All published articles of this journal are available on ScienceDirect.
Cuspal Deflection and Marginal Integrity of Class II Cavities Restored with Bulk-fill Resin Composites
Abstract
Objective:
This laboratory study aims to assess the cuspal deflection, adaptation, and marginal sealing of premolars restored with bulk-fill resin composites.
Methods:
Fourty-four premolars received class II preparations (distal and mesial boxes located 1 mm above and 1 mm below the cementoenamel junction, respectively). The teeth were distributed into four groups according to the resin composite used for restoration (n=11): G1 (control): Filtek Z250 XT; G2: Filtek Bulk-Fill; G3: Tetric N-Ceram Bulk-Fill; G4: Aura Bulk-Fill. A digital micrometer was used to measure the cuspal deflection before and after the restorative procedures. Replicas in epoxy resin of the restored teeth were achieved before and after thermal cycles. The cervical margins were observed by SEM at 200x magnification to obtain the percentage of continuous margins (%CM). After thermal cycles, the samples were immersed in a silver nitrate solution, and the microleakage was analyzed in the cervical margins.
Results:
ANOVA showed no significant differences in the cuspal deflection and %CM among the resin composites. Student’s t-test showed a significant decrease in the %CM after thermal cycles for all resin composites at the cervical margin in dentin. There was higher microleakage at the dentin margin for all the resin composites.
Conclusion:
Bulk-fill resin composites had comparable behavior to a conventional composite in regard to the cuspal deflection, adaptation, and marginal sealing parameters.
1. INTRODUCTION
The application of thicker increments in the tooth cavity, such as 4 to 5 mm, is possible when bulk-fill resin composite is used. There was an increase in the translucency of the material or an incorporation of new photoinitiators for effective polymerization. The chemical composition also had modifications to reduce the volumetric shrinkage arising from the polymerization of the material [1]. This volumetric shrinkage generates stresses at the tooth interface because the resin composite is bonded to the tooth structures by an adhesive system [2].
One factor related to polymerization shrinkage is the inward cuspal deflection in mesio-occlusal-distal (MOD) cavities [3]. Some studies showed that bulk-fill resin composites presented smaller cuspal deflection in comparison with conventional resin composites [3-5] and other studies demonstrated no significant difference in the total deflection among the materials [6-8]. Therefore, the results are conflicting.
Another relevant factor associated with stresses generated by polymerization shrinkage is the sealing of the margins. The sealing of the margins is affected by the intensity of the shrinkage stresses during photopolymerization, which is a relevant issue for the longevity of resin composite restorations. Clinically, stresses can be transmitted to the margins of the restoration and influence the marginal integrity [9]. Most studies showed that bulk-fill materials did not have a negative influence on marginal integrity [10-12]. However, regardless of the resin composite used for restoration, it is important to apply a well-performing adhesive to achieve good bonding quality between the tooth structures and resin composite [11]. Nowadays, there is a tendency towards the use of universal adhesives [13], and the adhesive must withstand the shrinkage stresses during resin composite polymerization [14].
In MOD cavities with cervical margins at dentin, marginal adaptation is a challenge [10], because the adhesion procedure for the dentin is complex [15]. The shrinkage stresses caused by polymerization can reduce the bond strength between the tooth and resin composite [14] and interfere with the adhesive interface, favoring greater or reduced infiltration [16]. The integrity of the margins and absence of leakage seem to be the most relevant criteria that determine the durability of a restoration [10].
The combination and sum of different factors, such as cuspal deflection, marginal adaptation, and marginal infiltration, can contribute to the emergence of postoperative sensitivity, secondary caries and pulp inflammation [17]. In addition, not all conventional or bulk-fill resin composites perform similarly in MOD cavities [3]. Even though resin composites are widely studied, the scientific literature lacks studies evaluating these three relevant outcomes; cuspal deflection, marginal adaptation and marginal infiltration, in the same study for high-viscosity bulk-fill resin composites under the same universal adhesive system. Therefore, this laboratory study aimed to assess, in vitro, the cuspal deflection, marginal adaptation and marginal sealing of MOD cavities restored with three bulk-fill resin composites and one conventional resin composite using the same universal adhesive system. This study was conducted under the null hypothesis that there are no significant differences in the (i) cuspal deflection, (ii) marginal adaptation, and (iii) marginal sealing among the evaluated resin composites.
