Survival of Partial Laminate Veneers and Categorical Covariates Affecting the Survival: A Systematic Review
Abstract
Background:
Partial laminate veneers (PLV) have been accepted widely among both clinicians and patients with their favorable specifications, such as conservativeness, superior esthetics, bond strength and durability, for three decades. Various esthetic and functional impairments spreading in a wide range may be restored with veneers instead of full contour crowns.
Objective:
Although advantages, partial laminate veneers are not free from complications and various factors can influence the service duration of these restorations.
Methods:
An electronic Pubmed/Medline and Google Academic search was conducted without time restriction, providing information on porcelain laminate veneer’s failure rate and survival. Assessment of the identified studies was performed by two independent reviewers. Clinical service durations and various types of failures were evaluated.
Results:
Debonding, fracture, discoloration of the porcelain; staining or disintegration of tooth-porcelain margin; hypersensitivity, secondary caries, pulp necrosis and the periodontal responses were the more frequently studied failures. The mean CFR was found as 8,22% per study. Enamel substrate, incisal overlapping and lithium disilicate veneers presented lower failure rates in comparison with dentine substrate, non-overlapping and feldspathic veneers.
Conclusion:
PLV’s have high survival rates. The overall survival of PLV restorations can be affected by several prognostic variables.
1. INTRODUCTION
Partial laminate veneer (PLV) restorations have progressively increased in popularity for esthetic and functional improvement of the anterior teeth. They are durable and conservative anterior restorations with superior esthetics [1]. Treatment of unsightly appearance and esthetic reshaping of anterior teeth are accomplished using PLvs instead of full coverage restorations [2]. Tetracycline staining is the most frequent discoloration in reviewed literature, and various techniques aiming the resemblance of the discolored teeth with the natural tooth color by using PLvs have been described [3]. It was shown that their bonding performance to the discolored tooth substance was not influenced by discoloration [4]. PLvs were also used for the treatment of isolated microdontia and conoid lateral incisors [5, 6]. Closing diastemata is another most known indication of the PLvs. However, the proportions of the clinical crowns should be evaluated meticulously in order to avoid unsatisfactory results [7]. PLvs were also recommended for young adult patients as an alternative treatment option against the conventional full-coverage restorations requiring aggressive sacrification of the tooth structure as well as the health of the supporting tissues [8]. PLvs were either employed in non-orthodontic restorative correction of dental crowding or to complete the orthodontic treatment as a second phase of a sequential technique [9, 10]. Their use for the esthetic rehabilitation of misplaced upper anterior teeth was reported [11]. They were used in the correction of congenitally missing lateral incisors [12, 13]. The tooth transformation procedure, supported by additional wax-up and indirect mock-up techniques, was described [14]. PLvs were also used in prosthodontic treatment and rehabilitation of the esthetic and functional impairments of challenging cases such as amelogenesis imperfecta [15, 16]. Clinical service duration and quality were evaluated in several studies, and long-term success was documented. Although PLV restorations are widely known as a predictable treatment option that offers excellent results, the clinical service period of a PLV restoration may be ended, interrupted, or disqualified due to various failures. The aim of this systematic review was to search the literature regarding the survival of glass-ceramic PLvs and to evaluate the relationship between the failure types and clinical service longevity of these restorations.
2. MATERIALS AND METHODS
The present study followed the PRISMA statement guidelines [17].
2.1. Article Identification
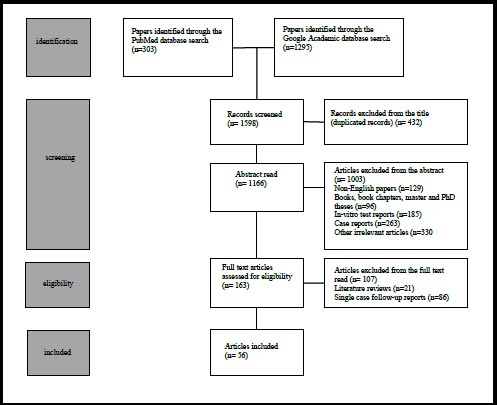
An electronic search without time restrictions was undertaken in May 2021in the PubMed/Medline and Google Academic databases by using the following keywords: “porcelain laminate veneer” OR “porcelain laminate veneer” AND “failure” OR “porcelain laminate veneer” AND “failure rate” OR “porcelain laminate veneer” AND “survival” OR “porcelain laminate veneer” AND “follow-up” OR “porcelain laminate veneer” AND “retrospective” OR “porcelain laminate veneer” AND “prospective.” A total of 1,598 articles were identified and screened.
2.2. Screening
Article identification, screening, eligibility, inclusion and exclusion assessments were performed by two reviewers independently. Of the 1,598 articles identified, 432 duplicates were excluded. Titles and abstracts of the remaining 1166 articles were evaluated. Non-English papers (n=129), books and/or book chapters, master and Ph.D. theses (n=96), papers reporting in vitro tests (n=185), case reports (n=263) and other irrelevant reports (n=330) were excluded. The remaining 163 articles have been assessed for eligibility.
2.3. Eligibility
Eligibility criteria included publications reporting clinical series of patients with PLvs without follow-up time restriction. Only clinical studies written in English and full text were considered.
Twenty-one literature review articles and 86 single-case follow-up articles were excluded. The remaining 56 studies were objected to for full-text reading and evaluation (Fig. 1). Two reviewers independently extracted the data using a standard Excell Worksheet prepared specifically for the present study. Included studies were evaluated for bias risk according to Critical Apprisal Skills Programme (CASP) checklist [18].
For each of the studies, year of publication, study design, number, age and gender of the patients, the number of the PLvs applied, follow-up period, clinical quality assessment protocols, survival rates and statistical software employed, independent prognostic variates, variate survivals, failure types and frequencies, were extracted when available.
3. RESULTS
3.1. Literature Search
Fifty six cohort studies which were published in a 31-year period between 1989 and 2020, were reviewed in the present study.
3.2. Test Population
There were a total of 3627 patients, with a mean of 64,76 patients per study. The number of patients differed from 10 [19] to 1170 [20, 21] among the reviewed reports (Table 1). Six studies [19, 21-26] were found, including 20 or less, 15 studies [27-41] between 21 and 50, and 13 studies [42-54] with 51–100 patients; six studies [55-60] with 101 to 500 patients; and two studies were found consisting more than 500 patients [20, 21]. The number of the followed patients has not been found in fourteen articles [61-74].
