All published articles of this journal are available on ScienceDirect.
Systematic Management of Severe Anterior Tooth Surface Loss using Provisional Onlay and Permanent Overlay Removable Prostheses: A Case Report
Abstract
Background:
Management of severe tooth surface loss presents a growing difficulty that is encountered increasingly in everyday practice. Loss of posterior support has been identified as the causative factor in severe anterior tooth surface loss, leading to a reduction in the occlusal vertical dimension and complex tooth wear, which can affect the quality of life.
Objective:
The purpose of this report is to show the systematic approach utilized in the management of severe anterior tooth surface loss in a partially edentulous old patient.
Case Report:
This report describes the management of a 59-year-old gentleman with a complaint of short anterior teeth as well as inefficient function. Clinical examination revealed short anterior teeth and multiple missing teeth posteriorly, which resulted in the loss of posterior tooth support. The management of this case involved reorganizing the occlusion to create the restorative space, which was achieved by a combination of fixed and removable restorations. The short- and medium-term management consisted of an occlusal splint, endodontic treatment, composite build-ups, provisional onlay acrylic dentures, and metal copings. Single crowns and removable cobalt chrome partial dentures were the definitive treatment for the maxillary arch, while a modified overlay cobalt chrome partial denture with cast facings and custom-made porcelain teeth was fabricated for the mandibular arch.
Results:
The patient was able to function well with the provisional onlay denture, and at the same time, the increased vertical dimension and the patient’s tolerance and compliance to partial denture treatment were evaluated. The permeant overlay partial denture restored the patient’s aesthetics and function, with minor adjustments needed. At the 2-year review appointment, the patient denied experiencing any muscular or temporomandibular joint soreness or dental complaints except for minor sensitivity. The patient was compliant and satisfied with the overall performance of the dentures.
Conclusion:
A systematic approach to the management of a patient with a complex presentation can lead to a predictable and favourable prognosis. Onlay and overlay removable partial dentures are regarded as treatment alternatives that are non-invasive, reversible, and conservative.
1. INTRODUCTION
Old patients who require extensive restorative care may display visible signs of significant wear on their teeth. This may be due to an ageing patient population in which many individuals are retaining more teeth [1]. It is normal for tooth wear to occur as a physiologic process; however, pathologic tooth wear can develop when this normal rate of wear process is accelerated by variables, either internal or external, that are not ordinary [2]. Severe tooth surface loss is defined as a multifactorial, non-carious pathological loss of tooth surface, and it has detrimental effects on the dentition and quality of life of patients [3]. It is essential that the underlying cause of abnormal wear be defined in order to prevent further pathologic changes; however, identifying the factors that are responsible for a severely worn dentition frequently presents a clinical dilemma [4]. Significant anterior attrition and a reduction in the occlusal vertical dimension (OVD) that may result in traumatic anterior occlusion have been associated with loss of posterior support [4]. Bruxism often results in progressively greater wear toward the anterior teeth. A definitive diagnosis may be made by hand-articulating diagnostic casts and matching wear facets. Additional intraoral findings may include grooving of the lateral borders of the tongue and evidence of cheek biting. Cupping or cratering of the occlusal surfaces can occur once the enamel has been damaged [4].
The unfavorable environment must be considered during rehabilitation, and choices must be made to provide the longest possible lifespan for the intervention. The loss of tooth structure can shorten and sharpen the teeth. Although this may or may not alter the OVD, it limits the amount of interocclusal space for future restorations and reduces the patient's aesthetic and functional values [3]. Severely worn teeth cannot always be restored through fixed prosthodontic means. Such cases may be present in combination with long edentulous spans that also require soft tissue replacement [5].