2. MATERIALS AND METHODS
This research was registered by the local Ethics Committee (CAAE 89998518.7.0000.5336).
This laboratory study evaluated the resin composites shown in Table 1.
2.1. Sample Size Calculation
The general linear model determined the number of specimens. The means and standard deviations obtained in a pilot study were used in the total sample size calculation. A total of 44 teeth were necessary for the study. Eleven specimens (n=11) for each group were evaluated.
2.2. Teeth Selection
Sound maxillary first premolars, obtained after extraction due to orthodontic indication, were disinfected in 0.5% chloramine T for 24 h. A digital caliper (Mitutoyo, Suzano, SP, Brazil) was used to measure the buccolingual and mesiodistal distances of the teeth. A maximum difference of 0.5 mm in each distance was accepted [18]. In total, 44 teeth were selected.
2.3. Cavity Preparation
The root of the tooth was positioned in a cylindrical matrix that was filled with self-cured acrylic resin up to 2 mm below the cementoenamel junction (CEJ). The MOD cavities were created by a single operator. A conical diamond bur (no 2133) (KG Sorensen, Barueri, SP, Brazil) was selected to perform the proximal boxes, and a conical diamond bur (no 3131) (KG Sorensen, São Paulo, SP, Brazil) was selected for the occlusal boxes. The diamond burs were used at high speed with a water spray. The occlusal isthmus was 3 mm deep. The width between the buccal and lingual cavosurface angles was two-thirds of the buccal and lingual cuspal tip distances. The widths of the proximal boxes were one-third of the buccal and lingual surface distances of the tooth at the level of the gingival wall and 1.5 mm deep. The cervical margins at the distal boxes were placed 1 mm above the CEJ, and the cervical margin at the mesial boxes was placed 1 mm below the CEJ. The preparations had rounded internal line angles, and the cavosurface angles were approximately 90° [18]. A periodontal probe (Hu-Friedy, Chicago, IL, USA) was used to measure the final depth, with 5 mm in the mesial boxes and 3 mm in the distal boxes. In each of the five preparations, the diamond bur was replaced.
| Material |
Composition Filler Content (% W / vol) Organic Matrix |
Lot No. | Manufacturer |
|---|---|---|---|
| Filtek Z250 XT Microhybrid |
Filler - Zirconia/Silica. (0,01 µm -3,50 µm) 84,5% | 60% Matrix: UDMA, TEGDMA, Bis-GMA, Bis-EMA |
N895410 | 3M/ESPE, St. Paul, MN, USA |
| Filtek Bulk-Fill Nanoparticle |
Filler - Zirconia (4 a 11 nm) / Silica (20 nm) /ytterbium fluoride (100 nm) 76,5% | 58,4% Matrix: UDMA, AUDMA, AFM, DDDMA, |
N874606 | 3M/ESPE, St. Paul, MN, USA |
| Tetric N-Ceram Bulk-Fill Nanohybrid |
Filler - Barium/Silica/Aluminum; ytterbium fluoride (0,04 µm-3 µm) 77% | 55% Matrix: Bis-GMA, UDMA, Bis-EMA |
W83652 | Ivoclar-Vivadent, Schaan, Liechtenstein |
| Aura Bulk-Fill Nanohybrid/ Universal | Filler - Barium Alumino-Borosilicate and silica 65% | 81% Matrix: UDMA, Bis-EMA, Bis-GMA, TEGDMA |
170273T | SDI, Bayswater, Vic, Australia |
2.4. Cuspal Deflection Testing (first measurement)
All prepared teeth received two resin composite spheres approximately 1.5 mm in diameter. One sphere was bonded with adhesive to the cuspal vertex of the buccal cuspal, and the other sphere was bonded to the cuspal vertex of the palatal cuspal. The resin composite spheres served as reference points for a precision micrometer (Mitutoyo, Suzano, SP, Brazil), which was used for measuring the intercuspal distance [19]. The prepared tooth was positioned on a metallic base. Then, the micrometer was positioned on a metallic fixation device to ensure that its fixation was always in the same position for the cuspal deflection measurements. The micrometer was placed in contact with the composite resin spheres, and the distance between the two spheres was measured three times, and the average was obtained.