A total of 14726 PL vs were evaluated, with a mean of 262,96 PLvs per study. The number of PL vs followed varied from 22 [66] to 2562 [20, 21] among the reviewed reports (Table 1). Five studies [19, 35, 41, 64, 66] were found between 22 and 50 veneers, eight studies [22-25, 31, 36, 39, 40] between 51 and 100 veneers, seventeen studies [26, 27, 29, 30, 32, 33, 37, 38, 44, 53, 61, 62, 65, 70-72, 74] were found reporting between 101 and 250 veneers, eighteen studies [28, 34, 42, 43, 45, 47-52, 54, 55, 57-59, 63, 67] were found reporting 251 and 500 veneers, and six studies [20, 21, 46, 56, 60, 69] were found reporting 501 and more PLvs. The number of the followed veneers has not been found in two articles [68, 73]. The mentioned two articles were not included in tables in order that followed veneers numbers are uncertain.
| Author(s) Refs. | - | Year (months) | Patient | PLV | Evaluation | MeanFollow-up Survival (%) | - | Statistics | Overall |
| Datta & Sandhu [56] | 2020 | 156 | 536 | OHIS | - | 24 | - | Descriptive | 83,33 |
| Faus-Matoses et al. [42] | 2020 | 64 | 364 | Subjective | 36 | - | - | Kaplan-Meier | 93,70 |
| - | - | - | - | - | - | - | - | 60 | 91,00 |
| - | - | - | - | - | - | - | - | 96 | 87,10 |
| Arif & Denisson [27] | 2019 | 26 | 140 | Ryge | - | 84 | - | Kaplan-Meier | - |
| - | - | - | - | - | - | - | - | 168 | 98,00 |
| Yüce et al. [22] | - | 2019 | 12 | 61 | USPHS | - | 24 | Kaplan-Meier. 100,00 | - |
| Arif et al. [61] | - | 2019 | - | 108 | GI,GPD,GCF | 84 | - | - | - |
| - | - | - | - | - | - | - | ANOVA-Pearson. 43,00 | 168 | - |
| Rocha et al. [62] | - | 2019 | - | 183 | USPHS | - | 12 | Kaplan-Meier | 98,50 |
| Malchiodi et al. [24] | 2019 | 13 | 79 | 36 | - | Kaplan-Meier | 98,70 | - | - |
| Imbrugia et al. [43] | 2019 | 53 | 265 | CDA-Ryge | 54,4 | - | Descriptive | 99,63 | - |
| Aslan et al. [28] | - | 2019 | 41 | 364 | USPHS | - | 120 | Kaplan-Meier | 97,40 |
| Aslan et al. [63] | - | 2019 | - | 413 | - | - | 60 | Kaplan-Meier | 98,00 |
| - | - | - | - | - | - | - | - | 120 | 95,00 |
| - | - | - | - | - | - | - | - | 180 | 91,00 |
| - | - | - | - | - | - | - | - | 240 | 87,00 |
| Gresnigt et al. [64] | 2019 | - | 48 | USPHS | - | 120 | - | Kaplan-Meier | 100,00 |
| Gresnigt et al. [57] | 2019 | 104 | 384 | USPHS | - | 132 | - | Descriptive | 95,50 |
| Monaraks & Leevailoj [65] | 2018 | - | 163 | USPHS-FDI | 68,1 | - | Kaplan-Meier | 97,50 | - |
| Olley et al. [66] | - | 2018 | - | 22 | Subjective | 600 | - | Kaplan-Meier | 100,00 |
| Nejatidanesh et al. [44] | 2018 | 71 | 197 | CDA | - | 60 | - | Kaplan-Meier | 99,00 |
| Awan et al. [41] | - | 2018 | 42 | 42 | Ryge | - | 20 | Chi Square | 63,15 |
| Kazakova & Kirov [58] | 2018 | 152 | 283 | USPHS | - | 108 | - | Descriptive | 97,18 |
| Karagözoğlu et al. [25] | 2016 | 12 | 62 | Subjective | 24 | - | - | Kaplan-Meier | 100,00 |
| Granell-Ruiz et al. [45] | 2014 | 70 | 323 | Subjective | 84 | - | - | Kaplan-Meier | 87,00 |
| Alhekeir et al. [29] | 2014 | 29 | 205 | Subjective 24 | - | - | Chi-Square | 82,80 | - |
| Öztürk & Bolay [30] | 2014 | 28 | 125 | USPHS | - | 24 | - | Descriptive | 91,20 |
| Fabbri et al. [67] | - | 2014 | - | 318 | CDA | - | 42,1 | Kaplan-Meier | 100,00 |
| Guess et al. [31] | - | 2014 | 25 | 66 | USPHS | - | 84 | Kaplan-Meier | 100,00 |
| Gresnigt et al. [23] | 2013 | 20 | 92 | USPHS | 21,6 | - | Kaplan-Meier | 94,60 | - |
| Gresnigt et al. [19] | 2013 | 10 | 46 | USPHS | 20,3 | - | Kaplan-Meier | 93,50 | - |
| Gürel et al. [46] | - | 2013 | 66 | 580 | Subjective | 144 | Kaplan-Meier | 86,00 | - |
| Vailati et al. [26] | - | 2013 | 12 | 134 | USPHS | 50,3 | Descriptive | 94,60 | - |
| Beier et al. [47] | - | 2012 | 84 | 318 | CDA-Ryge | 60 | Kaplan-Meier | 94,40 | 120 |
| - | - | - | - | - | - | - | 240 | 82,93 | 93,50 |
| Beier et al. [48] | - | 2012 | 84 | 318 | CDA-Ryge | 60 | Kaplan-Meier | - | 97,30 |
| - | - | - | - | - | - | - | - | 120 | 93,50 |
| - | - | - | - | - | - | - | - | 240 | 78,50 |
| Beier et al. [49] | - | 2012 | 74 | 292 | Subjective | 124,25 | Kaplan-Meier | 100,00 | - |
| Gürel et al. [50] | - | 2012 | 66 | 580 | Subjective | 144 | Kaplan-Meier | 92,76 | - |
| D’Arcangelo et al. [32] | 2012 | 30 | 119 | USPHS | 84 | - | Kaplan-Meier | 97,50 | - |
| Layton & Walton [59] | 2012 | 155 | 499 | Subjective | 60 | - | Kaplan-Meier | 98,00 | - |
| - | - | - | - | - | - | - | - | 120 | 96,00 |
| - | - | - | - | - | - | - | - | 180 | 91,00 |
| - | - | - | - | - | - | - | - | 240 | 91,00 |
| Granell-Ruiz et al. [51] | 2010 | 70 | 323 | Subjective | 84 | - | Kaplan-Meier | - | 97,10 |
| Della-Bona & Kelly [21] | 2010 | 1177 2562 | E & Wghsr | 120 | - | - | Kaplan-Meier | 53,00 | - |
| Çötert et al. [33] | - | 2009 | 40 | 200 | Subjective | 18 | Kaplan-Meier | 93,80 | - |
| Aykor & Özel [34] | 2009 | 30 | 300 | USPHS | 60 | - | Chi-Square | 95,00 | - |
| Burke & Lucarotti [20] | 2009 | 1177 2562 | E & Wghsr | 120 | - | - | Kaplan-Meier | 53,00 | - |
| Guess et al. [35] | - | 2008 | 25 | 66 | USPHS | 60 | Kaplan-Meier | 97,50 | - |
| Layton & Walton [52] | 2008 | 100 | 304 | Subjective | 73 | - | Kaplan-Meier | 96,00 | - |
| - | - | - | - | - | - | - | - | 93,00 | - |
| - | - | - | - | - | - | - | - | 91,00 | - |
| - | - | - | - | - | - | 132 | - | 73,00 | - |
| Murphy et al. [36] | 2005 | 29 | 62 | Subjective | 60 | 156 | Descriptive | 89,00 | - |
| Chen et al. [69] | - | 2005 | - | 546 | Modified Ryge | 192 | Descriptive | 98,00 | - |
| Wiedhahn et al. [60] 2005 | 260 | 617 | Subjective | 108 | - | - | Kaplan-Meier | 98,00 | - |
| Fradeani et al. [37] | 2005 | 42 | 182 | CDA-Ryge | 144 | - | Kaplan-Meier | 94,40 | - |
| Smales & Etemadi [38] | 2004 | 50 | 110 | Subjective | 84 | - | Descriptive | 95,80 | - |
| Peumans et al. [39] 2004 | 25 | 87 | Subjective | 120 | - | - | Descriptive | 68,00 | - |
