Dental Implant Treatment in Medically Compromised Patients: A Narrative Review
Abstract
Background:
In terms of health treatment and subjects, dental implants have evolved as a standard therapy to solve different complications regarding the retention and stability of dentures for edentulous patients. Although dental implant techniques have been utilized in medically compromised patients, scientific evidence is unclear on the feasibility of implants among these patients. Adequate planning and precautions should be exercised as risks are enhanced among these patients.
Objective:
The primary objective of this work was to provide a brief overview of contraindications, precautions, and guidelines for the use of dental implants among medically compromised patients.
Methodology:
A literature search was performed for published articles within the range 2011-2021 published in English in PubMed, Medline, and OVID Medline databases using the terms Dental Implants, medically compromised patients, treatment plan, and implant survival.
Results:
A total of 23 studies were assessed. There are several studies that have mentioned radiotherapy as a critical risk factor “associated with the frequency of dental implant loss.” On the other hand, it has illustrated that metabolic changes have mainly occurred in diabetic patients. It has been determined that implant survival can be lower in a few disorders. Additionally, risks and complications among medically compromised patients have been noted.
Conclusion:
The study suggests that the psychosocial and functional benefits of an “implant restoration ” are the documented relative risks related to the common medical condition as well as their respective treatments. The assessment of the overall risk factors with the patient's education about the risk needs to be done in order to make perfect intervention strategies.
1. INTRODUCTION
Before 2000 BC, pre-versions of dental implants were utilized in the civilization of Ancient China. At that time, carved bamboo pegs were used to replace the missing teeth. In the 18th century, gold along with alloys, was used to make structures similar to dental implants. In 1952, the first popular modern dental implants were made with titanium (Ti) basins encapsulated in rabbit bone [1]. Another study by Raikar et al. [2] states that a dental implant is a surgical component that interfaces with the bone of the jaw or skull to support a dental prosthesis, such as a crown, bridge, denture, facial prosthesis or to act as an orthodontic anchor. In dentistry, dental implants have been considered one of the most advanced ways of dental prosthodontic rehabilitation, achieving a high long-term success rate. This is one of the latest available therapies for the replacement of missing teeth. Implant survival is initially dependent on successful osseointegration following placement. Any alteration of this biological process may adversely affect treatment outcome, as stated by Naujokat et al. [3]. In the future, dental implants can be more effective as a treatment for “replacing missing teeth” by including innovative technologies like stem cell research and nanotechnology in implant dentistry. Emerging stem cell technologies and the requirements of alveolar ridge augmentation associated with implant dentistry have expanded the clinical concept to include stem-cell-based regeneration [4].
Dental implants are mainly utilized to replace missing teeth. Dental implants provide several advantages, including ensuring that the masticatory forces are transferred to the alveolar process. Dental implants also enhance the quality of life of the individual [5]. However, certain risks and complications are associated with the placement of dental implants, Bozier et al. [6] reported that the nasal cavity and maxillary sinus lie in close proximity to the alveolar bone around teeth in the maxilla. This makes the nasal cavity and maxillary sinus prone to get perforated during the placement of dental implants. Drills used in Implant therapy can easily penetrate the sinus and cause possible infection and sinus disruption. Additionally, there is a possibility of nerve damage in the mandible [6, 7]. Dental implants fail to undergo osseointegration in certain medically compromised conditions. Increased precaution and care must be exercised by the clinician and patients during implant placement in medically compromised patients. Hence, necessary care and precautions need to be exercised following implant placement. The patients should use an interdental brush to clean implant areas and prohibit plaque deposits. Smoking should be prohibited as it would impair the healing of the implant site. The follow-up visit for the second stage of implant surgery should be between 4 to 6 months [8].
The most prevalent age for dental implants is 35 years to 60 years. This age group has a higher chance of associated systemic comorbidities. All systemic comorbidities should be diagnosed prior to initiating the implant procedure [9]. In terms of the medically compromised, the treatment plan should be made with precision with an informed consent of the patient with the risks and precautions associated with the implant surgery [9, 10].
The purpose of this paper was to properly review different medical diseases that reportedly preclude effective dental implant treatment. The primary objective of this paper was to gather information from various published articles on the use of dental implants in medically compromised patients.
2. MATERIALS AND METHODS
2.1. Research Design
An internet search using search engines- Google, Research Gate and PubMed, PubMed Central was carried out. The keywords used for the search were dental implants, medically compromised patients, periodontal diseases, and peri-implantitis. Articles ranging from the duration of ten years from the year 2011–2021 were collected. Articles in the English language with full text available were included for tabular review (Table 1).