2.5. Restorative Procedures
The Single Bond Universal adhesive system (3M/ESPE, St. Paul, MN, USA) was applied using the selective enamel etching with 35% phosphoric acid for 15 s, followed by rinsing and drying. With the aid of a microbrush, the universal adhesive was applied actively on the enamel and dentin for 20 s and gently air-dried for 5 s, and light-cured with a Radii-Cal LED unit (SDI, Bayswater, Vic., Australia) at 1.100 ± 10 mW/cm2 for 10 s. The irradiance was measured by a radiometer (Model 100, Demetron Research Corporation, Danbury, CT, USA). The MOD cavities were restored with the Adapt SuperCap matrix system (Kerr Co, Orange, CA, USA). The proximal faces of the matrix were stabilized with low-fusion godiva and the cavities were restored: Group 1- Filtek Z250 XT resin composite (control): with the aid of a spatula, the material was applied obliquely to the cavity in 2 mm thick layers, without joining the walls, until the cavity was filled. The tip of the curing unit was positioned as close as possible to the occlusal surface of the tooth, and each increment was light-cured with a Radii-Cal LED unit for 20 s. The matrix was removed, the tip of the curing unit was positioned as close as possible to the distal and mesial surface of the tooth, and light-curing was repeated on the distal and mesial surfaces for 20 s. Group 2- Filtek Bulk-Fill resin composite: the material was applied to the cavity in a single increment of up to 4 mm in thickness with the aid of a spatula. Then, the resin composite was light-cured with a Radii-Cal LED unit for 20 s through the occlusal surface, being the tip of the curing unit as close as possible to the occlusal surface of the tooth. The rest of the cavity was filled with an additional increment of the resin composite, followed by light curing for 20 s. The matrix was removed, and light-curing was repeated on the distal and mesial surfaces for 20 s. Group 3- Tetric N-Ceram Bulk-Fill resin composite, and Group 4 - Aura Bulk-Fill resin composite: the restorations were performed as described for group 2. Sof-Lex Pop On flexible disks (3M/Espe, St. Paul, MN, USA) were used to finish and polish the restorations. The restorations were completed by a single experienced operator. Before starting the study, a short pilot study was conducted by the operator to train the cavity preparations and restorative procedures with the aim of standardization.
2.6. Cuspal Deflection Testing (second measurement)
After the restorative procedure, approximately 10 minutes were passed, and a new measurement of cuspal deflection was performed as previously described. The average distance of the resin composite spheres before the restoration was subtracted from the average distance of the spheres after the restoration. Thus, the cuspal deflection values were obtained. After obtaining the cuspal deflection values, the resin composite spheres were removed, and the restored teeth were stored in distilled water at 37 °C for 24 h.