The choice of techniques and materials is clinician- and patient-driven. If the patient has long edentulous spans in addition to highly worn teeth and retained roots, removable overlays, onlays, or overdentures may be feasible solutions for rehabilitating severely worn dentitions [6]. Management in the form of removable dentures can be offered reversibly and with little dental preparation. With several lost posterior teeth and a decreased vertical dimension, a removable denture can rapidly restore aesthetics, the number of occlusal contacts, and function. These dentures are made from polymethyl methacrylate or cobalt chrome framework and acrylic resin, and they have proved their efficiency in managing such cases [5].
When it comes to the space requirement, it is necessary for the metal framework and, later, the prosthetic teeth to have enough space. In cases of limited space, the prosthetic teeth may face the risk of being unsupported and non-retentive [6]. All anterior prosthetic teeth should have metal backings to decrease the incidence of prosthetic failure. Metal occlusal onlays on posterior teeth are recommended in situations where there is limited space, as acrylic occlusal onlays require a minimum of 2 mm of interocclusal space in order to be suitably stiff, but cobalt-chrome occlusal onlays only require 1 mm of space. The acrylic resin might crack and fracture under considerable stress. Thus, a chrome-cobalt framework, which is tougher and more durable, is recommended [7].
Rehabilitation with removable dentures comes with drawbacks; one of the greatest limitations is the patient’s compliance with wearing the denture. This can hugely affect the management’s success. Other drawbacks, such as gag reflexes and poor plaque control, can limit the use of such interventions [6].
Nowadays, revolutionary fabrication technologies, such as three-dimensional (3D) printing and computer-aided design and manufacturing, have changed and will change the way in which treatment is delivered to tooth-wear patients. While traditional techniques have been widely used and have demonstrated satisfactory outcomes, newer techniques, such as intraoral scanners and 3D printing, and materials, such as polyether ether ketone, are gaining popularity [8].
The purpose of this original report is to show the systematic approach utilized in the management of severe anterior tooth surface loss in a partially edentulous old patient. This report provides the reader with a feasible workflow for using provisional onlay and permanent overlay dentures with two-year follow-up results.
2. CASE REPORT
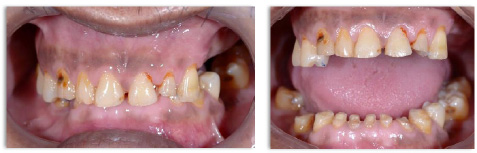
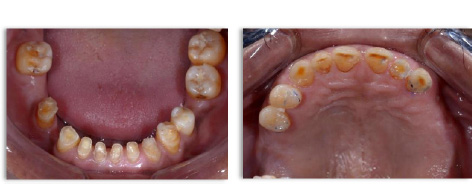
A 59-year-old gentleman came with a complaint of short anterior teeth as well as inefficient function. Additionally, he complained of the sensitivity of a few teeth. The patient requested the denture to masticate normally and for other social reasons. From his history taking, the patient reported that after the extraction of his posterior teeth, his anterior teeth started to become shorter gradually. Neither pain nor discomfort were reported from the temporomandibular joint area. The patient was a symptomatic dental attendee with no history of wearing dentures. Medically, the patient was fit and well. Clinical examination revealed short anterior teeth and multiple missing teeth posteriorly with loss of posterior tooth support (Figs. 1 and 2). Free-way space was 6 mm, and space analyses indicated inadequate interocclusal space to restore the teeth and replace the missing teeth. Sinus tracts with pus were associated with the lower anterior teeth (Fig. 3). In this case, it was assumed that this severe tooth surface loss was caused primarily by attrition due to the loss of posterior support. The patient gave his informed consent to proceed with the treatment.
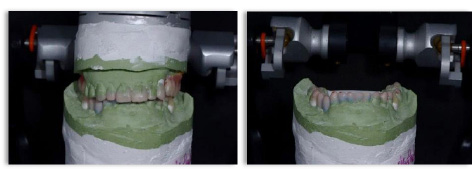
The management of this case involved reorganizing the occlusion achieved by a combination of fixed and removable prostheses. A diagnostic wax-up was done with the casts mounted in centric relation on a semi-adjustable articulator (C.S.A-400-Korea) to aid with the planning of the restorative work (Fig. 4). In this case, the OVD was increased by about 4 mm. The occlusal scheme was based on canine-guided excursions whenever possible and shared incisal protrusion.
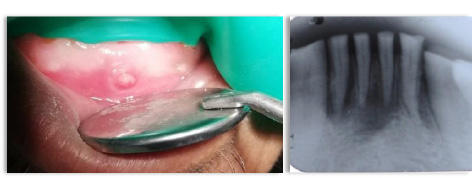
The treatment started with a stabilization phase, which consisted of a Tanner occlusal splint on the lower arch (Fig. 5) and endodontic treatment (Fig. 6). An occlusal splint was used to evaluate the patient’s adaptability to the planned occlusal changes. The patient did not report any discomfort related to this OVD increase.


