10].
In January 2021, the occupational health service of the University of L’Aquila organized a survey to investigate some medical and behavioral aspects related to the COVID-19 pandemic and its effect on oral health habits. The form involved SARS-CoV-2 infection and detection, symptoms, and changes in habits due to restrictions and quarantine. This study followed up another research designed to quantify antibody response (determination of Immunoglobulin M - IgM and Immunoglobulin G - IgG levels in the blood) against SARS-CoV-2 infection in the personnel of the University. This study was conceived to quantify the number of people who contracted the virus because of the so-called first and second pandemic waves in Central Italy, and it was performed before the adoption of vaccines.
The quantification of the above immunoglobulins was linked to pathologies and was merged with the results of an online form administrated to professors, technicians, research fellows, Ph.D. candidates, and resident physicians of the University.
The primary aim of this study was to relate the preventive habits of people in Italy and their attitudes towards common screening tests (such as colonoscopy, mammography, and PAP test), their sports, smoking, and alcoholic habits, and the probability of being infected by SARS-CoV-2 and to develop symptoms. A further aim of this investigation was to verify connections between the above habits, oral and dental hygiene habits, and the risk of getting infected and developing symptoms.
2. MATERIALS AND METHODS
This study was approved and allowed by the Institutional Review Board of the University of L’Aquila. The research was developed to investigate the connections between health values and preventive habits of people working at the University of L’Aquila and their attitudes to SARS-CoV-2 infection and the development of symptoms. This study was designed when the supply of swab kits and the use and diffusion of vaccines were still limited, so the importance of non-infection was central. Data were acquired during visits conducted by the Occupational Medicine Service and by dosing the total amount of IgGs and IgMs in blood samples obtained from the working staff of the University.
This study was designed within the “Ateneo in Salute” project (in Italian “Healthy University” Project). In this context, the Occupational Medicine Service had a central role throughout the pandemic, because it was involved in stating rules and policies regarding access to the University facilities.
In Italy, on March 3rd, 2020, access to students was declared forbidden. Until the end of May, access was allowed to a limited number of people for essential and non-deferrable activities. Then, access was regulated by assigning workspace to each staff member, by always wearing compulsory face masks, and by organizing all meetings virtually, using video conferencing software. However, professors, technical and administrative staff, research fellows, Consultants, and doctoral students continued to attend the university facilities to carry out their studies and teaching activities. Access for students to facilities and libraries was strictly limited and was allowed for specific needs only. Legally, remote working was preferred for members of the staff and normally applied, both in public administration and in private enterprises.
This study was based on a homogeneous population of professors, researchers, research fellows, doctoral students, technical and administrative staff, and students attending the university to write their thesis or do their internship. The study aimed to evaluate the following:
- The relationship between the risk of being infected by SARS-CoV-2 and the habit of adopting preventive oral health habits, such as frequency of dental visits and use of mouthwashes.
- The relationship between the infection risk and self-perception of gingival inflammation and/or periodontitis.
- The relationship between the probability of being infected and the attitude to adopt preventive habits in general, such as the influenza vaccination habits and the frequency of participation in screening programs.
- The perception of infectious and personal health risks related to the pandemic event.
The secondary aim was to evaluate statistically significant differences not foreseen in this study between the positive and non-positive group, or also between other homogeneous groups, and to evaluate the higher or lower frequency of specific symptoms in the positives and in the subgroups of the positives, such as the positives only in the serological and/or molecular test.
This study aims to investigate whether there were changes in the health and oral health habits consequently to the pandemic in a reasonably homogeneous population, i.e., different categories of university workers who mostly worked from home but who also attended the University facilities to carry out their work.
The focus was on the analysis of the differences between the control group (considering those subjects found “negative” or “unreactive” to blood tests) and the group of people who tested positive for COVID-19 disease. By positive, the authors indicate people who tested positive for PCR test, rapid antigen test, or antibody serology test after the infection. We also considered potentially positive people who reported three symptoms or more, who, however, had tested negative. In addition, during the acute phases of the pandemic, not all of those who needed a molecular COVID-19 diagnostic test could receive it, or they received the test after a long time when they probably had already recovered from the viral infection.