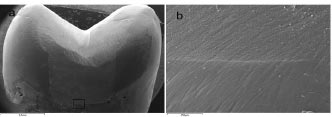
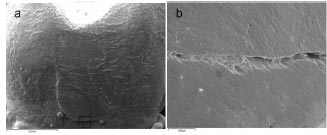
2.7. Obtaining Replicas
After the storage period, the teeth were molded with a polyvinyl siloxane material (3M ESPE St. Paul, MN, USA). An epoxy resin (Buehler, Lake Bluff, IL, USA) was poured into the molds to obtain epoxy resin replicas. The samples underwent 2,500 thermal cycles in water (5 and 55 °C with a dwell time of 30 s), and then a new set of epoxy resin replicas were obtained. The epoxy resin replicas were sputter coated (Balzers-SCD 050 Sputter Coater, Liechtenstein), and the cervical margins (mesial and distal) were evaluated by scanning electron microscopy (SEM) (Philips XL 30, Philips Electronic Instruments Inc., Mahwah, NJ, USA) at a magnification of 200x [18]. The values were expressed as a percentage of the continuous margins (%CM) over the total margin length for the cervical (distal and mesial) margins [18, 20]. The marginal analyses were performed by a blinded examinator.
2.8. Microleakage Analysis
After obtaining the replicas in epoxy resin, the teeth were covered with red nail varnish, except for the cervical restoration site and the surrounding 0.5 mm margin. The crowns were immersed in a 50% ammoniacal silver nitrate (AgNO3) solution for 24 h in a dark and closed environment. Afterwards, the silver nitrate of each tooth was removed by washing, and the crowns were immersed in a photo developing solution (Kodak, Rochester, NY, USA) under fluorescent light for 16 h [21].
After this period, the teeth were rinsed with water, and the nail varnish was removed with a scalpel blade. The teeth were cut in the mesiodistal direction using a water-cooled low-speed diamond saw (Extec Corp., London, UK) mounted on a laboratory-cutting machine (Labcut 1010, Extec Corp., London, UK), obtaining three portions from each tooth. In the sequence, the tooth portions were polished with 1000- and 1200-grit silicon carbide abrasive paper with manual pressure. A stereomicroscope (Olympus Corp., Tokyo, Japan) was used to observe the dye leakage (magnification of 25x) in the distal cervical margin (enamel) and mesial cervical margin (dentin). The tooth portion with the highest dye leakage was chosen for analysis. The dye microleakage was scored as follows: 0= no infiltration; 1= dye infiltration to half of the gingival wall; 2 = dye infiltration along the gingival wall; and 3 = dye infiltration along the gingival and axial walls. A blinded examinator performed the microleakage analyses [18].
2.9. Statistical Analysis
Cuspal deflection and %CM values were submitted to the Shapiro-Wilk normality test. As the values were normal (p>0.05), the cuspal deflection and %CM among the groups were analyzed by one-way ANOVA, followed by Tukey’s test. The %CM before and after thermal cycles was analyzed by a paired Student’s t-test. The microleakage data were analyzed by Kruskal-Wallis, followed by the Nemenyi test and Wilcoxon nonparametric tests. The statistical significance was set at 0.05.
| Groups | Cuspal Deflection (µm) | ±SD | p |
|---|---|---|---|
| Group 1 – Filtek Z250 XT | 14.1 | 3.41 | 0.127 |
| Group 2 – Filtek Bulk-Fill | 15.1 | 5.32 | - |
| Group 3 – Tetric N-Ceram Bulk-Fill | 19.0 | 3.49 | - |
| Group 4 – Aura Bulk-Fill | 17.0 | 6.22 | - |
3. RESULTS
3.1. Cuspal Deflection
According to one-way ANOVA, there was no significant difference in the cuspal deflection averages among the resin composites evaluated (p=0.127) (Table 2).
3.2. Marginal Integrity
According to one-way ANOVA, there was no significant difference in the %CM among the composite resins at the cervical margin in enamel (Table 3) and dentin (Table 4) (p>0.05). According to the Student’s t-test, there was no significant difference in the %CM before and after thermal cycling for all resin composites at the cervical margin in enamel (Table 3) (p>0.05). However, the Student’s t-test revealed a significant decrease in the %CM after thermal cycling for all resin composites at the cervical margin in dentin (p<0.05) (Table 4). Fig. (1a and 1b) show continuous margins at the cervical margin in enamel. Fig. (2a and 2b) show gap formation at the cervical margin in dentin.
