All published articles of this journal are available on ScienceDirect.
Computer-guided Surgery in Anterior Esthetic Area with Autologous Deciduous Tooth-Derived Material: Case Report
Abstract
Background
The literature has described several biomaterials for guided bone regeneration. Some authors have proposed using a material derived from dentin/ enamel among autologous biomaterials. This study aims to test the effectiveness of autologous material derived from deciduous teeth in guided bone regeneration.
Case Presentation
A 24-year-old female shows up with missing tooth #1.1 for a domestic accident. This requires implant-prosthetic rehabilitation. It is decided to be performed before implant therapy, a bone regeneration guided using biomaterial resulting from the patient’s deciduous teeth stored in a plastic box. GBR (Guided Bone Rehabilitation) is performed, and after 6 months, the implant is inserted by computer-guided surgery, and then a provisional prosthesis is placed.
Discussion
The material deriving from deciduous teeth, not preserved with precautions, has had excellent integration results. This allowed the implant to be placed in the best position for the final prosthetic rehabilitation.
Conclusion
This clinical case shows that using biomaterial derived from deciduous teeth has allowed an excellent result with negligible biological cost.
1. INTRODUCTION
Edentulous rehabilitation has revolutionized dentistry and significantly increased the life quality of patients [1]. As a result of the loss of the dental element, the alveolar bone undergoes resorption due to the loss of its function [2]. To obtain a good predictability of implant survival, enough bone around the implant is necessary. Several therapeutic options have been proposed over the years to solve the problem of bone insufficiency and to increase bone availability for subsequent implant-prosthetic rehabilitation [3, 4]. As reported by the literature, after extraction, there is a healing of the post-extractive site divided into several stages, starting with the formation and stabilization of the clot and ending with the recall of osteoblasts to form new bone tissue [5]. After the bone rehabilitation phase, a reduction in the residual bone quantity is determined more and more with time, determined by the loss of function of the post-extractive site. Bone resorption is mainly buccal palatal in the first months and greater in the molar region [6] than in the anterior one. The resorption in the anterior region is less challenging to manage as it is within the aesthetic zone. Especially in the maxillary region, the anterior teeth are often almost exclusively covered only by bundle bone [7]. The resorption remains, however, also linked to the surgical trauma of the extraction, the amount of bone present (bundle bone), the quality of the periodontal ligament, and genetics. For this reason, there is often insufficient residual bone to insert an implant fixture, which can allow the rehabilitation of the edentulous site.
In fact, unlike when the dental element is present, there should be at least 1.5 - 2 mm of bone for the implant, both vestibular and palatally/ lingually [8]. For this purpose, numerous guided bone regeneration techniques (GBR) and biomaterials with different functions (osteo- conduction, osteoinduction) have been described according to the type of biomaterial used. Some properties must have an ideal biomaterial: 1) osteoconduction, the ability to create a scaffold on which the cells can apply to begin the formation of the organic matrix initially, which will then be mineralized. Osteoconduction is an ability that can never be missed because, without support, the cells already present and the stem cells stimulated would not be able to create new tissue; 2) osteoinduction, on the other hand, is the ability to differentiate mesenchymal stem cells into chondrogenic or osteogenic cells that possess different growth factors, the most known of which are the BMP (morphogenetic proteins of bone).
These molecules are released from the same cellular component of bone, and they are divided into osteo- inductive factors, which stimulate stem cells towards the osteoblastic line, and growth factors, which stimulate the proliferation of already differentiated cells. Other proteins involved in the osteoinduction process are insulin-like growth factors (IGF-1 and IGF-2) and transforming growth factors (TGFbeta-1 and TGFbeta-2). To be defined osteoinductive, a material must be able to induce such differentiation even in areas where such behavior is unusual (heterotopicalosteoinduction), such as muscle tissue, as well as in skeletal sites (orthoto- picalosteoinduction); 3) osteogenesis, the formation of new bone by the vital cells, mainly osteoblasts, present in the graft. Each vital bone graft promotes it, then is taken directly from an extra or intra-oral site of the same patient (quote). From a histological point of view, there are no significant differences in literature between these materials [9]. Regarding certain surgical procedures for bone tissue augmentation, some scientific papers claim that autologous material is more effective than others [9, 10]. Some authors propose grafting autologous material composed of enamel and dentin from the tooth [11].