Systemic health data, symptoms, systemic health habits, self-perceived oral health data, and oral hygiene attitudes were investigated. Questions were about the self-perception of symptoms, with the symptoms list usually associated with COVID-19 syndrome. People reported to the Occupational Medicine Service staff whether they had been subjected to quarantine (so-called compulsory fiduciary isolation) or to hospitalization. The collection of data using Microsoft Form™ was from January 2021 to April 2021, while the data acquired by the previously conducted “Ateneo in Salute” Project were also obtained during the same period by the Occupational Medicine Service. Respondents also reported the type of test they had received. In order to find possible connections between these pathologies and habits and COVID-19 symptoms, respondents were also asked about their home oral hygiene practices, their attitudes toward attending the dental clinic to receive professional dental hygiene treatments, their self-perception of gingivitis or periodontitis, their dental flossing habits, and use of mouthwash.
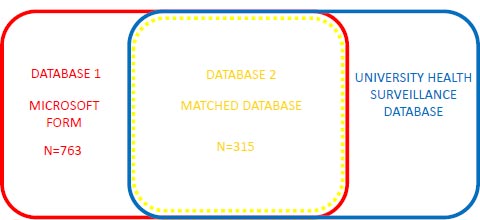
Data were obtained by sending a questionnaire using Microsoft Form™ via the University's email system. These data were matched with the data obtained from the serological tests performed by the Occupational Medicine Unit of the University of L’Aquila, and from the “Ateneo in Salute” Project. The project provided data about recent and past personal and family history. Data were then tabled using Microsoft Excel™. Thus, two databases were generated, one obtained by matching the two databases and the other one obtained by tabling the data acquired using Microsoft Form™.
The characteristics of the study sample of this observational cross-sectional study were analyzed using descriptive statistics. Using the molecular swab result, the study population was stratified into two groups: positive COVID-19 subjects and negative COVID-19 subjects. Discrete and nominal variables were expressed using frequencies and percentages, and the χ2 test or Fisher's exact test, as appropriate, were used to examine differences between the two groups. The continuous variables were expressed as mean and values and standard deviations (SDs) or median and Interquartile Range (IQR), whose significance was assessed with a t-test for independent samples.
Multivariate logistic regression was used to assess the associations, expressed as odds ratios (ORs) with 95% confidence intervals (95% CIs), between molecular swab negativity/positivity, chosen as a dependent variable, and each explanatory variable with significant levels lower than 0.05. Backward stepwise selection with the Akaike information criterion (AIC) was used to choose the best logistic regression model. A p-value of <0.05 was the criterion for statistical significance. The data were processed using the STATA/IC 15.1 statistical package.
3. RESULTS
Two databases were analyzed. One dataset was obtained by matching the data acquired during the occupational health assessments in 2020 with those reported in the forms. The second database was obtained by organizing the data on the survey forms. The first database consisted of 315 subjects, while the second database consisted of 763 subjects (Fig. 1).
Regarding the descriptive analysis of the first database, as described in the previous section, the following data were collected: 366 respondents were professors or assistant professors (researchers), 235 were administrative and technical staff, 159 were so-called “full-time equivalent workers” (doctoral students, medical and dental residents, and research fellows), and three undergraduates (already attending the university laboratories or facilities for thesis preparation).
One of the central questions of the form was about their self-perception of symptoms and their persistence. Considering the total cohort of respondents, symptoms were rated from moderate to severe: 6.6% fatigue; 6.2% muscle aches; 3% loss of smell or taste; 2.6% flu; 2.4% dry cough; 2.3% diarrhea; 2.2% fever; 1.7% sore throat; 1% conjunctivitis; 0.5% congested cough.
Eight respondents reported having symptoms for two weeks since they had tested positive, while 14 reported having symptoms until the form compilation.
Overall, 661 people did not experience any further social isolation restrictions, 74 were forced into so-called “fiduciary isolation,” 23 developed COVID-19 symptoms and were treated at home, and 5 were hospitalized. 715 reported not being in direct or close contact with a person who had tested positive for the COVID-19 test. Conversely, 48 respondents reported being in close contact with a COVID-19 case. Of these, 27 (57%) had contact with a cohabiting person. Interestingly, only one subject reported being tested positive for COVID-19 after having received a rapid antigen test. Twenty subjects reported a “reactive” or “positive” test result after a serological test.