| Aristidis & Dimitra [53] | 2002 | 61 | 186 | Subjective | 60 | - | Descriptive | 98,40 | - |
| Printzel et al. [70] | 2001 | - | 239 | CDA | - | 71 | Chi Square | 100,00 | - |
| Dumfahrt & Schäffer [71] | 2000 | - | 191 | CDA-Ryge | 120 | - | Kaplan-Meier 96,00 | - | - |
| Fradeani et al. [40] | 1998 | 21 | 83 | USPHS | - | 72 | Descriptive | 98,80 | - |
| Shaini et al. [55] | - | 1997 | 102 | 372 | Subjective | 78 | Kaplan-Meier | (Low) | - |
| Nordbø et al. [72] | 1994 | - | 135 | Subjective | 36 | - | Descriptive | (Low) | - |
| Dunne & Millar [54] | 1993 | 96 | 315 | Subjective | 63 | - | Descriptive | 83,00 | - |
| Calamia [74] | - | 1989 | - | 115 | USPHS | - | Descriptive | (Low) | - |
3.3. Time Span
In the present review, the shortest mean follow-up time period was 12 months [62], while the longest was 600 months [66], among the reviewed studies (Table 1). Ten studies [19, 22, 23, 25, 29, 30, 33, 41, 62, 73] had a mean follow-up time period of less than 2 years, eleven studies [24, 26, 34-36, 43, 44, 53, 67, 69, 72] between 2 and 5 years, 19 studies [20, 21, 28, 31, 32, 38-40, 42, 45, 51, 54, 55, 58, 60, 64, 65, 70, 71] between 5 and 10 years, and 12 studies [27, 37, 46-50, 52, 57, 59, 61, 63] with 10–20 years. In reviewed cohort reports, only one study was found that followed the test population for more than 20 years [66]. The follow-up time has not been found in three articles [56, 68, 74]
3.4. Monitoring the Clinical Success
In most of the follow-up studies, clinical success was assessed and recorded objectively. United States Public Health System (USPHS) was used in seventeen papers [19, 22, 23, 26, 28, 30-32, 34, 35, 40, 57, 58, 62-64, 74]. USPHS was used in combination with the Federation Dentaire International (FDI) system in one study [65]. The FDI system alone was used in one study [25]. California Dental Association (CDA) System and/or Ryge System was used in eleven studies [27, 37, 41, 43, 44, 47, 48, 67, 69-71]. United Kingdom National Health System was used to monitor the clinical success of the veneers in three studies [20, 21, 68]. Oral Hygiene Index Simplified was used in one study [56]. On the contrary, objectively unstructured studies in which no system was used are not few [24, 29, 33, 36, 38, 39, 42, 45, 46, 49-55, 59-61, 66, 72, 73].
3.5. Statistical Evaluation
Kaplan–Meier life table analysis has been used in most of the reviewed articles to calculate the survival of restorations [19-25, 27, 28, 31-33, 35, 37, 42, 44-52, 55, 59, 60, 62-67, 71]. Chi-square analysis [29, 34, 41, 52, 70, 71], Cox regression analysis [27, 46], ANOVA and Pearson Test [61], Kruskal–Wallis and Mann–Whitney U tests [62],Mantel–Cox Log Rank [23, 33, 44, 49, 59, 64, 67] were also used. Numerous studies have also used descriptive statistics instead of survival analysis [26, 30, 36, 38-40, 43, 53, 54, 56-58, 69, 74] (Table 1).
3.6. Overall Survival
According to Burke and Lucarotti [20], PLV is an elective restoration, often placed in the absence of disease for purely aesthetic reasons. As such, it would appear desirable that the success rate of the technique was 100%, although this is rare. Mean overall survival in reviewed literature was calculated as 90,81% regardless of the follow-up time interval.
Articles from the early period before 2000 indicated a relatively lower overall survival rate [55, 72, 74]. Lower survival rates were attributed to the effects of existing restorations and inexperienced operators [54, 55], adhesive material and technique [37], and incompetency of the materials and methods, such as luting of the feldspathic PLvs to the unprepared teeth [55, 72]. Recent studies reveal higher survival rates. In the present review, five studies reported overall survival rates of 43% and 80% [20, 21, 39, 41, 61], and six studies reported between 81% and 89% [29, 36, 45, 46, 54, 56]. The number of studies reporting overall survival in 90%–95% is ten [19, 23, 26, 30, 33, 34, 37, 38, 50, 57], and between 96 and 99 is fifteen [24, 28, 32, 35, 40, 43, 44, 51, 53, 58, 60, 62, 65, 69, 71].Eight articles reported 100% overall survival [22, 25, 31, 49, 64, 66, 67, 70]. A close relationship between the time and the survival rate can be seen in some studies [27, 42, 47, 48, 52, 59, 63]. Aslan et al. [63] reported the survival rates of PLvs after 60, 120, 180, and 240 months as 98%, 95%, 91%, and 87%, respectively. Beier et al. [47] reported survival rates of 94.4%, 93.5%, and 82.93% after 60, 120, and 240 months, respectively. Another study of Beier et al. [48] reported survival rates of 97.3%, 93.5% and 78.5% after 60, 120 and 240 months, respectively. Layton and Walton [59] reported survival rates of 98%, 96%, 91%, and 91% after 60, 120, 180, and 240 months, respectively. However, 5 years before this study, the same survival rates were 96%, 93%, 91%, and 73%, respectively (Table 2) [52]. Arif et al. [27] followed 140 PLvs for 84 and 168 months. The survival rate was 98% after 168 months, but the 84-month survival rate was not specified. However, it was mentioned that the survival rate decreased over time. The overall survival of PLV restorations can be affected by several prognostic variables. These variables, such as the substrate tissue [30, 33, 46, 50, 51, 62, 69], preparation [25, 62, 74], incisal preparation configuration [30, 31, 33, 38, 49, 70, 72], proximal preparation [33], apical finishing level [33], abutment vitality [33, 48, 57], existing restorations [23, 57], veneer material [19, 22, 44, 64, 67], extensions [24, 35, 46], type of resin cement [48, 62], bonding material and application types [34, 57, 58], application jaw [33], bruxism [42, 45, 47, 48], tobacco consumption [48] and operator skills and experience [29, 36, 62, 74] have been comparatively tested with a considerable number of cohort studies and their relationship with PLV failures were reported.