The clinical trial, meta-analysis, monocentric study, retro prospective study, cohort study, control and case study, cross-sectional study and case study types were considered for the tabular review. In vitro studies were not included in the analysis.
| Name of Disease | Guidelines | Indication | Contraindication | Precaution |
|---|---|---|---|---|
| Endocrine Disease | ||||
| Diabetes | Avoiding instant loading of the implants | Very safe therapy for the controlled diabetic patient | Slightly higher rate of failure compared to the patient without Diabetes | -Patient should bring the glucometer-Eat everyday meals as per the prescriptions |
| Cardiovascular Disease | ||||
| -Myocardial infarction-Angina-Endocarditis-Replacement of prosthetic valve | Avoid the place with a prosthetic valve to skip endocarditis and other issues | There is a long-term success of dental implants with controlled cardiovascular disease. This therapy will not disrupt the long-term anticoagulant treatment | Cardiovascular disease has no direct contraindication, but the infection will occur. Proper care and prescribed antibiotics should be taken at the right time | The palace if dental implants should be avoided through the latest MI/CVA care till six months of primary care |
| Thyroid | ||||
| Hyperthyroidism | The utilization of epinephrine needs to be avoided. | The survival rates of different medically compromised patients with hypothyroidism indicate a massive success rate for the placement of dental implants. | This therapy will make the patient most sensitive to sympathomimetic drugs like epinephrine. | If the patient has any symptoms of thyrotoxicosis, then dental implants should be delayed. |
| COPD Asthma | The patient with COPD asthma needs to receive prophylactic attention | If the therapy is processed with proper precautions, then the patient will improve self-esteem and oral health. | There is a huge chance of increasing dental erosion risks. There is a higher risk of a heart attack in a week. | Patients should rinse their mouth after utilizing a steroid inhaler in order to decrease the critical incidents oforal candidiasis. |
| AIDS | If the person does not have sufficient structure for the dental implants, then there is no way for this therapy. | This therapy is quite suitable for the rehabilitation of HIV-positive patients with the most controlled risk factors as well as “CD4+ cell counts”. | The average marginal loss of bone is 0.83 mm at the HIV patient level, whereas 0.99mm at the implant level, but this is not a contraindication. | The dentist should wear PPE kits, hand engines and sharp disinfectant objects. |
| Osteoporosis | Dental implants will be easily performed along with a predictable prognosis with “osteoporosis: patient under specific oral bisphosphonates | Research has shown that patients with osteoporosis do not visualize any significant risk for the dental implant | Patients with this disease are not contraindicated for this therapy but can affect the jawbone. | After a dental implant, the patient should adequately follow the medication. Doctors should determine the patient's metabolic rate before initiating. |
| Radiotherapy in cancer patients. | The dental implant process should be taken after six months of radiotherapy. It should be taken before radiotherapy | It is highly needed before radiotherapy due to the osteonecrosis risks in irradiated fields. | It has no direct contraindication but can be affected by radiotherapy if placed in the maxilla. | Oral surgery needs to be performed before initiating the therapy |
| Bleeding disorder | The dentist should determine the bleeding disorder properly and understand it | Significantly less loss of the mass of jawbones. | There is no proper evidence to prove that the bleeding disorder is a contraindication to dental implant therapy. | The patient should continue to bite down firmly on gauze sponges, applying little pressure by biting down on the gauge. |
| Hypertension | The uncontrolled hypertension is 180/110 or more than this. This guideline should be followed | There is no way to perform dental implants without stabilized blood pressure. It is impossible to initiate this therapy with a high blood pressure of more than 180 diastolic blood pressure. | If the patient has high blood pressure, the patient tends to work hard. In this situation, the dental implants will be more complicated by anxiety. | Hypertension medication should be provided before taking medical implantation. |
| Pregnancy | It is quite safe if used after the first trimester. It will be better after delivery. | Changes in the immune system, as well as gestational Diabetes and inflammation in gums, can contribute to the optimum rate of a dental implant. | There's no direct contraindication, but it is unethical to conduct therapy during pregnancy. | Instruction of oral hygiene, polishing and plaque control needs to be performed essentially. |
| Parathyroid disease | In this situation, dental implants can be performed without the procedure of lengthy grafting. | Implant in the mandible has a higher success rate rather than in the maxilla. | Tartar development at the implant site can cause irritation in gum tissue through the toxin-emitting bacteria. | The patient should follow the medication after completing the dental implant. |
| Chemotherapy | Dentists should determine the stability of the bone because weak bone can fail the therapy. | This will help to feel the tooth and jaw because chemotherapy can disrupt this tissue. | A jawbone can grow back, but it may still have very little density, completely unable to hold the implant accurately. | The patient should rinse their mouth with “0.12% chlorhexidine and check-up”. |
2.2. Inclusion Criteria
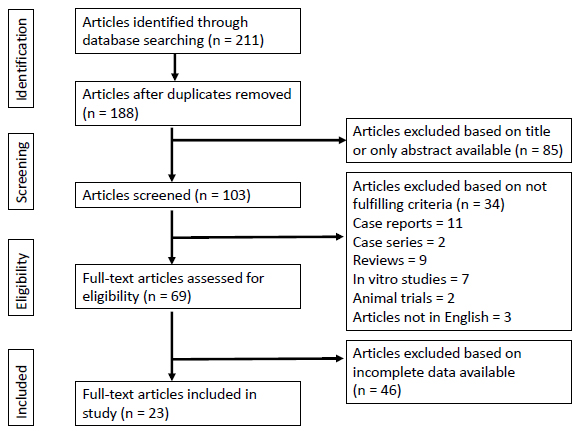
Articles ranging from the duration of ten years from the year 2011–2021 were collected, which included only published articles on the use of dental implants in medically compromised patients (Fig. 1).