Overall, 97 subjects of the study population underwent the COVID-19 swab testing. No significant statistical differences were found regarding gender, age, food habits, medical personal history, and type of employment at the University (Tables 1-3).
| Characteristics | n or Median | % or IQR |
Nasopharyngeal RT-PCR Test Result n (%) or Median (IQR) |
p-value | |
| - | - | - |
Negative 82 (84.54%) |
Positive 15 (15.46%) |
- |
| Gender | - | - | - | - | - |
| Male | 46 | 47.42% | 37 (45.12%) | 9 (60.00%) | 0.289* |
| Female | 51 | 52.58% | 45 (54.88%) | 6 (40.00%) | |
| Age | 52 | 39-58 | 53 (40-58) | 44 (35-55) | 0.343** |
| Employment | - | - | - | - | 0.263*** |
| Professor | 40 | 41.24% | 36 (43.90%) | 4 (26.67%) | |
| Other | 57 | 58.76% | 46 (56.10%) | 11 (73.23%) | |
| Characteristics | n or Median | % or IQR |
Nasopharyngeal RT-PCR Test Result n (%) or Median (IQR) |
p-value | |
| - | - | - |
Negative 82 (84.54%) |
Positive 15 (15.45%) |
- |
| Family medical history | |||||
| Diabetes | - | - | - | - | 0.277* |
| No | 72 | 77.42% | 62 (79.49%) | 10 (66.67%) | - |
| Yes | 21 | 22.58% | 16 (20.51%) | 5 (33.33%) | - |
| Personal medical history | |||||
| Medication intake | - | - | - | - | 0.394** |
| No | 57 | 61.96% | 46 (59.74%) | 11 (73.33%) | - |
| Yes | 35 | 38.04% | 31 (40.26%) | 4 (26.67%) | - |
| Physical activity | - | - | - | - | 0.261* |
| No | 43 | 46.74% | 34 (44.16%) | 9 (60.00%) | - |
| Yes | 49 | 53.26% | 43 (55.84%) | 6 (40.00%) | - |
| Times/week | 3 | 2 - 3 | 3 (2 - 3) | 2.5 (2 - 5) | 0.920*** |
| Minutes/week | 135 | 90 - 200 | 150 (90 - 200) | 120 (120 - 150) | 0.872*** |
| Metabolic syndrome | - | - | - | - | 0.165** |
| No | 90 | 98.90% | 76 (100.00%) | 14 (93.33%) | - |
| Yes | 1 | 1.1% | 0 (0.00%) | 1 (6.67%) | - |
| Cardiovascular disease | - | - | - | - | 0.256** |
| No | 85 | 93.41% | 72 (94.74%) | 13 (86.67%) | - |
| Yes | 6 | 6.59% | 4 (5.26%) | 2 (13.33%) | - |
| Characteristics | n or Median | % or IQR |
Nasopharyngeal RT-PCR Test Result n (%) or Median (IQR) |
p-value | |
| - | - | - | Negative | Positive | - |
| Screening test | |||||
| Breast screening (Mammogram) | - | - | - | - | 0.344* |
| No | 14 | 29.79% | 11 (26.83%) | 3 (50.00%) | - |
| Yes | 33 | 70.21% | 30 (73.17%) | 3 (50.00%) | |
| Characteristics | n (%) or mean±SD |
Score n (%) or mean±DS |
p-value | |
|
1 – 7 155 (49.36%) |
8 – 10 159 (50.64%) |
|||
| Age | 49.48±11.41 | 46.73±11.26 | 52.05±10.98 | <0.001* |
Regarding the dental and oral hygiene section of the form, 59% (453 people) reported not attending a dental office during the last six months at least. No one reported any worsened gingivitis and periodontal disease, while three people reported perceiving gingival bleeding or a worsened gingivitis on brushing.
Most people (169) reported perceiving SARS-CoV-2 as a dangerous threat to their health (on a scale of 10, they rated it 8). Overall, 671 people were in favor of vaccine prophylaxis, while 83 expressed doubts about vaccinations. Only 9 people reported being “against” vaccines and not trusting their efficacy (Data from Microsoft Form™).
Regarding the matched database explained in Fig. (1), a statistically significant difference was found in risk perception towards COVID-19 between those with a medium risk perception (score 1 to 7) and those with a higher risk perception (score 8 to 10), considering that the first group had an average age of 46.73±11.26 of SD, while the second group had an average age of 52.05±10.98 of SD (p-value < 0.001) (Tables 4-6).