| Author(s) Refs. | - | CFR | DBN | FRC | CHP | DSC | MDC | MDI | BOP | GRC | HYS | EIR | SCR | ABF |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Datta & Sandhu [56] 16,67 | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Faus-Matoses et al. [42] | 6,30 1,90 7,70 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Arif & Denisson [27] | 4,38 | 2,00 4,35 5,26 | - | - | - | - | - | 2,00 | 4,00 | - | - | - | - | - |
| Yüce et al. [22] | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Arif et al. [61] | - | - | - | - | - | - | - | - | - | 27,00 | - | - | - | - |
| Rocha et al. [62] | - | - | 0,54 | 1,09 | - | 0 | - | - | - | - | 8,74 | - | - | - |
| Malchiodi et al. [24]. 1,30 | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Imbrugia et al. [43] 0,37 | 0,37 | - | - | 6,40 | 3,40 | - | - | - | - | - | - | - | - | - |
| Aslan et al. [28] | 1,64 1,09 | 0,55 | - | - | - | - | - | - | - | - | - | - | - | - |
| Aslan et al. [63] | 3,63 | 2,18 | 1,45 | - | - | - | - | - | - | - | - | - | - | - |
| Gresnigt et al. [64] | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Gresnigt et al. [57] | 4,98 0,78 | 3,90 | - | - | - | - | - | - | - | 0,26 | - | - | - | - |
| Monaraks & Leevailoj [65] 2,50 | 1,25 | 1,25 | - | - | - | - | - | - | - | 0,61 | 0 | - | - | - |
| Olley et al. [66] | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Nejatidanesh et al. [44] 1,0 | - | 1,0 | - | - | - | - | - | - | - | - | - | - | - | - |
| Awan et al. [41] | 36,83 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Kazakova & Kirov [58] | - | - | 0,35 2,12. 0,35 | - | - | - | - | - | - | - | - | - | - | - |
| Karagözoğlu et al. [25] | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | - | - | - |
| Granell-Ruiz et al. [45] | 13,0 | 9,00 | 4,00 | - | - | - | - | - | - | - | - | - | - | - |
| Alhekeir et al. [29] | 34,88 10,30 | - | 20,70 58,60 | 69,00 | 0 83,30 | 0,48 | - | - | - | - | - | - | - | - |
| Öztürk & Bolay [30] 8,80 | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Fabbri et al. [67] | 2,00 | 0,31 | 0,94 | 1,57 | - | - | - | - | - | - | - | - | - | - |
| Guess et al. [31] | - | 2,40 | 8,33 | 8,33 | - | - | 0 | - | - | - | 0 | - | 0 | - |
| Gresnigt et al. [23] | 5,40 | 1,08 | 2,17 | 1,08 | 13,79 18,39 | - | - | 21,73 | 0 | 0 | - | - | - | - |
| Gresnigt et al. [19] | 0 | 0 | 0 | - | 0 | 0 13,04 | - | - | 17,39 | 0 | 0 | - | - | - |
| Gürel et al. [46] | 3,44 | 0 | 3,44 | - | - | - | - | - | - | - | - | - | - | - |
| Vailati et al. [26] | 5,40 | - | - | - | - | - | 0 | - | - | 0 | 0 | 0 | - | - |
| Beier et al. [47] | 17,24 | - | - | - | - | - | - | - | - | - | - | - | - | |
| Beier et al. [48] | 17,24 | - | 13,05 | - | - | - | - | - | - | - | - | - | - | - |
| Beier et al. [49] | 6,84 | 0,34 | - | - | - | - | - | - | - | - | - | - | - | - |
| Gürel et al. [50] | - | 7,24 | 7,24 | - | - | 0 | 0 | 0 | - | - | 0 | - | 0 | - |
| D’Arcangelo et al. [32] | 2,50 | 0,27 | 0,54 | - | - | 4,20 | 2,50 | - | 2,19 | - | - | 0,27 | 0,27 | - |
| Layton & Walton [59] | 4,65 | - | - | - | 0,54 | - | - | - | - | - | - | - | - | - |
| Granell-Ruiz et al. [51] | 2,90 | 9,00 | 4,00 | - | - | 39,30 | 2,00 | 21,60 | 7,70 | 3,10 | 2,80 | 3,10 | - | - |
| Della-Bona & Kelly [21] | 47,00 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Çötert et al. [33] | 6,20 | 5,50 | - | - | - | - | - | - | - | - | - | - | 0,50 | - |
| Aykor & Özel [34] | - | - | - | - | 1,33 | 1,33 | - | 2,00 | - | - | - | - | - | - |
| Burke & Lucarotti [20] | 47,00 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Guess et al. [35] | - | 2,50 | 1,90 | - | - | - | - | - | - | - | 0 | 0 | - | - |
| Layton & Walton [52] 5,26 0,65 | 1,63 | - | - | - | - | - | 1,63 | - | - | 0,31 | 0,31 | - | - | - |
| Murphy et al. [36] | 11,00 | 6,00 | 5,00 | - | - | - | - | - | - | - | - | - | - | - |
| Chen et al. [69] | - | 1,00 | - | - | 0 | - | 1,00 | - | - | - | - | - | - | - |
| Wiedhahn et al. [60] | 2,00 | 6,0 | - | - | - | - | - | - | - | 3,80 | 2,60 | - | 2,00 | - |
| Fradeani et al. [37] | 5,60 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Smales & Etemadi [38] | 8,18 | - | 5,45 | - | - | - | - | - | - | - | - | - | - | - |
| Peumans et al. [39] | - | - | 11,00 | - | - | 19,00 | 20,00 | - | - | - | - | 10,00 | - | - |
| Aristidis & Dimitra [53] | 1,60 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Printzel et al. [70] | - | - | - | 1,25 | 8,78 | 1,25 67,00 | - | - | - | - | - | - | - | - |
| Dumfahrt & Schäffer [71] | 4,00 | - | 3,14 | - | - | 17,00 | 1,00 | 25,00 | 31,00 | - | - | - | - | - |
| Fradeani et al. [40] | 1,20 | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Shaini et al. [55] | “high” | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Nordbø et al. [72] | 5,18 | 0 | 5,18 | - | - | - | - | - | - | - | - | - | - | - |
| Dunne & Millar [54] | 17,00 | 11,00 | 8,00 | - | - | - | - | - | - | - | - | - | - | - |
| Calamia [74] | - | “low” | “low” | - | - | - | - | - | - | - | - | 0 | - | - |
3.7. Failures
The cumulative failure rate (CFR) was reported to be between 0 and 47% in the reviewed literature (Table 2). The mean CFR was found as 8,22% per study. Five studies reported 0 failures [19, 22, 25, 64, 66]. One study reported a CFR of less than 1% [43], while 19 studies reported a CFR of more than 1% but less than 5% [24, 27, 28, 31, 32, 35, 40, 44, 46, 51, 53, 57, 59, 60, 63, 65, 67, 69, 71]. The number of studies reporting a CFR between 5% and 10% is 11 [23, 26, 30, 33, 37, 38, 42, 49, 50, 52, 72]. Ten studies reported CFR values higher than 10% [20, 21, 29, 36, 41, 45, 47, 48, 54, 56].