2.3. Exclusion Criteria
Studies and articles for which full text was unavailable or articles published in a language other than English were excluded.
2.4. Expected Outcome
This research work was expected to summarize the recent updates of precautions to be considered when deciding to provide dental implant treatment for medically compromised patients. This may help clinicians to select the best treatment option to minimize the failure rate of dental implants for those patients and maximize the rate of success of the implant.
3. RESULTS
It has been seen that different authors have studied different medical disorders (Table 2) that are relevant in implant dentistry, as described in Table 1. Based on this perspective, all of the included studies were identified and addressed in the below mentioned (Table 2). The Table 2 addressed the result of different studies that used samples and processes to install dental implant with different diseases, as described by Ata-Ali et al. [11-38].
The results selected are based on different papers. There are several studies that have mentioned radiotherapy as a critical risk factor “associated with the frequency of dental implant loss.” This particular treatment involves ionizing radiation and is very reliable for explaining the relation between dental implant loss and radiotherapy while placed over the “oral cavity.”
| No. of Studies | Author/Refs. | Year | Type of Study | No of Patients | Outcomes |
|---|---|---|---|---|---|
| 1 | Claudy et al. [18] | 2015 | Meta-Analysis | A total of 1814 patients were considered | There is a negative relationship between radiotherapy and dental implant |
| 2 | Smith Nobrega et al. [19] | 2016 | Meta-Analysis | 2220 participants and 9231 dental implants were considered | Dental implant areas in irradiated parts of an oral cavity have an optimum survival rate with strict monitoring of patients. |
| 3 | May et al. [21] | 2016 | Prospective cohort study | 16 adults | 10% failure rates have been determined with dental implants in AIDS healthy patient |
| 4 | Oliveira et al. [22] | 2020 | Case study with long followup | 18 patients | Dental implant treatment in HIV-positive patients achieved long-term survival, with a success rate comparable with that observed in healthy patients, indicating that implant rehabilitation is not a contraindication for HIV-positive patients. |
| 5 | Gay-Escoda et al. [23] | 2016 | Retrospective Study | 9 subjects | Oral rehabilitation with dental implants in HIV-positive patients “seems to provide satisfactory results” by maintaining strict maintenance |
| 6 | Rubinstein et al. [35] | 2019 | Retrospective Study | 67 HIV positive patients | The result of this study has suggested that dental implants in HIV patients are effective and safe. |
| 7 | Schimmel et al. [27] | 2018 | Meta-Analysis | 600 articles | Dental implants can be placed in aged patients except the osteoporosis and dementia disease |
| 8 | Akel [12] | 2019 | Meta-Analysis | Sample range was 32 to 127 | The failure rate of dental implants with parathyroid is maximum in smoker participants |
| 9 | Parihar et al. [13] | 2020 | Retrospective Study | 68 | Dental implant procedure with hypothyroidism has a negative influence on the success of dental implants |
| 10 | Sánchez-Martos et al. [37] | 2020 | Meta Analysis | Total 721 patient254 women and467 men | Use of diode laser in dental implants is effective in reducing clinical signs of peri-implant mucositis |
| 11 | Al Ansari et al. [14] | 2022 | Meta-Analysis | Total l5510 participantsSample range was n=3 to n=80 | Implant in diabetic patients has shown a significant risk of failure and massive marginal bone loss |
| 12 | Esposito et al. [38] | 2013 | Meta-Analysis | 1162 | No significant adverse consequence is reported in pregnant women |
| 13 | Wu et al. [28] | 2016 | Cohort Study | 728 patients | Treatment with antihypertensive drugs can be associated with the increased survival rate of osseointegration plant |
| 14 | Chrcanovic et al. [17] | 2017 | Meta-Analysis | Unspecified | Patients estimated with an increasing implant failure rate |
| 16 | Seki et al. [29] | 2020 | Case Study with Control Groups | 35 patients receiving a total of 77 dental implants with a medical history of anxiety-related disorders. | A 7 yearlong follow study and antihypertensive prescriptions have helped in better situations to be developed. A significant difference was observed while measuring the implant depth for hypertensive patients in comparison to the control group. |