Focusing on the “prevention attitude” shown by the university employees, the data about participation in screening campaigns from the whole group of employees and from the group of people who had tested positive for the infection were matched. Referring to Tables 3 and 6, no difference between the two groups can be found. Likewise, regarding the differences in infection risk between the group of people who had received seasonal influenza vaccination and those who had not received the same vaccination, no substantial differences were found. Although there was a little discrepancy, no significant difference was found between the group of people with no reported family history of diabetes and those with a reported family history of diabetes.
Details about the results regarding symptoms, restrictive measures, and screening participation are described in Tables 4-6.
Factors related to SARS-COV 2 risk perception are described in Table 7.
Table 5.
| - | n (%) or mean±DS |
Score n (%) or mean±SD |
p-value | |
|
1 – 7 155 (49.36%) |
8 – 10 159 (50.64%) |
|||
| Family medical history | ||||
| Diabetes | - | - | - | 0.032* |
| No | 251 (82.03%) | 115 (77.18%) | 136 (86.62%) | - |
| Yes | 55 (17.97%) | 34 (22.82%) | 21 (13.38%) | |
| Cardiovascular disease | - | - | - | 0.285* |
| No | 236 (77.63%) | 118 (80.27%) | 118 (75.16%) | - |
| Yes | 68 (22.37%) | 29 (19.73%) | 39 (24.84%) | |
| Personal medical history | ||||
| Smoking | - | - | - | 0.398* |
| No | 256 (83.39%) | 127 (85.23%) | 129 (81.65%) | - |
| Yes | 51 (16.61%) | 22 (14.77%) | 29 (18.35%) | - |
| Cigarettes/day | 9.24±5.76 | 10.24±6.52 | 8.40±5.04 | 0.341** |
| Alcohol intake | - | - | - | 0.056* |
| No | 209 (68.30%) | 94 (63.09%) | 115 (73.25%) | - |
| Yes | 97 (31.70%) | 55 (36.91%) | 42 (26.75%) | - |
| Medication intake | - | - | - | 0.147* |
| No | 204 (66.45%) | 105 (70.47%) | 99 (62.66%) | - |
| Yes | 103 (33.55%) | 44 (29.53%) | 59 (37.34%) | - |
| Physical activity | - | - | - | 0.357* |
| No | 136 (44.30%) | 62 (41.61%) | 74 (46.84%) | - |
| Yes | 171 (55.70%) | 87 (58.39%) | 84 (53.16%) | - |
| Times/week | 2.96±1.47 | 3.00±1.23 | 2.90±1.71 | 0.682** |
| Minutes/week | 180.66±134.60 | 179.70±117.55 | 181.77±152.72 | 0.924** |
| Hypertension | - | - | - | 0.083* |
| No | 266 (87.21%) | 135 (90.60%) | 131 (83.97%) | - |
| Yes | 39 (12.79%) | 14 (9.40%) | 25 (16.03%) | - |
| Malignant tumors | - | - | - | 0.069* |
| No | 289 (94.14%) | 144 (96.64%) | 145 (91.77%) | - |
| Yes | 18 (5.86%) | 5 (3.36%) | 13 (8.23%) | - |
| * χ2 test ** Student’s t test ***Fisher exact test | ||||
| - | n (%) or mean±DS |
Score n (%) or mean±SD |
p-value | |||||||||
|
1 – 7 155 (49.36%) |
8 – 10 159 (50.64%) |
|||||||||||
| Screening test | ||||||||||||
| Cervical cancer screening (Pap-smear test) | - | - | - | 0.269* | ||||||||
| No | 17 (10.06%) | 10 (12.82%) | 7 (7.69%) | - | ||||||||
| Yes | 152 (89.94%) | 68 (87.18%) | 84 (92.31%) | - | ||||||||
| Colorectal cancer screening (Colonoscopy) | - | - | - | 0.145* | ||||||||
| No | 183 (63.54%) | 93 (67.88%) | 90 (59.60%) | - | ||||||||
| Yes | 105 (36.46%) | 44 (32.12%) | 61 (40.40%) | - | ||||||||
| Breast cancer screening (Mammogram) | - | - | - | 0.194* | ||||||||
| No | 44 (26.04%) | 24 (30.77%) | 20 (21.98%) | - | ||||||||
| Yes | 125 (73.96%) | 54 (69.23%) | 71 (78.02%) | - | ||||||||
| - | Odds Ratio |
C.I. (95%) |
p-value |
| Age | 1.04 | 1.02 - 1.06 | 0.001 |
| Diabetes | - | - | - |
| Noa | 1 | - | - |
| Yes | 0.53 | 0.28 - 0.99 | 0.049 |
| Serological test | - | - | - |
| Noa | 1 | - | - |
| Yes | 2.87 | 0.94 - 8.88 | 0.064 |
| Preventive measures and use of PPE | - | - | - |
| Oftena | 1 | - | - |
| Always | 2.09 | 0.95 - 4.63 | 0.068 |
AIC=382.