Debonding, fracture, abrasion or discoloration of the porcelain; staining or disintegration of tooth-porcelain margin; hypersensitivity, secondary caries, pulp necrosis or fracture of the abutment tooth and the periodontal responses such plaque accumulation, gingival bleeding on probing (BOP) and recession; were found as PLV failures in the reviewed literature.
3.7.1. Debonding
In the present study, the mean rate of debonding was found as 3,22% per study. During the early days of PLV applications, debonding was accepted as the main failure of this type of restoration [40, 54, 55, 73]. Dunne and Millar [54] reported an 11% debond rate in 1993. Recent articles also reported lower debond rates. In the reviewed literature, four articles reported 0 debond [19, 25, 46, 72]. Six articles reported debond rates under 1% [32, 43, 52, 57, 62, 67]. Nine articles reported a debond rate under 5% but over 1% [23, 24, 27, 28, 35, 42, 60, 63, 65]. Debond rates between 5% and 10% have been reported in seven studies (Table 2) [31, 33, 36, 45, 49-51]. Debonding that does not end but interrupts the PLV service can be recorded as an “event” but may easily be recemented and not reduce the overall survival [33].
3.7.2. Porcelain Fracture
From minute edge cracks to gross fragments, porcelain fractures may occur in varying degrees [27, 42, 62]. In the reviewed literature, porcelain fracture rates were found to be between 0 and 13.05% (Table 2) [19, 23, 25, 27, 28, 31, 32, 36, 38, 39, 42, 44-46, 48, 49, 51, 52, 57, 60, 62, 63, 65, 67, 71]. The present study found the mean fracture rate as 3,65% per study. Porcelain fracture is the main reason for PLV failure, according to Beier et al. [47, 48]. Interaction between porcelain fracture and parafunctions was demonstrated [42, 45, 47]. In contrast with debonded PLvs, porcelain fracture ends the PLV overall survival. Generally, they cannot be repaired, and they should be remade [33]. Minor porcelain and/or enamel chips may break out of PLV restoration. Seven chipping events in the incisal finishing line were reported in 135 PLvs (5,18%) in a follow-up study in 1994 [72]. This rate is lower, as 1.08% and 1.57% in newer reports [23, 67]. Kazakova and Kirov [58] also noted 0.35% chipping in cemented with an acid-etching test group and 0 chipping in cemented with the laser-ablation test group. Chipping does not end or interrupt the service of the PLV but disqualifies the restoration service and esthetic performance.
3.7.3. Tooth Fracture
Tooth fracture is reported as a PLV failure in very few frequencies in the reviewed follow-up articles [32, 33]. D’Arcangelo et al. [32] and Çötert et al. [33] reported tooth fracture rates of 0.27% and 0.5% respectively. They concluded that the fracture incidence of the pulpless teeth was higher, and the difference was significant. Meanwhile, Layton and Walton [52] reported that 6% of the total failures are tooth fractures.
3.7.4. Discoloration
Shade and translucency of the porcelain, resin cement, and substrate tissue and the long-term durability of the color composition, have been mentioned as the factors dominating esthetic success [59]. In 1998, Fradeani reported that the color match of most of the 83 PLV was alpha after 6 years [40]. Similarly, staining of the 135 PLvs has been reported as negligible after 3 years [72]. In contrast, another retrospective study reported color change as the most common PLV failure (20,7%) [29]. In the present study, the mean rate of discoloration was found as 3,77% per study.
3.7.5. Marginal Staining
The thin resin composite cement line between the porcelain and tooth darkens routinely. In the present study, the mean marginal staining rate was found as 12,21% per study. However, the reviewed literature contradicted the marginal staining rate of PLV restorations. This rate was found in reviewed literature as 0 [19, 25, 31, 50], 1.33% [34], 3.4% [43], 4.2% [32], 13.79% [23], 17% [71], 19% [39], 39.30% [51], and 58.6% [29] in different studies (Table 2). Kazakova-Kirov [58] reported that they found less marginal discolorations in laser-ablated PLvs in comparison with acid-etched PLvs. Gresnigt et al. [57] and Beier et al. [47, 48] revealed that the difference in the marginal discoloration rates of the smoker and non-smoker patient groups is statistically significant in favor of non-smokers.
3.7.6. Marginal Disintegration
In the present study, the mean marginal disintegration rate was found as 4,96% per study. Marginal voids or defects were mostly met as small percentages, such as 0.35% [58], 1% [69, 71], 1.25% [70], 2% [51], and 2.5% [32]. However, Gresnigt et al. [23] reported an 18.39% marginal disintegration rate (Table 2). Kazakova and Kirov [58] reported no difference between the marginal disintegration rates of acid-etched and laser-ablated PLvs. In addition, Karagözoğlu et al. [25] reported that the marginal disintegration rate of the minimally prepared PLV group was significantly better than that of the prepless group. Peumans [39] also calculated a 20% marginal disintegration rate and noted that disintegration occurred, especially on existing composites. Guess et al. [35] advocated that the marginal disintegration rates of PLvs increase with extended time.
3.7.7. Gingival Bleeding on Probing
In the present study, the mean gingival bleeding on probing (BOP) rate was 30,76% per study. Gingival and plaque indices have been employed to monitor the gingival health status of PLV restorations for a long time [32], although the score of bleeding in probing has also been used in several studies (Table 2) [30, 32, 50, 71]. Dumfahrt and Schäffer [71] have recorded 25% gingival bleeding in probing. Granell-Ruiz et al. [51] also calculated a 21.6% gingival bleeding in probing. However, at 69%, the rate is much higher, according to Alhekeir et al. [29]. Arif et al. [61] also reported the periodontal health status of 108 PLvs after 198 months. They advocated that 43% of the patients had a normal gingival index, 15% had mild inflammation, and 46% had moderate inflammation and BOP. The pocket depth was found at 2.17% and 2.16% in the upper and lower PLvs, respectively. However, the difference was not significant.
3.7.8. Gingival Recession
The present study found the mean gingival recession rate as 9.93% per study. But in 2000, the 10-year gingival recession rate was 31% [71]. Layton and Walton [52] reported that gingival recession is 12.5% of the total failures of followed PLvs (Table 2). The gingival recession rate was also reported as 0 [29], 2.19% [32], 7.70% [51], and 27% [61].
3.7.9. Hypersensitivity
According to studies regarding PLvs, the absence of hypersensitivity is one of the major advantages of PLvs [55, 72]. Minimal invasive preparation procedures help in minimizing hypersensitivity. Hypersensitivity was reported to be 0 in most PLV follow-up reports [25, 26, 31, 35, 50]. Other articles reported hypersensitivity rates of 3.1% [51], 3.8% [69] and 8.74% [62]. Gresnigt et al. [19, 23] reported a hypersensitivity rate of 17.39% and 21.73%, respectively. Alhekeir et al. [29] also reported a relatively high hypersensitivity rate of 83.30% and attributed this rate to the insufficient skills of the operators (Table 2). The mean rate of hypersensitivity was found as 12,55% per study.