Composite (Filtek Z350, 3M ESPE, USA) build-ups of the maxillary and mandibular canines and premolars at the planned raised OVD and canine-guided occlusion were done first (Fig. 7). After that and after obtaining final impressions to do the onlay dentures, the maxillary and mandibular incisor teeth were covered with Bisacryl material, Protemp 4 (3M ESPE, Germany) that was injected in the putty index (3M ESPE, USA) which was made from the waxed-up duplicated model. These temporaries were used to restore the function and aesthetics of the anterior teeth and to act as a mock try-in (Fig. 8). After this, dental casts from alginate impressions were made to act as a guide for the technician in building up the onlay denture’s acrylic teeth.


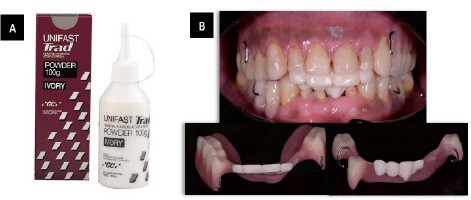
The fabrication of onlay acrylic teeth was done by using Unifast Trad acrylic resin (GC, Japan) (Fig. 9A). After 3 months of wearing the provisional onlay dentures (Fig. 9B), the patient was reassessed. There were no problems, and the patient was satisfied with the increase in OVD, aesthetics, phonetics, and function. A decision was made to remove the onlay teeth from the maxillary denture and do the composite build-ups on teeth 12, 11, 21, and 22 only (Fig. 10).

Due to the COVID-19 pandemic, the patient was not reviewed for a long time. Due to this, there was one fractured composite and wear and staining of multiple composite build-ups (Fig. 11). However, the patient was satisfied, and no complaints were recorded. The teeth and restorations were polished, and full-mouth prophylaxis was done for the patient.

Cast posts and metal copings for teeth 33, 32, 41, and 42 were done (Fig. 12). The fit was acceptable after a few adjustments were made with the help of Fit Checker (GC, Japan) and Arti Spot (Bausch®, Germany). The metal copings were cemented using dual-cure ParaCore cement (Coltene, Germany) (Fig. 12). The lower onlay denture was adjusted to ensure a good fit over the metal copings.

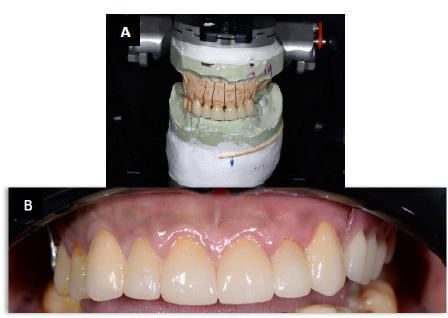

In the definitive stage, anterior single crowns were fabricated with the aid of a facebow and semi-adjustable articulator (Fig. 13A). The crowns were cemented with RelyX Ultimate Clicker (3M ESPE, Germany) (Fig. 13B).
After the cementation procedure, final impressions of the maxillary and mandibular arches were made by a one-stage double mix impression technique by using a special tray with light and heavy body polyvinyl siloxane impression material, EXAMIX™ NDS (GC, Japan). The maxillary and mandibular metal frameworks were then fabricated by the technician following the design drawn on the instruction card. The mandibular framework was tried inside the patient’s mouth, as shown in (Fig. 14). The removable cobalt chrome partial dentures (Co-Cr PDs) were the definitive treatment for the maxillary arch, while a modified cast-facing overlay type Co-Cr PD with custom-made porcelain teeth was fabricated for the mandibular arch (Fig. 15). These dentures were prescribed for all-day use only and were to be taken out before sleep. There were follow-up visits at 1, 4, and 6 weeks after the delivery visit, and then follow-ups after six months and yearly (Fig. 16). There were slight adjustments at each check-up. The patient denied experiencing any muscular or temporomandibular joint soreness and reported that he was satisfied with the overall performance of the denture.