A difference was found between the group of those who had received professional oral hygiene treatments during the last six months and those who had received the same treatments more than six months earlier.
The matched database presented the following numbers after the data analysis.
In the comparison between the two groups (positive or not for the molecular swab), statistically significant differences emerged based on the job performed: the non-teaching staff tested positive with a higher frequency than the teaching staff (72.97% vs. 52.61%, p = 0.021). Regarding preventive dentistry habits, the percentage of those who had gone to dentists and/or hygienists at least three months earlier was about three times higher among negatives than positives (31.75% vs. 10.81%), while the percentage of those who had gone to the dentist and/or hygienist more than six months earlier was higher among the positives than the negatives (67.57% vs 53.085%) (p = 0.022).
Those with a high-risk perception towards COVID-19 received more serological tests (96.86% vs. 90.97%, p = 0.029) and reported adopting preventive measures and using personal protective equipment more frequently compared to those with a medium-low risk perception towards the infection (93.08% vs 83.87%, p = 0.010) (Table 8).
Gingival bleeding was more frequent among positives than negatives (35.14% vs. 19.43%, p = 0.033), and among these, the use of electric toothbrushes was less frequent than positives (28.91% vs 45.95%, p = 0.040) (Tables 9, 10 and 11).
As shown in Table 10, those who attended dental offices more frequently to receive dental hygiene treatment showed a lower percentage of positivity to SARS-CoV-2 infection, demonstrating a better preventive attitude.
| - | n (%) or mean±DS |
Score n (%) or mean±SD |
p-value | |||||||||
|
1 – 7 155 (49.36%) |
8 – 10 159 (50.64%) |
|||||||||||
| Nasopharyngeal RT-PCR test | - | - | - | 0.082* | ||||||||
| No | 217 (69.11%) | 100 (64.52%) | 117 (73.58%) | - | ||||||||
| Yes | 97 (30.89%) | 55 (35.48%) | 42 (26.42%) | |||||||||
| Results | - | - | - | 0.257** | ||||||||
| Negative | 82 (84.54%) | 44 (80.00%) | 38 (90.48%) | - | ||||||||
| Positive | 15 (15.46%) | 11 (20.00%) | 4 (9.52%) | - | ||||||||
| Quick antigenic swab | - | - | - | 0.915* | ||||||||
| No | 161 (51.27%) | 79 (50.97%) | 82 (51.57%) | - | ||||||||
| Sì | 153 (48.73%) | 76 (49.03%) | 77 (48.43%) | |||||||||
| Results | - | - | - | / | ||||||||
| Negative | 153 (100.00%) | 76 (100.00%) | 77 (100.00%) | - | ||||||||
| Positive | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | - | ||||||||
| Serological test | - | - | - | 0.029* | ||||||||
| No | 19 (6.05%) | 14 (9.03%) | 5 (3.14%) | - | ||||||||
| Yes | 295 (93.95%) | 141 (90.97%) | 154 (96.86%) | |||||||||
| Results | - | - | - | 0.526* | ||||||||
| Negative | 302 (96.18%) | 148 (95.48%) | 154 (96.86%) | - | ||||||||
| Positive | 12 (3.82%) | 7 (4.52%) | 5 (3.14%) | - | ||||||||
| Preventive measures and use of PPE | - | - | - | 0.010* | ||||||||