3.7.10. Pulp Necrosis
Although PLvs are performed with minimally invasive conservative preparations, all invasive procedures intervening in the structural unity of the teeth include the risks of vitality change and necrosis of the tooth pulp. Endodontic failures have been reported in very few frequencies such as 0 [19, 23, 25, 26, 35], 0.26% [57], 0.48% [29], 0.61% [65], 2% [27], 2.6% [60] and 2.8% [51]. The present study found the mean pulp necrosis rate as 0,79% per study.
3.8. Categorical Covariates
The above-mentioned failures were investigated by comparing the failure rate differences according to the selected independent categorical covariates in the reviewed literature (Table 3). Some of the covariates consider the preparation geometry, such as the preparation [25, 62, 70], substrate tissue [30, 33, 46, 50, 51, 62, 69], incisal preparation [30, 31, 33, 38, 49, 70, 72], proximal preparation [33], and apical finishing level [33]. Another group of covariates regards the abutment tooth, such as the abutment vitality [33, 48, 57], existing restorations [23, 57] and location [33]. Other covariates include materials such as veneer material [19, 22, 44, 64, 67], extensions [24, 35, 46], luting material [48, 62], bonding material, and application methods [34, 57, 58]. Finally, covariates regarding the patient and the operator, such as bruxism [42, 45, 47, 48], tobacco consumption [48], and operator skills and experience [29, 36, 62], were also found to be studied in the reviewed literature.
| Author(s) Refs. | - | Variables | - | - | - | - | - | Survival % | - | Sig. |
|---|---|---|---|---|---|---|---|---|---|---|
| Faus-Matoses et al. [42] | Splinteffect in bruxists | - | (with vs without splint) | - | - | 89,10 - 63,90 | - | + | - | - |
| Yüce et al. [22] | - | Porcelain type | - | - | (CAD-CAM vs heat pressed) | - | 100,00 -100,00 | - | - | - |
| Rocha et al. [62] | - | Substrate | - | - | (enamel vs dentine) | - | - | - | - | - |
| - | - | - | Resin cement type | - | - | - | - | - | - | - |
| - | - | - | Preparation | - | - | (feather edge vs prepless) | - | 98,50 - 93,50 | - | + |
| - | - | - | Operator experience | - | (experienced vs inexperienced) | - | - | - | - | - |
| Gresnigt et al. [64] | Veneer material | - | - | (porcelain vs indirect composite) | 100,00 - 75,00 | - | + | - | - | - |
| Gresnigt et al. [57] | Existing restorations | - | (with vs without) | - | - | 84,60 - 95,50 | - | - | - | - |
| - | - | - | Immediate dentine sealing | (sealed vs not-sealed) | - | - | 96,40 - 81.80 | - | + | - |
| - | - | - | Tooth vitality | - | - | (vital vs pulpless) | 95,60 - 88,10 | + | - | - |
| Nejatidanesh et al. [44] | Porcelain type | - | - | (Empress CAD vs Emax CAD) | - | 97,80 -100,00 | - | + | - | - |
| Awan et al. [41] | - | Discolored endotreated teeth | (PLV vs ceramometal) | - | - | 63,15 - 78,26 | - | - | - | - |
| Karagözoğlu et al. [25] | Prep. Depth | - | - | (minimal vs prepless) | - | 100,00- 100,00 | - | - | - | - |
| Granell-Ruiz et al. [45] | Effect of bruxism | - | (bruxist vs non-bruxist) | - | - | - | - | - | + | - |
| Öztürk & Bolay [30] | Incisal prep. | - | - | (overlap vs bevel) | - | - | 85,70 - 94,00 | - | - | - |
| - | - | - | Prep. depth | - | - | (enamel vs min. dentine exposure) | - | - | - | - |
| - | - | - | - | - | (min. vs severe dentine exposure) | - | - | + | - | |
| Fabbri et al. [67] | - | Manufacturing | - | - | (layered vs monolithic) | - | 98,00–100,00 | - | - | - |
| - | - | - | Localisation | - | - | (anterior vs posterior) | 98,00–100,00 | - | - | - |
| Guess et al. [31] | - | Preparation | - | - | (overlapped PLV vs full veneer) | - | 97,60–100,00 | - | - | - |
| Gresnigt et al. [23] | Existing restorations | - | (with vs without) | - | - | 93,50- 96,00 - | - | - | - | - |
| Gresnigt et al. [19] | Veneer material | - | (porcelain vs indirect composite) | 87,00- 100,00 | - | - | - | - | - | - |
| Gürel et al. [46] | - | Substrate | - | - | (fully enamel vs enamel on margin) | - | - | - | - | - |
| - | - | - | Substrate | - | - | (enamel vs dentine) | 99,00- 94,00 | - | + | - |
| Coronal extension | - | (extended vs not-extended) | - | - | - | - | + | - | - | - |
| - | - | - | Apical extension | - | (extended vs not-extended) | - | - | - | - | - |
| - | - | - | Existing restorations | - | (with vs without) | - | - | - | - | - |
| - | - | - | Diastema | - | - | (with vs without) | - | - | - | - |
| - | - | - | Discoloration | - | - | (with vs without) | - | - | - | - |
| - | - | - | Abrasion | - | - | (with vs without) | - | - | - | - |
| Beier et al. [47] | - | Abutment vitality | - | (vital vs pulpless) | - | - | - | + | - | - |
| - | - | - | Effect of bruxism | - | (bruxist vs non-bruxist) | - | - | - | + | - |
| - | - | - | Tobacco consumption | - | (smoker vs non-smoker) | - | - | + | - | - |
| Beier et al. [48] | - | Abutment vitality | - | (vital vs pulpless) | - | - | - | + | - | - |
| - | - | - | Effect of bruxism | - | (bruxist vs non-bruxist) | - | - | - | + | - |
| - | - | - | Tobacco consumption | - | (smoker vs non-smoker) | - | - | + | - | - |
| Beier et al. [49] | - | Incisal preparation | - | (overlapped vs non-overlapped) | - | 86,70–100,00 | - | - | - | - |
| Gürel et al. [50] | - | Substrate | - | - | (80% enamel vs dentine) | - | - | + | - | - |
| Granell-Ruiz et al. [51] | Incisal preparation | - | (simplified vs functional) | - | - | - | - | + | - | - |
| Çötert et al. [33] | - | Localisation | (maxillary vs mandibular) | - | 97,50- 95,00 | Abutment vitality | (vital vs pulpless) | 94,80 - 93,30 | - | - |
| - | - | - | Substrate | - | - | (enamel vs min. dentine exposure) | 93,20 - 95,70 | - | - | - |
| - | - | - | Incisal preparation | - | (overlapped vs non-overlapped) | - | 97,80 - 84,70 | + | - | - |
| - | - | - | Proximal preparation | - | (chamfered vs sliced) | - | 96,30 - 87,40 | + | - | - |
| - | - | - | Cervical preparation | - | (supragingival vs infragingival) | - | 99,40 - 63,30 | + | - | - |
| Aykor & Özel [34] | Bonding | - | - | (total-etch vs self-etch) | - | - | - | - | - | |
| Guess et al. [35] | - | Veneer design | - | - | (overlapped vs full) | - | 97,50–100,00 | - | - | - |
| Wiedhahn et al. [60] Manufacturing | - | - | (heat-pressed vs CAD-CAMed) | - | - | - | - | - | - | - |
| Smales & Etemadi [38] | Incisal preparation | - | (overlapped vs non-overlapped) | - | 95,80 – 85,50 | - | - | - | - | - |
| Printzel et al. [70] | Veneer type | - | - | (PLV vs full veneer) | - | 100,00 -100,00 | - | - | - | - |
| Malchiodi et al. [24] Extension (extended vs not-extended) - | - | - | - | - | - | - | - | - | - | - |
3.8.1. Preparation
Early studies advocated that preparation of the abutment teeth is not compulsory [55, 72]. Recent reports agree that a minimally invasive preparation is required to obtain a suitable space for the restorative material, avoid hypercontour, eliminate the convex contours according to the path of insertion, cover the unesthetic stump color, permit the adjustment check, obtain an internal enamel tissue that can be etched properly, and obtain an atraumatic cervical finishing line [33]. Enamel thickness and age-related changes have been studied, and reparation depth has been reported in 0.3–1.0 mm for normal shaded teeth [70]. However, PLvs with and without abutment preparation have recently been compared, and statistically significant differences have been found regarding marginal and internal gap measurements [25, 62].