3. DISCUSSION
Pathologically severe tooth surface loss due to several causes other than caries can have serious consequences for a person's dentition and overall quality of life [3]. In this case, it was assumed that this severe tooth surface loss was caused primarily by attrition due to the loss of posterior support. The elements of erosion and abrasion were also assumed to be part of the causing factors that led to this disease level.
The management of this case involved reorganizing the occlusion. The reorganized approach was chosen in this case as it can increase the restorative space, and the occlusal scheme can be achieved based on canine-guided excursions whenever possible and shared incisal protrusion. Patients who have canine-guided occlusion would have a healthier periodontium with less tooth surface loss compared to patients with group function occlusion [9].
OVD was raised by a combination of fixed and removable restorations. The degree of raised OVD should be chosen based on the dental restorative and aesthetic requirements. In most cases, a minimal rise in OVD should be performed; nevertheless, a maximum increase in OVD of 5 mm may be justified in order to give an appropriate occlusal space for the restorative material and to enhance the aesthetic value of the anterior teeth [10]. In this case, the OVD was increased by about 4 mm, and the patient did not report any discomfort related to this increase. An occlusal splint and onlay dentures were used to evaluate the patient’s adaptability to the planned occlusal changes.
Direct composite build-ups are relatively simple to place, have an acceptable aesthetic outcome, and are predictable. The universal composite was chosen for its aesthetics and strength, and it will be easy to repair and reversible [11]. It also has an accelerated wear rate compared to metal/ceramic and potentially inadequate wear resistance for posterior use [12]. The survival rates of anterior composites (direct or indirect) were >90% and 50% at 2.5 years and 5 years, respectively. However, evidence on long-term outcomes remains limited [3]. If the composite build-up fails due to fracture, other options, such as extra coronal restorations in the form of a full-coverage crown, should be considered.
Emax monolithic ceramic crowns were chosen because Emax is a highly durable and very strong ceramic that can overcome some porcelain chipping problems encountered commonly in zirconia or PBM crowns [13]. In terms of survival rate, most types of all ceramic single crowns (SCs) were similar to those reported for PBM SCs. Lithium disilicate SCs have a survival rate of 94.9% for 5 years [14].
Post and core build-ups of teeth 33, 32, 41, and 42 were not done because of the absence of an adequate ferrule and due to short roots. Therefore, it was decided to prosthetically rehabilitate the patient by utilizing the teeth as overlay or onlay abutments. It was decided to place copings over the overlay abutments to prevent further decay, and the patient was instructed to take care of his oral hygiene together with periodic fluoride application to avoid the development of caries [15]. In the periapical radiograph (Fig. 12), there was a gap of less than 2 mm between the post and gutta-percha of teeth 33 and 32. This gap was studied by Moshonov et al., 2005, and they found that a gap of less than 2 mm had a satisfactory outcome of 53.6% up to 5 years [16].
Severely worn teeth cannot always be restored through fixed prosthodontic means. Such cases may be present in combination with long edentulous spans that also require soft tissue replacement. Onlay and overlay removable prostheses (ORP) are subsets of overdentures and can be used in the management of missing posterior teeth and tooth wear. An onlay denture is a denture that covers the occlusal or incisal surfaces of the abutment teeth, while an overlay denture is a denture that covers the worn teeth with a full labial veneer facing [17]. ORP can be utilised in the role of provisional dentures for evaluating changes in the occlusal vertical dimension, as well as aesthetics, phonetics, and function. When a patient has significant tooth wear and limited financial resources, these ORPs can be used either as an interim or permanent solution [17].
There are alternative prosthetic options available to replace missing teeth, such as replacement with an implant-supported removable or fixed denture. Multiple factors should be considered in choosing a treatment plan. Periodontal, biomechanical, aesthetic, financial, and the patient’s wishes are the most critical factors [9]. Despite the fact that the survival rate of an implant-supported denture is higher compared to a removable partial denture [18, 19], with fewer adverse effects on the remaining dentition, the removable partial denture was chosen due to financial restraints and the patient’s wishes.
Onlay partial dentures are an option to consider when there is between one-third and one-half of the coronal tooth present and the remaining tooth tissue is in good health and aesthetically pleasing. On the other hand, overlay dentures are recommended when there are between one-third and one-half of the coronal teeth present, but the aesthetics of the abutment teeth are unsatisfactory [20].
ORPs are regarded as treatment alternatives that are non-invasive, reversible, and conservative [5]. In comparison with conventional dentures, they provide superior retention, stability, and support, in addition to a decreased rate of alveolar bone resorption. When compared to the expense of a fixed prosthesis, the cost of these dentures is significantly lower, and they also need less chair time and are easier to repair. In terms of the drawback, these dentures are linked to reduced aesthetics, an increased chance of acquiring caries and periodontal disorders, as well as an increased danger of losing tooth vitality. Overlay and onlay dentures’ teeth may wear, fracture, debond, or discolour [20].
Proper oral hygiene reinforcement combined with regular dental follow-up may improve the prognosis of this treatment option [21]. Despite all challenges and limitations, the treatment was considered successful, and the patient was satisfied with the outcomes.
CONCLUSION
A key element for successful rehabilitation is to identify the aetiology and determine the proper sequence of treatment. A systematic approach in the management of a patient with a complex presentation can lead to a predictable and favourable prognosis. Despite all challenges and limitations, the treatment for this case was considered successful, and the patient was satisfied with the outcomes.
AUTHORS’ CONTRIBUTIONS
MA contributed to the conceptualization of the study, collection of the material, did the treatment procedures, designed the graphical part of the manuscript, and wrote the manuscript; AIA wrote the manuscript; YJ and AH took part in the conceptualization of the study; AA conceptualized the study and provided her final approval for the version of the manuscript to be published.
LIST OF ABBREVIATIONS
| OVD | = Occlusal vertical dimension |
| SCs | = Single crowns |
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
The participant involved in this study provided his written informed consent.
FUNDING
This work was fully funded by the Fundamental Research Grant Scheme (FRGS/1/2022/SKK0/USM/01/3) under Ministry of Higher Education, Malaysia.
ACKNOWLEDGEMENTS
The authors are thankful for all efforts done by the laboratory technicians and dental assistants.