Human dentin has similar osteointegration charac- teristics to human bone [12, 13]. After demi- neralization, both demineralized-dentin-matrix (DDM) and mineralized bone matrix (DBM) are mainly made up of type I collagen (90%) and non-collagenic proteins for the remaining 10%. They consist of non-collagenic proteins such as osteo- pontin, osteocalcin, sialoproteins, and phosphoproteins that are an active part of the process of bone calcification. These include growth factors, morphogenetic proteins (BMP), and LIM mineralization protein 1, which give the tooth osteoinductive properties [13-16]. This study aims to verify the effectiveness of dentinal autologous material deriving from the deciduous tooth in guided bone regeneration (GBR) for insertion of implants.
2. METHODS - CASE PRESENTATION
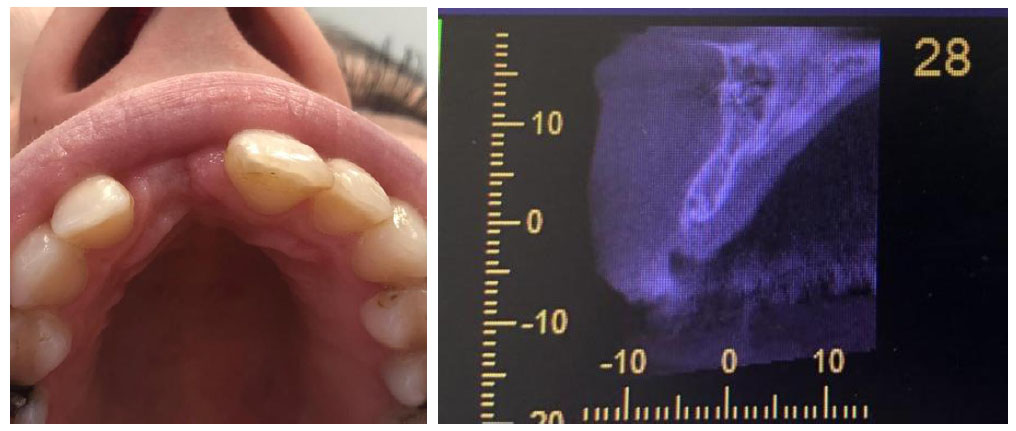
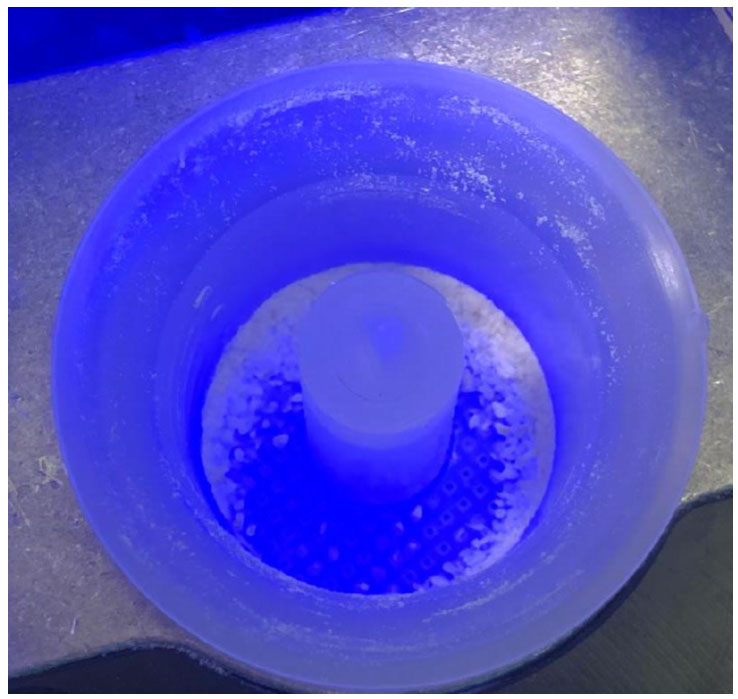
The subject of our study is a 24-year-old non-smoker female, ASA-1 (according to the classification of the American Society of Anesthesiologists), proficient in understanding the information provided. Her request is to rehabilitate through implant-prosthetic therapy the tooth #1.1 (central maxillary incisor) that is missing due to a domestic accident. The patient is evaluated with objective examination and through CBCT; from these analyses, it is possible to appreciate the lack of sufficient bone in a vestibule-palatal sense to allow the insertion of an implant (Fig. 1a and b). In this case, therapeutic possibilities were limited. The operator proposed a horizontal guided bone regeneration and, once healing was achieved, the insertion of an implant to support a fixed prosthesis. The patient has approved the therapeutic proposal, allowing the use of her deciduous teeth (kept in a plastic container for about 20 years) as an autologous material for grafting (Fig. 2). The patient consented to the proposed therapy and photographs for educational and research purposes. The use of deciduous teeth results from the fact that the patient would like to use material derived from her organism and not heterologous material. For this reason, the choice with the lower biological cost is to obtain autologous biomaterial from deciduous teeth that the patient lost in the phase of physiological exchange around 7 years. The patient signed informed consent before