3.8.2. Substrate Tissue
The difference between the bonding performances of enamel and dentine tissues has been demonstrated by several retrospective studies (Table 3) [30, 33, 46, 50, 62]. The survival rates of PLvs bonded to enamel and dentine have been reported as 99% and 94%, respectively [46]. The survival rates of PLvs bonded to pure enamel and partially exposed dentine were reported as 93.2% and 95.7%, respectively, and the difference was insignificant [33]. The difference between the survival rates of the PLvs bonded to pure enamel tissue and those bonded to enamel and minimally exposed dentine was found statistically insignificant, while the difference between the survival rates of the PLvs bonded to minimally exposed dentine and those bonded to severely exposed dentine was significant [30]. When dentine exposure is necessary during preparation, enough sound enamel must be protected as much as possible to maintain a good bonding; to obtain maximum bond strength, the preparation margins should be on the sound enamel [33]. Some of the reports reviewed in the present review have considered the outline tissue as a categorical covariate (Table 3) [33, 46]. Gürel et al. [46] calculated the survival rate of the PLvs with preparations confined to the enamel and enamel but only at the margins as 99% and 94%, respectively. They concluded that PLvs have high survival rates when bonded to enamel, providing a safe and predictable treatment option that preserves tooth structure. Çötert et al. [33] calculated the overall survival rates of the PLvs confined on pure enamel, partial enamel, and dentine as 90.5% and 50%, respectively. The Aesthetic Pre-evaluative Temporaries technique has been described to keep the maximum quantity of enamel tissue [50]. Using this approach, 80% of the 580 PLV preparations have been confined to the enamel tissue. Over 144 months, 42 PLvs have failed, but when the preparations were limited to the enamel, the debond rate was reported to decrease to 0 [50]. Preservation of sound enamel tissue can also be maintained by the mock-up technique [22, 46, 59].
3.8.3. Incisal Preparation
Classically, four types of incisal preparations have been described [38]. According to the reviewed literature, with and without overlapped incisal preparations are more popular than the other two [29, 51]. According to a 3-year retrospective report of 135 PLvs without incisal overlapping, debonding was not recorded, while seven incisal chipping events were recorded [72]. Preparation without overlap has been advised as conservative, predictable, and successful. The 2-year survival rates of PLvs with and without overlap have been reported as 85,7% and 94%, respectively, and the difference was found insignificant [30]. In contrast, the 18-month survival rates of PLvs with and without overlap have been reported as 97.8% and 84.7, respectively, and the difference was found to be significant [33]. Guess et al. [31] compared the overlapped PLV with full veneers regarding overall survival and failures and found insignificant differences. Beier et al. [49] also compared the overall survival of overlapped and non-overlapped veneers after 60, 96, 120, 180, and 240 months and reported that the differences were statistically significant. Smales and Etemadi [38] also reported that the difference between overlapped and non-overlapped veneer survival rates is insignificant (Table 3).
3.8.4. Proximal Preparation
Preparation of the proximal chamfers is recommended in teeth with normal proximal contacts. In contrast, in diastema cases, proximal surfaces may require feathering [33]. Survival rates of the PLvs with chamfered and feathered proximal outlines were reported as 96.3% and 87.4%, respectively, and the difference was found to be significant (Table 3) [33].
3.8.5. Gingival Finishing Level
Creation of a mini-chamfer finishing line at the gingival margin level or above it has been advised, and the negative influence of the infra gingival finishing level on PLV survival has been demonstrated [33]. Survival rates of the PLvs finishing at supra and infra gingival levels were calculated as 99.4 and 63.3%, respectively, and the difference was found to be significant (Table 3) [33].
3.8.6. Vitality
A significantly higher failure risk of the non-vital PLV abutments compared with the vital ones was demonstrated (Table 3) [33, 47, 48, 57].
3.8.7. Existing Restorations
Recent studies showed that existing composite restorations may not be required to be replaced prior to the cementation of PLvs when the carious lesion is absent (Table 3) [23, 46, 57]. No significant influence of the presence of composite restorations was reported on the failure rates of the followed PLvs [46]. In addition, the survival rates of the PLvs luted to the intact teeth and the PLvs luted to the teeth with existing restorations were reported as 96% and 93.5%, respectively, and the difference was found statistically insignificant [23]. Therefore, an existing composite restoration of good quality is not required to be removed, but it is better to be surface-treated by silica coating and silanization prior to the luting of the PLV restoration [57].
3.8.8. Location
The overall survival rates of the upper and lower PLvs were found as 97.5% and 95%, respectively, and the difference was found significant [33], while mouth quadrant differences were found insignificant in another study [21, 67].
3.8.9. Veneer Material
Awan et al. [41] reported the overall survival of the ceramo-metal restorations and PLvs applied to the endodontically treated and discolored teeth as 78.26% and 63.15%, respectively, and the difference was found to be insignificant. Indirect veneers are made of several materials, including acrylic, composite, and various porcelain materials. The survival rates of the heat-pressed and CAD-CAMed veneers were found to be both 100% [22]. The overall survival of EmpressCAD and EMaxCAD veneers was reported as 97.80% and 100%, respectively, and the difference was found to be significant [44]. The overall survival of CAD-CAMed (Cerec) PLvs was calculated as 94%, and 98% of the survived restorations were classified as clinically acceptable after 9 years [60]. The authors advocated that the high survival rate and favorable clinical results would support the use of CAD-CAMed PLvs in clinical situations similar to those for laboratory-processed porcelain veneers (Table 3). Veneers of the anterior and posterior regions, made of veneered and monolithic lithium disilicate (LiDiSi) were followed for 42 months, and the survival rates were found to be 98% and 100%, respectively, and the difference was found to be insignificant [67].