| 17 | Gargallo-Albiol et al. [36] | 2021 | Cross-Sectional Study | 31 patients with 45 implants | Peri-implantitis is the major cause of IR |
| 18 | Malm et al. [34] | 2021 | Primary Case Study | Implant failure was observed within a group of 408 individuals, tallied against the same number of control cases | COPD and asthma related disorders are positively and significantly correlated with dental hygiene, and implant failures are related to the presence of smoking habits. |
| 19 | Neetemu et al. [31], | 2021 | Cross-Sectional Study | 80 patients with 119 implants to study for bleeding on probing into the gum and jawbone | 42 implant probing showed a significant amount of bleeding behaviour, and peri-implant gingivitis |
4. DISCUSSION
4.1. Radiotherapy and Irradiated Bone
An elaborate analysis of dental implants in medically compromised patients have been described by authors, such as Caccianiga et al. [16]; they stated that radiotherapy and smoking both are directly integrated, which results in an increased chance of “dental implant failure”. This author has argued that further study is needed for the identification of the relationship between osteoporosis and diabetes as well as the chance of implant failure. Opinions of the authors Chrcanovic et al. [17] and Claudy et al. [18] stated a comparable implant survival between the irradiative native bone and non-irradiative native bone. It has been determined that soft tissue around the implant plays a crucial role in the success of the implant as well as “long-term periodontal health” is directly associated with the keratinised gingiva. Smith Nobregga et al. [19] stated that dental implant areas in irradiated parts of an oral cavity have an optimum survival rate with strict monitoring of patients.
4.2. HIV and/or AIDS
Shivakumar et al. [20] conducted a systematic review to determine the impact HIV has on dental implants. They concluded that HIV infection does not pose a serious threat to implant survival on short-term evaluation. The osteoporotic subjects presented massive rates of implant loss, and there is lower evidence to prove that osteoporosis has “detrimental impacts on bone healing.” May et al. [21], had conducted a prospective cohort study to determine the success of dental implant rate in patients having AIDS in comparison with widely accepted rates of failure in healthy patients at 5-7%. Oliveria et al. [22] Radiographs obtained at 6 months, 12 months, and 12 years of functional loading showed mean (SD) marginal bone losses of 0.32 (0.23) mm, 0.37 (0.23) mm, and 2.43 (1.48), respectively.
Gay-Escoda et al. [23] identified that “oral rehabilitation with dental implant therapy” in
HIV patients tends to provide effective results. The authors Lemos et al. [24] have identified from the result that “marginal bone loss was 0.83 nm” at the “patient level as well as 0.99 at the implant level”. From this data, the authors have stated that “dental implants” are perfect for the “rehabilitation of HIV patients” with strict maintenance of “different risk factors and normal CD4+ cell counts”. The author Duttenhoefer [9] has claimed that dental implants are very safe and predictable procedures for “dental rehabilitation” in an immunocom-promised patient.
4.3. Diabetes
Oslon et al. [25] evaluated that diabetic patients had shown a massive chance of failure along with marginal bone loss in contrast to the installed implant in nondiabetic patients. It is identified that the higher risk of failure in diabetic patients as well as glycaemic control, can improve the success of osseointegration in the implants. It has been seen that bone remodelling around the implant is very low as well as quite less effective in diabetic and cardiovascular patients, but the patients having diabetes have a steady rate of bone remodelling. Their study supports the use of dental implants in type 2 diabetic patients. The overall survival rate of the implant in diabetes is not different from the survival rate in healthy individuals within the first 6 years.
4.4. Thyroid Disorders
The researchers Torrejon-Moya et al. [26] conducted a “systematic review and meta-analysis” in order to determine whether Patients with Thyroid Disorder have a Contraindication for Dental Implants. This study concluded that patients with thyroid disorders could be rehabilitated with dental implants, with similar survival rates as patients without thyroid disorders.