| - | Cervical margin (enamel) | - |
|---|---|---|
| Groups | Before Thermal Cycles | After Thermal Cycles |
| Group 1 – Filtek Z250 XT | 100 Aa (0.00) | 92.6 Aa (10.2) |
| Group 2 – Filtek Bulk-Fill | 100 Aa (0.00) | 89.6 Aa (30.7) |
| Group 3 – Tetric N-Ceram Bulk-Fill | 95.3 Aa (9.5) | 87.2 Aa (12.3) |
| Group 4 – Aura Bulk-Fill | 97.4 Aa (11.3) | 85.5 Aa (22.8) |
| - | Cervical Margin (dentin) | - |
|---|---|---|
| Groups | Before Thermal Cycles | After Thermal Cycles |
| Group 1 – Filtek Z250 XT | 91.5 Aa (25.6) | 70.3 Ab (28,2) |
| Group 2 – Filtek Bulk-Fill | 87.7 Aa (20.6) | 66.9 Ab (29.4) |
| Group 3 – Tetric N-Ceram Bulk-Fill | 89.6 Aa (32.1) | 65.2 Ab (26.1) |
| Group 4 – Aura Bulk-Fill | 85.5 Aa (19.6) | 67.6 Ab (18.7) |
| Scores |
G1
Enamel Margin |
G2
Enamel Margin |
G3
Enamel Margin |
G4
Enamel Margin |
G1
Dentin Margin |
G2
Dentin Margin |
G3
Dentin Margin |
G4
Dentin Margin |
|---|---|---|---|---|---|---|---|---|
| 0 | 0% | 18% | 9% | 18% | 0% | 0% | 0% | 0% |
| 1 | 46% | 9% | 27% | 46% | 0% | 0% | 0% | 0% |
| 2 | 27% | 18% | 27% | 27% | 55% | 9% | 0% | 18% |
| 3 | 27% | 55% | 37% | 9% | 45% | 91% | 100% | 82% |
G2 – Filtek Bulk-Fill
G3 – Tetric N-Ceram Bulk-Fill
G4 – Aura Bulk-Fill
3.3. Marginal Sealing
The Kruskal-Wallis test showed no significant difference in the microleakage scores among the resin composites for the enamel margin (p=0.249). However, there was a significant difference among the resin composites for the dentin margin (p=0.010). The Nemenyi test showed a significant difference only between Filtek Z250 XT (45% of score 3) and Tetric N-Ceram Bulk-Fill (100% of score 3) at the dentin margin (p<0.05).
According to the Wilcoxon nonparametric test, there was no significant difference in the microleakage scores between the enamel and dentin margins for Filtek Z250 XT (p=0.0732) and Filtek Bulk-Fill (p=0.0538). However, there was a significant difference in the microleakage scores between the enamel and dentin margins for Tetric N-Ceram Bulk-Fill (p=0.0025) and Aura Bulk-Fill (p=0.0004). There was a predominance of score 3 in the dentin margin, and the microleakage was significantly higher in dentin than in the enamel. The microleakage score distribution is shown in Table 5.
4. DISCUSSION
The results showed that there was no significant difference in cuspal deflection among the resin composites evaluated. Thus, the first hypothesis was not rejected. This finding corroborates other studies that also found similarities in the cuspal deflection between high-viscosity bulk-fill and conventional resin composites [6-8]. In addition, a systematic review suggested a moderate potential of bulk-full resin composites for reducing stress [22].
The cuspal deflection is a phenomenon directly related to polymerization shrinkage that, associated with the adhesion of the resin composite to the cavity walls, generates shrinkage stresses and cuspal deformation [3, 8]. In the present study, the cuspal deflection was measured 10 min after the restoration was finished since cuspal deflection reaches a plateau 10 min after polymerization [7].