The survival and clinical performances of porcelain and indirect composite laminate veneers were compared [19]. Three failures in the group of resin composite veneers were reported, but the difference between the survival rates was found to be insignificant. Minor voids and defects were observed in six of the composite veneers and three of the ceramic veneers. Slight staining at the margins (n = 3) and slightly rough surfaces were more frequently observed for the resin composite laminate veneers (n = 18) up to the final recall (Table 3). In another study comparing resin and porcelain veneers, the overall survival was 75% and 100%, respectively, and the difference was significant [64].
3.8.10. Luting Material and Technique
PLvs must be bonded with a correct adhesive technique to reach a successful survival rate [37]. Reviewed literature showed that the resin composite luting agents have been preferred for PLvs [19, 23, 29, 33, 34, 45, 62, 72]. A light-cured composite luting agent was preferred in a 7-year retrospective study [32]. The clinical performance of the PLvs cemented with light-cured hybrid composite (Z100, 3M-ESPE) to the teeth treated with total-etch adhesive (Scotchbond Multi-Purpose Plus, 3M-ESPE) and self-etch adhesive (AdheSE, Ivoclar-Vivadent) systems were compared. A statistically significant difference between the total-etch and self-etch groups was not found [34] (Table 3).
3.8.11. Extensions
PLvs may be used to extend tooth contours in any direction [46]. The effects of proximal, apical, or incisal extensions on PLV survival have been studied in the literature. It was shown that extensions in the incisal direction can increase the failure probability 2–3 times, while the extensions in the apical direction do not create any failure risk (Table 3) [46]. Malchiodi et al. [24] also reported that the difference between the survival rates of extended and non-extended veneers was insignificant.
3.8.12. Parafunctions
Parafunctions, mostly bruxism, may potentially affect the PLvs and other dental restorations [45]. The risk of failure was calculated as 7.7 times greater when associated with an existing parafunction (Table 3) [47, 48]. The survival rates of the PLvs of bruxist and non-bruxist patients were compared according to the presence or absence of ceramic failures such as cracks, fractures, and debonding [45]. It was concluded that bruxism activity should be recognized as a higher risk of failure in PLV applications (Table 3). Survival rates of the PLvs applied to bruxist patients were found to be 89.1% in the splint-wearer group and 63.9% in the non-splint-wearer group, respectively; the difference was significant [42].
3.8.13. Tobacco Consumption
The success rates of PLvs of smokers and non-smokers were compared, and a significantly greater marginal discoloration in the PLvs of the smoker patients was noticed [29, 43, 47, 48, 57, 59, 64].
3.8.14. Operator Skills and Expertise
Burke and Lucarotti [20] considered the factors associated with the need for re-intervention of teeth restored with PLvs. They scanned the data of 2562 PLvs in 1177 patients and collected the factors influencing PLV survival. They concluded that dentist factors did not appear to influence PLV survival after re-intervention. Rocha et al. [62] reported that operator skills and experience did not influence the survival of PLV. However, some of the papers reviewed in the present study indicated the influence of the skills and experience of the operator on the clinical performance of PLvs (Table 3) [29, 55].
4. DISCUSSION
In the present systematic literature review, it was aimed to investigate the survival of porcelain PLvs and categorical covariates affecting the survival. A total of 975 PLvs out of 14726 PLvs of 3627 patients were failed. The mean CSR in the reviewed literature was calculated as 90,81% regardless of the follow-up time interval. Debonding, fracture, abrasion or discoloration of the porcelain; staining or disintegration of tooth-porcelain margin; hypersensitivity, secondary caries, pulp necrosis or fracture of the abutment tooth and the periodontal responses such plaque accumulation, gingival BOP and recession; were recorded as PLV failures in the reviewed literature. Failure patterns of PLvs appear as the results of the interactions of the prognostic variables. Insufficient clinical examination of the patient, teeth, intermaxillary relations, and esthetic appearance may cause failures. Parafunctions; mostly bruxism, may potentially shorten PLV survival [29, 45, 47, 55]. Night guards were also advised to protect the PLvs against the harsh occlusal forces in bruxist patients [42, 45]. Consumption of tobacco products affects PLV restorations. The PLvs of smokers exhibit a significantly greater marginal discoloration rate [47].
PLV abutments may exhibit various clinical conditions, such as discoloration, carious defects, developmental anomalies, fractures, abrasions, and existing restorations. It may also require apical, incisal, or proximal extensions [24, 46]. The amount of sound enamel tissue remaining after the preparation procedure, dentine expositions, level, and direction of the functional forces were advised to be planned and managed preoperatively [29, 30, 33, 46]. Protection of an adequate amount of sound enamel tissue was observed to have a primary important role in the bond strength and survival of PLvs [25, 29, 30, 33, 46].
Clinical operations, especially invasive steps such as tooth preparation, should be performed for preoperative planning applications. The weakness of the bond strength of the dentine tissue in comparison with that of the enamel and the lower survival rates of the dentine-bonded PLvs in comparison with the enamel-bonded PLvs were demonstrated [33, 46]. Marginal finishing of the PLV is better to be conducted on sound enamel tissue, while overpreparation and dentine exposition have been performed intentionally [33]. Most of the reviewed reports agreed to lute PLvs with dual-cure resin composite cements. Long-term bond strength and survival rates of PLvs luted with self-adhesive cement remain questionable and require further investigation.
The aims of the finishing procedures were reported as the establishment of marginal integrity by reducing surface irregularities and polishing of the cement line exposed marginally [71], which may cause leakage, debonding, and gingival inflammatory response. The research reports reviewed in the present study agree that PLvs have little or no influence on periodontal health. Low rates of gingival disorders, such as recession and BOP have been reported [29, 30, 32, 50, 51, 71].
Despite the development of porcelains, bonding and luting agents, as well as the clinical techniques, skills, and experience of the operator still influence the overall success of PLV restorations. Relatively low survival rates of PLvs planned and performed by inexperienced or non-proficient operators such as students or dental interns were exhibited by some of the reviewed papers [29, 55].
The twenty, fifteen, ten, seven and a half, five, three and two-year estimated cumulative survival rates of the porcelain PLvs were 89,3%, 88,3%, 89,6%, 93,8%, 97,1%, 97,4% and 91,5% respectively.
CONCLUSION
Debonding, fracture, discoloration of the porcelain, staining or disintegration of tooth-porcelain margin, hypersensitivity, secondary caries, pulp necrosis and the periodontal responses were the more frequently studied failures. The mean CFR was found as 8,22% per study. Enamel substrate, incisal overlapping and lithium disilicate veneers presented lower failure rates than dentine substrate, non-overlapping and feldspathic veneers.
AUTHOR’S CONTRIBUTIONS
The authors contributed equally to this work.
LIST OF ABBREVIATIONS
| PLV | = Partial Laminate Veneer |
| USPHS | = United States Public Health System |
| FDI | = Federation Dentaire International |
| CDA | = California Dental Association |
| CFR | = cumulative Failure Rate |
| BOP | = Bleeding on Probing |
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author [I.C] upon reasonable request.
ACKNOWLEDGEMENTS
Declared none.
SUPPLEMENTARY MATERIAL
PRISMA checklist is available as supplementary material on the publisher’s website along with the published article.
Supplementary material is available on the publisher’s website along with the published article.