4.5. Hypertension and Related Disorders
Schimmel et al. [27] have identified the impact of a dental implant on the patient having antihypertensive medication. The finding of this study suggested that treatment with “antihypertensive drugs” can be associated with an enhanced survival date of osseointegrated implants. Authors Wu et al. [28] have documented that the lifetime incidence of epistaxis in both maxillofacial and dental practice can be considered as high as 60%. This situation can be created by the placement of dental implants. This study has stated that for patients with “bleeding disorders like vascular defects,” it is significant to properly reinforce hemostasis at the time of maxillofacial or dental surgery by utilising “local measures depending on the mechanical compression and hemostatic agent.” Seki et al. [29] conducted a “retrospective cohort study” to determine the influence of antihypertensive medication on dental implants. The result of these studies showed little correlation between the utilisation of “antihypertensive medication” and several clinical parameters in “anodised peri-implant tissue.” Study by Fabris et al. revealed that the histological appearance of bone derived from hypertensive patients was normal [30].
4.6. Respiratory Diseases
Chen et al. [5] performed a randomised control trial to evaluate the association of dental cleaning with decreased risk of COPD. This study identified that “advanced dental cleaning” is associated with a decreased “frequency of COPD exacerbations.” The study focussed on evaluating the relation between “peri-implant on probing in peri-implant disease” as well as its relation with different multilevel factors.” This study showed the significant association between “gingival recession and thin gingival biotype” along with peri-implant BoP.
4.7. Other Conditions
Nettemu et al. [31] identified the impact of diode laser therapy in peri-implant mucositis through systematic review and meta-analysis. The results of this study have shown that using od diode lasers has promising “results in the treatment of peri-implant mucositis.” Giro et al [32]. stated that osteoporotic patients presented higher rates of implant loss; however, there is lower evidence to strengthen or refute the hypothesis that osteoporosis may have detrimental effects on bone healing. De Medeiros [33] stated there was no difference in implant survival rate between patients with and without osteoporosis, either at the implant or patient levels.
This study had some limitations. There is a small number of articles on HIV. This was the major limitation in evaluating the impact of the HIV-positive patient on a dental implant. The main aim of this study was to determine “the dental implant in medically compromised patients,” but the heterogeneity of the studies in relation to the implants utilised and follow-up period. Another limitation is that this review has collected lower levels of evidence instead of randomised control trials. The lack of randomised control trials shows that this review is based on limited evidence. Collecting data for 10 different diseases and peri-implant processes was not easy, and there were few diseases with very insufficient data. Insufficient data on different diseases has made the data collection process very complicated.
In the future, randomised control trials based on the selected topics are required to achieve “a better understanding of the underlying relationship among different risk factors.” It can be recommended that “patients with a history of radiation in the neck and head” can be properly treated with dental implants. The patient and the clinician should be aware of the potential risks and other issues relevant to “implant therapy” in the irradiated patient in order to provide a predictable and safe treatment. The psychosocial and functional benefits of an “implant restoration” are the documented relative risks related to the common medical condition as well as their respective treatments. Recent surface treatment can show a massive improvement in bone-implant contact. In addition, one surface modification is more adequate than another as it creates a comparatively marginal bone loss. The assessment of the overall risk factors with the patient's education about the risk needs to be done in order to make perfect intervention strategies.
CONCLUSION
From the comprehensive study, it can be concluded that the success rate of dental implants in “medically compromised patients” is different. This rate of success and failure varied in different experiments by different authors. It has been determined that it is impossible to make any effective conclusion on the impact of “osteoporosis on dental implant therapy.” It has been determined from this study that “dental implants placed in irradiated areas” have a comparatively lower survival rate than in non-irradiated areas. It has been seen that dental implants in “diabetic patients do not differ from the healthy patient” for 6 years, but it can increase the risk of long-term treatment failure in a diabetic patient. As the “AIDS patient reaches the low end of the CD4 spectrum” as well as manifests AIDS, this situation puts the patient in a future immunocompromised patient, enhancing the chance of neoplasia and opportunistic infection. This study has found a positive relationship between periodontitis and hypothyroidism. It has been determined that dental implants in diabetes 1 patients have more chance of failure than type II diabetes. This entire study has shown that the use of medicine can be associated with an optimum survival rate of “dental implants.” Moreover, the potential significance of increasing oral hygiene in the treatment and prevention of COPD has been observed. It has been identified that there is very little evidence to support different influences of “immunodeficient con-ditions” on dental implants' survival rate.
LIST OF ABBREVIATIONS
| HIV | = Human Immunodeficiency Virus |
| COPD | = Chronic Obstructive Pulmonary Disease |
| AIDS | = Acquired Immunodeficiency Syndrome |
ACKNOWLEDGEMENTS
Declared none.