The polymerization shrinkage stress developed by the resin composite is also related to the photoactivation technique [23]. However, the present study used the continuous photoactivation method, as it is the most commonly used method in clinical practice. Another factor that influences the polymerization shrinkage is the elastic modulus of the resin composite [24].
The elastic modulus of the material depends on the chemistry and structure of the monomers, the percentage of fillers, and the interactions between the resin matrix and the fillers [24]. There is less deformation in materials with high elastic modulus, which produces more rigid restorations. This increases the effect of polymerization shrinkage on residual shrinkage stresses [2]. The elastic modulus is 12.3 GPa for Filtek Z250 XT [25], 8.86 GPa for Filtek Bulk-Fill, and 8.04 GPa for Tetric N-Ceram Bulk-Fill [26], and the elastic modulus of Aura Bulk-Fill was not obtained in the literature. Although the elastic modulus of Filtek Z250 XT was higher than the elastic modulus of Filtek Bulk-Fill and Tetric N-Ceram Bulk-Fill, these differences were not reflected in the significantly different values of cuspal deflection under the methodology applied. This finding can be related to the monomer percentage and organic matrix composition, as well as fillers characteristics that greatly influence the physico-mechanical properties of the resin composites [26]. For instance, all resin composites tested have urethane dimethacrylate (UDMA). It is attributed to UDMA a significant reduction in polymerization shrinkage due to its higher molecular weight that contributes to reduced shrinkage stress [27]. Despite the higher elastic modulus, it is possible that a higher percentage of UDMA in Filtek Z250 XT, in comparison to the other resin composites, has favored a reduction in the amount of contraction and stress zones that occur during the degree of polymerization.
Because polymerization shrinkage and cuspal deformation contribute to the appearance of cracks in enamel at the cervical level [28], it can be assumed that among the evaluated resin composites, none of them have a greater tendency toward forming cracks and, consequently, none of them have an increased risk of tooth fracture [28].
Restoring class II cavities is challenging, especially when the gingival margins are below the JCE. The results of the present study showed that there was no significant difference in the %CM among the resin composites, both before and after thermal cycles. Therefore, the second hypothesis was not rejected. In the enamel margin, there were 100% continuous margins for Filtek Z250 XT and Filtek Bulk-Fill, and above 95% for Tetric N-Ceram Bulk-Fill and Aura Bulk-Fill. One possible justification for the high %CM in the enamel may be the use of the Single Bond Universal adhesive system associated with selective enamel etching. Enamel etching with 37% phosphoric acid provides greater adhesive bond strength to this substrate [29]. The marginal adaptation is influenced by the magnitude of the polymerization shrinkage stress, and the shrinkage stress should not exceed the adhesive force at the substrate/resin composite interface to avoid gap formation [9]. Thus, greater bond strength between the adhesive and the enamel favors the maintenance and/or reduction of gap formation. In the dentin margin, there was a lower %CM in relation to the enamel margin. The Single Bond Universal adhesive system was applied in the self-etch mode on dentin. The greater formation of gaps is possibly related to the lower bond strength values of the adhesive to dentin because of the greater complexity of this substrate in the adhesion process [15].
The %CM was also verified after 2,500 thermal cycles. At both the enamel and dentin margins, there was a decrease in the %CM after thermal cycles. However, this reduction was statistically significant only for dentin. The smaller formation of gaps at enamel margins is related to the more effective adhesion obtained on enamel in relation to dentin, which prevents the formation of gaps after the thermal cycles [30]. In addition, phosphoric acid etching is the most reliable method for achieving a fatigue-resistant enamel bond [29].
Microleakage occurred both at the cervical margins located in dentin and enamel. However, the microleakage occurrence score of 3 was higher in dentin than in enamel. This finding is related to the greater gap formation in dentin, as the gap allowed the passage of tracer and, consequently, microleakage. This finding is in accordance with the literature, which shows that microleakage is greater in dentin [30, 31]. This is because dentin is a biological tissue with higher variability than enamel, and it is a challenge to achieve high bond strength to this substrate [15]. In addition, the universal adhesive system was applied on tooth substrates following the manufacturer’s instructions, which included gently air-drying for 5 seconds to evaporate the solvent. However, an extended solvent evaporation time, such as 15 s, could have improved the bonding effectiveness [32], contributing to better results of %CM and microleakage.