| Often | 36 (11.46%) | 25 (16.13%) | 11 (6.92%) | - | ||||||||
| Always | 278 (88.54%) | 130 (83.87%) | 148 (93.08%) | - | ||||||||
| COVID-19 vaccine propensity | - | - | - | 0.999** | ||||||||
| No | 2 (0.64%) | 1 (0.65%) | 1 (0.63%) | - | ||||||||
| Yes | 281 (89.49%) | 139 (89.68%) | 142 (89.31%) | - | ||||||||
| Don’t know | 31 (9.87%) | 15 (9.68%) | 16 (10.06%) | - | ||||||||
| Characteristics | n (%) or mean±SD |
Nasopharyngeal RT-PCR Test Result n (%) or mean±SD |
p-value | |||||||||
| - | - |
Negative 211 (85.08%) |
Positive 37 (14.92%) |
- | ||||||||
| Sex | - | - | - | 0.289** | ||||||||
| Male | 46 (47.42%) | 37 (45.12%) | 9 (60.00%) | - | ||||||||
| Female | 9 (60.00%) | 45 (54.88%) | 6 (40.00%) | - | ||||||||
| Age | 48.93±11.97 | 49.38±12.14 | 45.73±10.60 | 0.346* | ||||||||
| Employment | - | - | - | 0.021** | ||||||||
| Professor | 110 (44.35%) | 100 (47.39%) | 10 (27.03%) | - | ||||||||
| Other | 138 (55.65%) | 111 (52.61%) | 27 (72.97%) | - | ||||||||
| - | n (%) or mean±SD |
Nasopharyngeal RT-PCR Test Result n (%) or mean±SD |
p-value | |||||||||
|
Negative 211 (85.08%) |
Positive 37 (14.92%) |
|||||||||||
| Last dental appointment | - | - | - | 0.022** | ||||||||
| <3 months | 71 (28.63%) | 67 (31.75%) | 4 (10.81%) | - | ||||||||
| 3 to 6 months | 40 (16.13%) | 32 (15.17%) | 8 (21.62%) | - | ||||||||
| >6 months | 137 (55.24%) | 112 (53.08%) | 25 (67.57%) | - | ||||||||
| Last professional oral hygiene | - | - | - | 0.140*** | ||||||||
| <6 months | 90 (36.29%) | 80 (37.91%) | 10 (27.03%) | - | ||||||||
| 6 to 12 months | 68 (27.42%) | 53 (25.12%) | 15 (40.54%) | - | ||||||||
| >12 months | 90 (36.29%) | 78 (36.97%) | 12 (32.43%) | - | ||||||||
| Gingivitis and/or periodontitis within the past year | - | - | - | 0.481** | ||||||||
| No | 231 (93.15%) | 195 (92.42%) | 36 (97.30%) | - | ||||||||
| Yes | 17 (6.85%) | 16 (7.58%) | 1 (2.70%) | - | ||||||||
| Gingival bleeding after brushing | - | - | - | 0.033*** | ||||||||
| No | 194 (78.23%) | 170 (80.57%) | 24 (64.86%) | - | ||||||||
| Yes | 54 (21.77%) | 41 (19.43%) | 13 (35.14%) | - | ||||||||
| Using mouthwash within the last 6 months | - | - | - | 0.108*** | ||||||||
| No | 181 (72.98%) | 158 (74.88%) | 23 (62.16%) | - | ||||||||
| Yes | 67 (27.02%) | 53 (25.12%) | 14 (37.84%) | - | ||||||||
| Type of toothbrushes | - | - | - | 0.040*** | ||||||||
| Manual | 170 (68.55%) | 150 (71.09%) | 20 (54.05%) | - | ||||||||
| Electric | 78 (31.45%) | 61 (28.91%) | 17 (45.95%) | - | ||||||||
| Daily dental flossing | - | - | - | 0.263*** | ||||||||
| No | 148 (59.68%) | 129 (61.14%) | 19 (51.35%) | - | ||||||||
| Yes | 100 (40.32%) | 82 (38.86%) | 18 (48.65%) | - | ||||||||
| - | - | - | - | |||||||||
| Recently reported halitosis | - | - | - | 0.671** | ||||||||
| No | 206 (83.06%) | 173 (81.99%) | 33 (89.19%) | - | ||||||||
| Yes | 27 (10.89%) | 24 (11.37%) | 3 (8.11%) | - | ||||||||
| Previous halitosis | 15 (6.05%) | 14 (6.64%) | 1 (2.70%) | - | ||||||||
| Student’s t test Fisher exact test χ2 test | ||||||||||||
| - | Odds Ratio |
C.I.