surgery. Before the surgery, professional hygiene and scaling were performed on the gingival. During the surgical act, after preparing the patient, local anesthesia was infiltrated with 1:100'000 adrenalin in position 1.1. A full-thickness flap was performed to allow access to the bone tissue. Subsequently, bone regeneration was performed guided by the biomaterial obtained from the patient’s deciduous teeth. For the use of deciduous teeth as an autologous graft, the following protocol was followed: 1) the teeth were cleaned and the absence of demineralization or carious lesions verified; 2) the teeth were dissected by the operator using a bur 3) teeth were chopped, demineralized, and sterilized through the Tooth Transformer instead, using an automated procedure. Material with an approximate weight of 1.5 g was obtained (the granules have an average diameter of 0.4 - 0.8 mm) (Fig. 3). Surgical sutures 4-0 are applied. Post-operative instructions are given, prescribing mouthwash containing 0.20% chlorhexidine twice daily for 15 days and using an analgesic such as paracetamol when needed. After 6 months from the GBR, a CBCT is performed to evaluate bone healing and program the implant insertion (Fig. 4a-d). From computed tomography, it is possible to observe the formation of new osteoid tissue in zone 1.1 that allows the insertion of an implant 3.5 x 11.5 mm (T3, 3i). Implantation is performed by static computer-guided surgery. Pre-chirurgical design is carried out using software (Navimax, Biomax). To carry out the design on the computer, the DICOM files of the CBCT acquired with radiological markers of known shape (Navibite, Biomax) and STL files obtained by intra-oral scanning of the patient’s arcades were coupled. Through the computer design of the implant-prosthetic rehabilitation of the site, a surgical template is built that allows, through the bushing, the implant to be inserted in the best position to obtain the best emergency for future prosthesis. The guide will enable you to insert the implant with a flapless method, drastically reducing swelling and post-operative pain and with more accuracy. The surgical template is produced in Peek with dental support to eliminate the possibility of tissue resilience and, at the same time, any precision errors determined by the positioning of the surgical guide itself.