In the present study, there was a significant difference in the microleakage scores among the composite resins only in the dentin margin, with scores of only 2 and 3. Thus, the third hypothesis was rejected. A significant difference occurred in the dentin margins between Filtek Z250 XT and Tetric N-Ceram Bulk-Fill. Filtek Z250 XT was the composite resin with the highest microleakage score of 2 in dentin, and Tetric N-Ceram Bulk-Fill had the highest score of 3. Although there was no significant difference in the cuspal deflection average, coincidentally, Filtek Z250 XT obtained the lowest value (14.1 µm), and Tetric N-Ceram Bulk-Fill obtained the highest value (19.0 µm) of cuspal deflection. It is difficult to determine whether a difference of 5 µm in cuspal deflection is clinically significant. However, it cannot be ruled out that the largest cuspal deflection for Tetric N-Ceram Bulk-Fill contributed to the highest level of microleakage in this group.
According to the manufacturer, Tetric N-Ceram Bulk-Fill has an initiator called Ivocerin, an alternative photoinitiator based on germanium salt derivate [33]. This initiator has a higher photocuring activity than that of camphorquinone, enabling deeper polymerization and a higher bottom/top surface hardness ratio [34]. However, this initiator has a higher absorption spectrum in the 350- to 470-nm range compared to that of camphorquinone, and a multiwave LED light curing is recommended for photoactivation [33]. In the present study, a monowave LED light curing was used for all resin composites since most professionals still have this equipment in their offices. In addition, a systematic review concluded that the multiwave light curing units are useful but not essencial for activation resin composites containing alternative photoinitiators [35]. Although a monowave LED curing unit was used, the monomer-polymer conversion of Tetric N-Ceram Bulk-Fill generated polymerization shrinkage stresses when polymerized inside the cavity, favoring the highest value of cuspal deflection. In addition, if the polymerization of the material had not been adequate with the use of a monowave LED curing unit, worse results of marginal adaptation would be expected, and this finding was not confirmed, since there was no statistical difference in the %CM among the resin composites. However, it cannot be ruled out that a possible deficient polymerization of Tetric N-Ceram Bulk-Fill has contributed to a failure of bonding to dentin, justifying the high percentage of score 3.
The present study has the limitation of using only thermal cycles as an aging method. It would be relevant to include cyclic mechanical loading in future studies since restorations are submitted to chewing loads in the oral cavity. As a laboratory study, care must be taken to extrapolate the results to clinical reality, and clinical trials are necessary to generate better evidence on bulk-fill resin composites.
CONCLUSION
It can be concluded that restorations with bulk-fill resin composites obtained cuspal deflections and marginal adaptations similar to a conventional resin composite before and after thermal cycles despite the limitations of this in vitro study. In addition, none of the evaluated resin composite, in association with the same universal adhesive system, could avoid the microleakage process, which was higher in dentin than in enamel.
LIST OF ABBREVIATIONS
| MOD | = Mesio-occlusal-distal |
| CEJ | = Cementoenamel junction |
| SEM | = Scanning electron microscopy |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This research was registered by the local Ethics Committee (CAAE 89998518.7.0000.5336).
HUMAN AND ANIMAL RIGHTS
No animals were used in the study. All the human experimentation was performed according to the Helsinki declaration.
AVAILABILITY OF DATA AND MATERIAL
The data that support the findings of this study are available from the corresponding author, [A.M.S.], on special request.
FUNDING
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior — Brasil (CAPES) — Finance Code 001.
ACKNOWLEDGEMENTS
The authors thank the Central Laboratory of Microscopy and Microanalysis of PUCRS for the images of Scanning Electron Microscopy.