(95%) |
p-value | ||||||||||
| Employment | - | - | - | ||||||||||
| Professor | 1 | - | - | ||||||||||
| Other (Researcher, Technical-Administrative personnel, Student/Ph fellow) | 2.60 | 1.14 - 5.90 | 0.022 | ||||||||||
| Last dental appointment | - | - | - | ||||||||||
| <3 months a | 1 | - | - | ||||||||||
| 3 to 6 months | 5.68 | 1.46 - 22.01 | 0.012 | ||||||||||
| >6 months | 6.13 | 1.89 - 19.89 | 0.003 | ||||||||||
| Gingival bleeding after brushing | - | - | - | ||||||||||
| Noa | 1 | - | - | ||||||||||
| Yes | 2.77 | 1.22 - 6.26 | 0.015 | ||||||||||
| Type of toothbrush | - | - | - | ||||||||||
| Manuala | 1 | - | - | ||||||||||
| Electric | 3.01 | 1.38 - 6.57 | 0.006 | ||||||||||
The multivariate logistic regression model confirmed that the job, the timing of the last visit to the dentist or hygienist, the presence of bleeding in the past year, and the type of toothbrush used for oral hygiene are factors independently associated with molecular test positivity for COVID-19.
Family history of diabetes is more frequent in the group with a low-medium risk perception towards SARS-CoV-2 infection (22.82% vs 13.38%, p = 0.032).
The multivariate logistic regression analysis highlighted that risk perception towards SARS-CoV-2 infection in the sample group examined increases with age (OR 1.04, 95% CI 1.02 - 1.06, p = 0.001), and it decreases if there is a family history of diabetes (OR 0.53, 95% CI 0.28-0.99, p = 0.049) (Tables 2, 5, 8).
4. DISCUSSION
Analyzing the above data, the discussion can be divided into two parts. The first part addresses the relationship between the risk of positivity to SARS-CoV-2 and preventive oral hygiene habits, such as frequency of visits to the dentist and use of mouthwashes. The study also evaluated the relationship between positivity risk and self-perception of gingival inflammation and/or periodontitis. The second part of the discussion deals with an evaluation of the relationship between the risk of positivity to SARS-CoV-2 and preventive habits in general, such as influenza vaccination habits and the frequency of screening participation.
The difference found in risk perception of the COVID-19 illness could be caused by the fact that death risk increases with age [11] (Table 7).
Analyzing the dental attendance and attitudes to dentistry, some interesting data were found. During the first two heavy pandemic months (March and April 2020), in Italy, dental services, mostly represented by private offices and clinics, were limited by law to emergencies, moreover, people perceived a very high risk of COVID-19 contamination in dental settings, even if this belief was later refuted by evidence [12, 13]. Then services were gradually re-activated, permitting to receive most treatments safely.
The habit of visiting dental offices frequently is linked to a better preventive attitude. People who care for dental therapy could have a lower risk of testing positive for COVID-19. These results agree with the literature data [14]. The correlation between oral prevention habits and general health prevention habits should be evaluated in a separate paper.
Oral health maintenance, good oral-systemic health, and avoiding smoking may all be effective measures to prevent and control COVID-19 disease.
Gingival bleeding was more frequent among the positive group, linking this to a possible association between the COVID-19 inflammatory response and the gingival inflammatory response [15]. Surprisingly, the use of electrical toothbrushes was more frequent among the positive group, suggesting that people with a “preventive” attitude believe in achieving optimal dental hygiene by using manual toothbrushes [16, 18], so reflecting more on the act and the movements associated to toothbrushing [9, 17].
Regarding oral hygiene habits, fear and risk perception towards COVID-19 was higher in participants who paid more attention to their oral hygiene habits, developed different frequencies and number of meals, had an increased perception of the importance of dental health, and decided to postpone the dental visits.
Studies showed that stress caused by COVID-19 increases detrimental oral habits, such as temporomandibular disorders and bruxism. Young single females could be more at risk of developing these bad habits [19].
In our study, a difference was clear between teaching and non-teaching staff, with the second group being more likely to develop SARS-CoV-2 positivity [20]. These data should be linked with the different tasks, the different accessibility, and different exposure to the public [21], considering that teaching activity (excluding traineeships) was carried out by use of video conferencing software, as described above.
Analyzing preventive habits in general, a family history of diabetes is associated with a medium risk perception of COVID-19, not an elevated one, which is linked with a medium risk connected to COVID-19 disease (Table 8). Analyzing these data, the increased risk for people affected by diabetes should be considered [22-24], which apparently disproves this perception founded by us. Patients affected by chronic diseases were indicated as “patients at risk” by mass media communications at the beginning of the pandemic. This result is probably linked to the habitual relationship of these people with the concepts of risk and disease. People who normally attributed high risk to COVID-19 disease underwent more serological exams to check for infections.