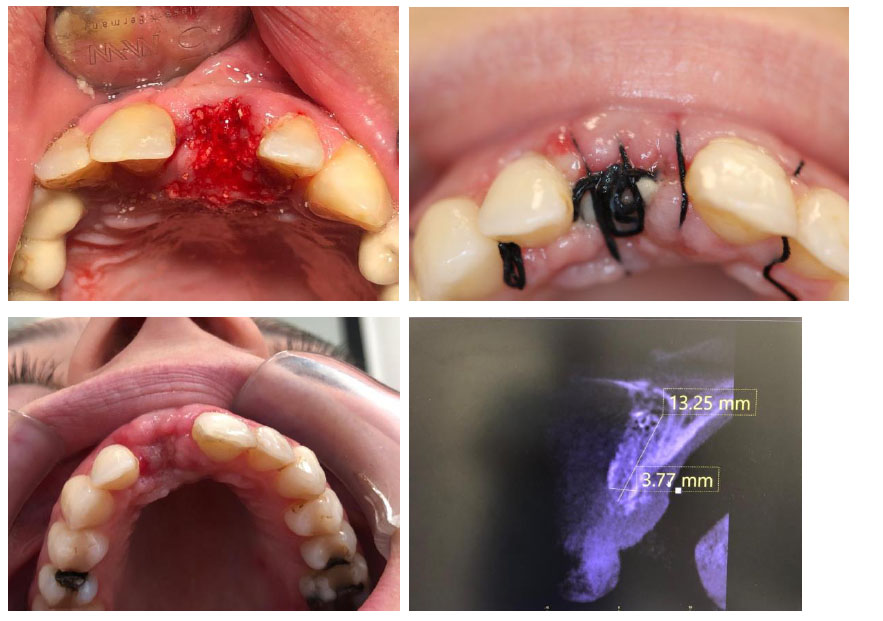

An accessory hole is also inserted under the template that allows the passage of the cutters to irrigate them during the preparation of the implant site. Once the implant is inserted, the non-resorbable suture is performed. Despite having obtained excellent primary stability, we prefer to wait for the full osseointegration of the implant and opt for a delayed load. A Maryland bridge is placed to fill the space, waiting for the implant to be loaded with fixed dentures (Fig. 5a and b).
3. RESULTS AND DISCUSSION
The study shows how deciduous teeth, even if preserved without special precautions, can be used as grafting material with excellent integration results and clinical outcomes to allow the execution of GBR. For this study, we used autologous material because the patient did not want animal material to be used. Using her deciduous teeth allows us to eliminate any biological and economic costs. Based on research by Schmidt-Schultz and Schultz in 2005 [17], we can say that the mineral and non-mineral components of the tooth did not change in the past period before using deciduous teeth as autologous material for GBR. These positive results are supported by studies describing similar cases using deciduous and permanent teeth. In 2018, a review of the literature was published by Gual-Vaqueset et al. [16] to evaluate the use of teeth as implant material before implantation. In this study, where 182 implants were analyzed, the authors defined the safe and effective use of such materials for bone augmentation where necessary [16]. In 2020, a case report published by Minetti et al., aimed at evaluating the use of autologous material from deciduous teeth for alveolar preservation (ARP) [12], shows that the use of this material also, from a histological point of view has excellent features of osseointegration and clinical outcome. In 2022, Minetti et al., in a study, analyzed 101 histological samples of 96 patients, assessing the increased amount of bone tissue, residual autologous material, and viable bone. Through this histological analysis, the authors argue that using autologous material from teeth has a predictable procedure and allows the creation of new vital bone that can support dental implants.
Furthermore, guided implant surgery translates into a more focused preoperative case study period, during which the implant position can be selected based on the patient's anatomical situation using 3D imaging software. This significantly reduces the risk of error during surgery, avoiding damage to nerves, sinus cavities, and adjacent dental roots, and allows the surgeon to operate with greater safety using the “flapless” technique. Therefore, implant placement can be performed with faster operating times (especially for complex cases) and minimally invasive methods that promote the patient's post-operative recovery without significant symptoms or discomfort. In addition, placing an implant in the correct position allows the best prosthetic crown to be loaded.
CONCLUSION
In conclusion, using deciduous teeth is a valid alternative to autologous material with a lower biological cost than other techniques for collecting autologous material. In addition, excellent maintenance of the deciduous teeth could increase the quality of the biomaterial produced, resulting in greater effectiveness in the guided bone regeneration or the preservation of the post-extractive alveolus. Further studies are needed to confirm what this study and others have proven.
LIST OF ABBREVIATIONS
| DDM | = Demineralized-dentin-matrix |
| DBM | = Mineralized Bone Matrix |
| IGF-1 and IGF-2 | = Insulin-like Growth Factors |
| TGFbeta-1 and TGFbeta-2 | = Transforming Growth Factors |
| ARP | = Alveolar Preservation |
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.