People who declared to the Occupational Medicine Service to suffer from cardiovascular diseases show a higher likelihood of testing positive, even if p is not <0.05. This phenomenon could not be explained only by referring to comorbidities demonstrated for COVID-19 [25, 26], because in our study, an association between cardiovascular disease and the risk of testing positive for COVID-19 can be found.
This study shows that different jobs and different exposure to the public could be linked to different possibilities to be found positive for COVID-19. The difference could be attributed to different ages linked to different occupations and job positions.
The attitude to attend a dental office to receive professional hygiene treatment is linked to a decreased risk of testing positive for COVID-19, thus suggesting that preventive oral hygiene attitudes are linked to adherence to preventive measures and social distancing attitudes. This finding also disproves the initial belief that associated dental offices with COVID-19 risk due to aerosol production during dental practice. This belief has been disproved by the scientific literature [12, 13]. The authors underline these data because they remark on the safety of dental offices even during pandemic difficulties. After all, already in “normal” circumstances, dentists and dental hygienists must prevent cross infections. The authors, however, remind us that these are self-declarations obtained from a survey form, and so they are susceptible to inaccuracies or misperceptions by study participants. In addition, the authors underline that the sample was represented by a homogeneous population consisting of people having a professional or research link with the University of L’Aquila. Most of these people have a university degree or a high education level.
Gingivitis was perceived more in the group of those who tested positive. This finding could be linked to the general inflammatory response caused by the disease but also to the challenges of maintaining optimal oral hygiene during infection.
Another very interesting finding, which should be studied specifically, is linked to those with a family history of diabetes. Indeed, those with a family history of diabetes perceived a medium risk associated with COVID-19. We could indirectly hypothesize that these people already tested preventive measures during their ordinary lives.
The original outcome of this study is represented by these preventive habits, which have been associated with an increased risk of testing positive for COVID-19 infection in a homogeneous population of university workers in Italy, although with different job duties.
This study demonstrates that risk perception varies according to pathological conditions, that the habit of attending dental office is associated with a higher attitude to follow preventive measures, and that it is a better predictor of health promotion and preventive habits, and different tasks could be linked to a different probability of testing positive. Further research is necessary to understand these forms of different risk perception according to different categories to improve specific preventive protocols for the next pandemic events.
In a university environment, classified in Italy as a “medium risk” environment, different jobs are linked to different risks and risk perception.
CONCLUSION
In a homogeneous environment, such as that represented by a small-medium Italian University in Central Italy, the risk of testing positive for COVID-19 can vary according to different job positions and different academic roles.
Risk perception varies according to different job positions and different tasks in the same homogeneous environment, as it was underlined in other papers [27].
This study underlines the correlation between the risk perception toward COVID-19 and age and personal or family history of chronic diseases.
With regard to personal oral hygiene habits, attendance at dental offices and adherence to general home dental hygiene practices are positive and potentially protective factors. On the other hand, at the beginning of the COVID-19 pandemic, it was commonly believed that dental office attendance could be a risk factor for infection due to the production of aerosol-containing water, saliva, and blood. An important recent study investigated the inequalities regarding access to oral care, especially in a public dental system like the one in the United Kingdom [28].
This study demonstrates that even in a homogeneous environment, risk and its perception could vary because of different jobs and, subsequently, different relationships with the public. As already discussed, it is well known that the possibility of working with low or zero direct contact with other people was linked to the consciousness of a low infection risk.
LIST OF ABBREVIATIONS
| SDs | = Standard Deviations |
| IQR | = Interquartile Range |
| ORs | = Odds Ratios |
| AIC | = Akaike Information Criterion |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Institutional Review Board of the University of L’Aquila, protocol number 39858.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures were conducted in accordance with the Helsinki Declaration.
CONSENT FOR PUBLICATION
All participants were involved voluntarily after providing informed consent.
AVAILABILITY OF DATA AND MATERIALS
The data mentioned in the manuscript are available on Institutional Microsoft Form platform and on Occupational Health Service Database of the University of L'Aquila; data were also obtained with "Ateneo in Salute" Project, described in our paper.
ACKNOWLEDGEMENTS
Declared none.


